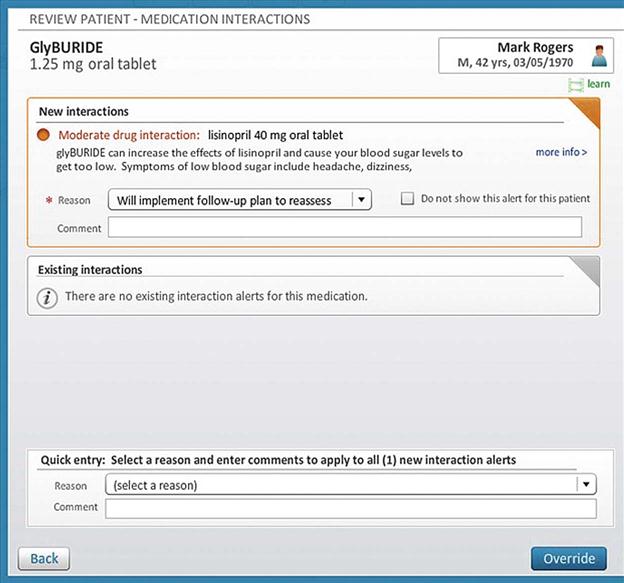
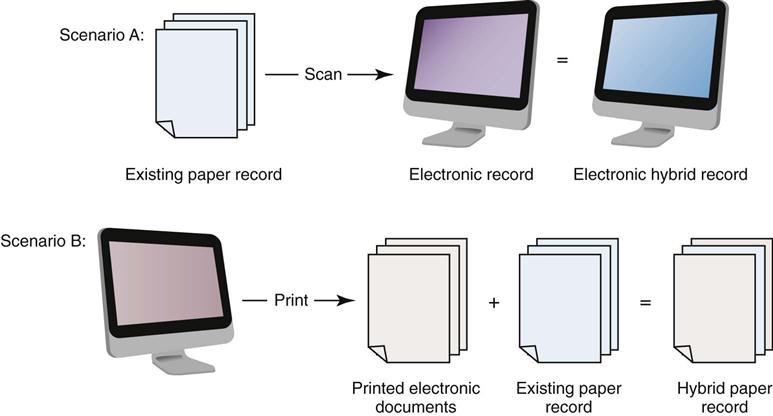
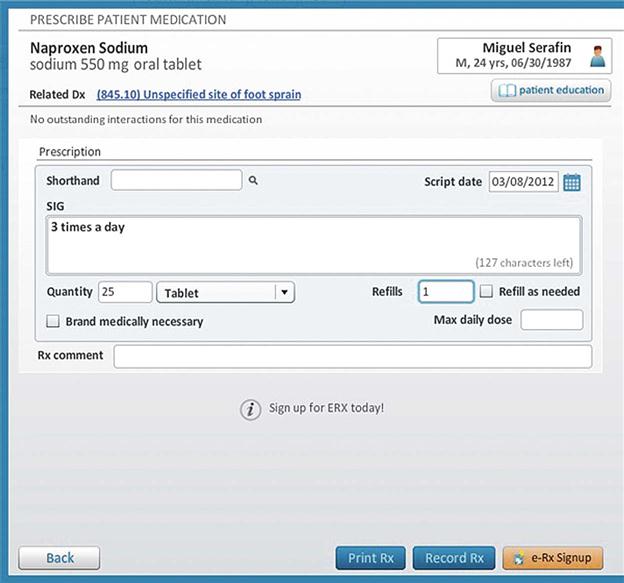
Prerna Dua and Kim Theodos By the end of this chapter, the student should be able to: 1. Define electronic health record. 2. Compare and contrast an electronic health record with a hybrid electronic health record. 3. Identify the advantages of the electronic health record. 5. Explain the history and future of the electronic health record. 6. Discuss meaningful use and its impact on the development of the electronic health record. 7. Identify the challenges and issues associated with implementing the electronic health record. algorithm American Recovery and Reinvestment Act (ARRA) audit trail bar code Certification Commission for Health Information Technology (CCHIT) clinical decision-making system (CDS) clinical pathway computerized physician order entry (CPOE) data repository data warehouse Digital Imaging and Communication in Medicine (DICOM) digital signature document imaging electronic document management system (EDMS) electronic health record (EHR) encryption e-PHI evidence-based decision support evidence-based medicine health information exchange (HIE) Health Information Technology for Economic and Clinical Health Act (HITECH) Health Level Seven (HL7) hybrid record indexing infrastructure integrity interface interoperability longitudinal record meaningful use Nationwide Health Information Network (NHIN) Office of the National Coordinator of Health Information Technology (ONC) picture archiving and communication system (PACS) point-of-care documentation super user workflow Modern health care requires modern technology. For health information professionals, this comes in the form of the electronic health record (EHR). Although traditional paper records still exist in some organizations, significant progress is being made toward transitioning to a completely electronic record. Just as with any other type of major change, health care organizations can be found in many of the various steps and stages of transition. Although some facilities are operating in a fully functional EHR environment, others are in a hybrid phase, in which both paper and electronic mediums are utilized. Historically, this move was championed by health information management (HIM) professionals; however, it has become a focus of the federal government, several of its agencies, and many private consumer groups. This chapter is an introduction to the EHR in all its stages. HIM professionals are facing new responsibilities and new challenges, but their opportunities are greatly expanding. In addition to addressing those changes, this chapter discusses future trends for health care in the electronic exchange of information. As discussed throughout this book, the medical record has been traditionally maintained in a paper format. Each department within a facility may develop a form to document treatment, tests, and other results pertinent to that department’s functions. The paper record is generated at the time of the patient’s admission or encounter and moves with the patient as he or she receives treatment throughout the health care facility. The paper record is assembled after discharge, analyzed, and then filed in the HIM department. A need for increased accessibility and a proven increase in quality of care have led to a trend away from paper records and toward the EHR. One specific scenario highlighting the need for the EHRs occurred during Hurricane Katrina in 2005, when millions of health records were displaced and destroyed, leaving patients without access to their medical records. This made it difficult for the physicians working in disaster medical centers and community hospitals to deliver continued care based on established patient care plans. Responding in part to this disaster, more public and private efforts were initiated, and attention was focused on the development of an EHR system. In a hybrid record, some departments of the hospital use computer information systems to document patient care, but other departments continue to use paper documentation. Recording of clinical data at the time treatment is delivered to the patient is called point-of-care documentation. Some clinical point-of-care documentation may be captured electronically through the system, making data collection into the patient’s health record immediate. Physicians and other health care professionals may capture patient information directly into the health record using several different documentation systems, detailed throughout this chapter. The hybrid record represents a midpoint between the traditional paper record and the fully functional EHR, in which all the documentation surrounding patient care is captured and maintained electronically. There are various degrees of computerization in the hybrid record, ranging from only one department generating electronic reports that make up the patient’s health record to many departments generating electronic reports. Facilities may choose to transition to an EHR in stages by converting the various portions of the health record individually, and most facilities do use the hybrid stage as a step toward a completely EHR. This process may result in a hybrid record with some functions producing electronic data and others remaining paper-based. Managing hybrid records presents unique challenges. Even with a complete electronic point-of-care system, there will still be paper that must be reconciled during downtime or from other organizations, often resulting in scanning or other electronic storage. It can be anticipated that health records will always be in some form of hybrid, and this probability should be acknowledged during development of the system. As stated in Chapter 2, even facilities that rely on paper documentation for their clinical data tend to use computer systems for patient registration data. One example of a hybrid record can be seen during the interfacing (when two independent systems are configured to communicate with each other) between the financial department and the master patient index. The master patient index (MPI) is a major database stored in each facility that houses information about every patient, mostly consisting of demographic information. Although it contains a great deal of information about a patient, it is beneficial for the MPI to be able to gather information from other systems in the hospital as well. The financial system shares information with the MPI, enabling the facility to generate a computerized face sheet or admission record. Utilizing technology in this way is an efficient means of transmitting information between departments and creates an opportunity for further development and interfacing. Because information can be shared, communication between departments is faster, less redundant, and more accurate. Practitioner documentation, consisting of clinical data, makes up a large portion of a traditional medical record. One form of documentation in the record is the transcribed reports, such as the history and physical (H&P), discharge summary, and operative reports. Traditionally, after these reports were dictated (read or spoken aloud and recorded) and transcribed (typed), the HIM department would print and file them in the patient’s chart to be authenticated by the physician. In some hybrid records, these reports are integrated with the computer system and can be signed and stored electronically. In these systems, a digital signature can satisfy the authentication of the medical record, the process whereby the caregiver reads the content of the typed report and signs it, affirming that the content is accurate. Although traditionally done via a handwritten signature, this can be done electronically by clicking a button in the record that indicates “sign the record.” Doing so adds a statement on the document or note indicating that it has been electronically signed by the user. That statement also includes the date and time that the user signed it. Hospitals may take another approach to digital signatures similar to those in retail establishments, where the user signs the name on an electronic signature pad that captures the handwritten signature and adds the image to the document. Ancillary departments, such as laboratory, radiology, and pharmacy, may also use information systems to collect data and generate reports. Their data may be held in a separate database or interfaced with the HIM and/or financial systems. Collectively, these ancillary systems make up a great portion of the health record. Having this information available electronically to multiple users is a great advantage for caregivers, resulting in better quality of care. Physician’s orders are customarily handwritten, although the increased use of hybrid records has encouraged physicians to input this information electronically. A computerized physician order entry (CPOE) system is an application that allows a physician to enter orders for medications, tests, treatments, or procedures into a system. The traditional method of hand writing prescriptions and orders can be difficult, tedious, or even dangerous, and the electronic entry of physician’s instructions for the treatment of the patients reduces potential medical errors. Information portals such as laptops, handheld electronic devices, and mobile computing terminals in the hospitals has made the input of point-of-care information convenient for physicians. The CPOE system provides the physician with a list of medications that can be used for the specific treatment of the patient’s diagnosis. It offers a clinical decision-making system (including but not limited to generic drug ordering, drug interaction information, and laboratory information) that may be needed before the medication is prescribed. The CPOE system provides alerts to the physician based on the patient’s drug list, allergies, interactions, or other potential contraindications. CPOEs are an important part of a fully EHR because they help improve the quality of clinical documentation, allow for more efficient delivery of medications, and reduce excessive and duplicate testing (Dixon, Zafar, 2009). Maintenance of the complete medical record can be a challenge in hybrid records. Facilities with hybrid records may choose to retain part of the record electronically or to print out a paper copy of the computer-based portions, thus creating a paper record. Some facilities transfer or scan the paper-based portion into a digital format using a document imaging system, creating an electronic copy of that information. In document imaging, a scanner converts the paper document into a digital image, which is then stored on a document server, optical disk, or other storage medium. An example is illustrated in Figure 3-1. An electronic document management system (EDMS), such as the one pictured, may be used as a storage and retrieval mechanism and allows for additional documents to be added to an electronic record. For example, an EDMS may be used to scan records transferred from another facility to the EHR. Document imaging can be performed after discharge or at the point of care. As the documents are scanned into the system, the different types of reports are then indexed. Indexing identifies the report by type and organizes them for easier retrieval when needed. It is similar to the plastic tab separators used in the paper records, in that it electronically divides the various sections and indicates in which section the information belongs. Bar coding is a type of automated indexing that is sometimes used to decrease errors and improve productivity in the indexing process. Document scanning and indexing are a solution that makes a paper record or paper portions of a record into electronic images. It proves to be useful especially in a hybrid environment or in an EHR, where it is used to add miscellaneous items and documents. It also allows various functions of the HIM department to be performed electronically, such as coding, analysis, and physician chart completion. In this hybrid record, each sheet of paper contained in the record can be viewed from the computer, but this method does not allow for more in-depth retrieval and use of the data contained in the scanned images. The computer simply recognizes the document as an image rather than recognizing the individual data elements contained in the document. Because individual data elements cannot be added or manipulated electronically, the use of document imaging is limited to storage and access. The challenges associated with managing a hybrid record are substantial. Because portions of the record may be saved as scanned images, locating a specific data element in a document may be difficult. Controlling the various versions of the record is also important to ensure that the most up-to-date version of the record and documentation is stored in all parts of the patient’s record. For example, if a patient changes her address and it is updated in the MPI, that change should be reflected in every system, including anything that has been scanned. The goal is always to have a reliable and accessible patient record, in whichever way that record may be organized or stored. Many facilities have utilized hybrid records as a sensible, affordable solution to make progress toward an EHR. The Health Information Management Systems Society (HIMSS) Electronic Health Record Committee (2003) defines the EHR as follows: “The Electronic Health Record (EHR) is a secure, real-time, point-of-care, patient-centric information resource for clinicians. The EHR aids clinicians’ decision making by providing access to patient health record information where and when they need it and by incorporating evidence-based decision support (the best care results from the conscientious, explicit, and judicious use of current best evidence). The EHR automates and streamlines the clinician’s workflow, closing loops in communication and response that result in delays or gaps in care. The EHR also supports the collection of data for uses other than direct clinical care, such as billing, quality management, outcomes reporting, resource planning, and public health disease surveillance and reporting.” To elaborate the preceding definition, a fully functional EHR incorporates the patient history, demographics, and patient problem lists, list of current medications, and patient’s allergies, as well as physician clinical notes, which include patients’ medical history and follow-up notes. In addition, prescriptions are sent to the pharmacy electronically before being verified for drug interaction, and contraindication warnings are provided. The laboratory and radiology tests are ordered and viewed electronically, with the results being incorporated into the EHR. Further, the out-of-range values for the laboratory tests are highlighted as they are included within the EHR. An EHR results from computer-based data collection. Physicians and other clinicians capture data at the point of care, with the ability to retrieve the data later for reporting and use in research or administrative decision making. Health care workers document via various input ports on the various clinical units, using laptops, handheld computers, and bedside terminals, into templates. Very few, if any, paper reports are generated. The EHR allows all departments (e.g., nursing) to document care electronically using these templates. The electronic record should provide a CPOE. E-prescribing, which allows the electronic transmission of prescription information from physician’s office to the pharmacy—shown in Figure 3-2—is a pronounced feature in EHRs. Other important features included in the EHRs are to send reminders to patients for patient preference or preventive follow-up care, to print out the diagnosis summary and current medication list, to provide patients with timely electronic access to their health information, and to apply evidence-based medicine. Evidence-based medicine (EBM) encompasses clinical expertise, patient values, and latest research available for making a decision in a patient’s care. It helps the physicians understand that a certain treatment will be suitable for the patient and will do him or her more good than harm. The EHR can also provide clinical decision-making algorithms for physician and nonphysician caregivers. An algorithm is a set of step-by-step instructions for solving a problem. An EHR can provide certain prompts or alerts specific to the physician’s orders and provide drug-drug and drug-allergy interaction checks. As shown in Figure 3-3, the EHR prompts the possibility of a moderate drug interaction between the previously prescribed drug, lisinopril, and the newly prescribed drug, glyburide. Wyatt et al (1991) proposed the formal definition of clinical decision-making systems (CDSs) as “active knowledge-making systems which use two or more items of patient data to generate case-specific advice.” Care paths, or clinical pathways, are electronic aids (algorithms) that help caregivers make decisions about treatment. Reference material may be available for electronic use when specific diagnoses are documented. Table 3-1 summarizes the functions of the EHR. TABLE 3-1 FUNCTIONS OF THE ELECTRONIC HEALTH RECORD From Committee on Data Standards for Patient Safety: The National Academic News. http://www.iom.edu/Reports/2003/Key-Capabilities-of-an-Electronic-Health-Record-System.aspx. Accessed July 26, 2012. Since the data in a patient’s EHR can come from many different facilities or sources, in many systems, a data repository is used. The data repository stores data from unrelated software programs. These software programs can be created by different vendors and have different applications. Health care organizations should be able to integrate the data and provide a multidisciplinary view of their elements. A data repository can store the data from these different systems and make them usable through the use of an interface without the need to run reports from each system. For example, data may be collected from three separate software programs and stored in the data repository. Consider a patient who has diabetes: The data repository would store data from the pharmacy software program extracted from the medication administration report indicating the amount of insulin the patient receives. The laboratory software program submits its findings, storing the patient’s glucose levels, and the nursing notes would contain the glucose monitoring results obtained from the nursing flow sheets. This repository data are then collected and reorganized in a data warehouse. Data warehousing facilitates the use of the data in the health records of many individuals by making all this information available for analysis. The data warehouse collects information from different databases and organizes it for use in ad hoc reports and analytical research. Data warehousing is used to make a variety of vital decisions in health care. Stakeholders in the health care industry use this information for analyzing revenue (e.g., to calculate the cost of treating a patient with diabetes) and for clinical management (e.g., to determine the average amount of insulin needed by a patient with diabetes in a specific age group). It has operational applications (e.g., to assess the staffing pattern for patients on a diabetic nursing unit) as well as use in outcome management (e.g., to estimate the percentage of patients who showed improvement after treatment). In a true EHR, data are collected, used, and shared with other all authorized hospital departments and users, as shown in Figure 3-4. The traditional HIM department functions can be performed electronically, either while the patient is still receiving treatment (concurrently) or after discharge (National Institutes of Health, 2006).
Electronic Health Records
Chapter Objectives
Vocabulary
The Evolution of the Electronic Health Record
The Paper Record
The Hybrid Record
The Electronic Health Record
TOPIC
FUNCTION
Health information and data
Allows caregivers to have immediate access to key information such as allergies, medications, and lab test results
Result management
Allows caregivers to quickly access new and past test results, increasing patient safety and effectiveness of care
Order management
Allows caregivers to enter and store orders for prescriptions, tests, or services in a computer-based system that improves legibility, reduces duplication, and increases speed of executing the orders
Decision support
Allows the use of reminders, alerts, and prompts that will improve compliance with best clinical practices, ensure regular screening, and identify possible drug interactions
Electronic communication and connectivity
Allows for efficient, secure, and readily accessible communication among caregivers and patients that will improve the continuity of care, enhance timeliness of diagnoses and treatments, and reduce the frequency of adverse occurrences
Patient support
Provides tools that give patients access to their own health records, provides Internet education, and assists them carrying out home monitoring and self-teaching, which can help improve chronic conditions
Administrative processes
Allows for administrative tools such as scheduling, which would improve efficiency and provide more timely service
Reporting
Allows electronic data storage using uniform data standards that will enable organizations to respond to third-party regulatory agencies

Electronic Health Records
Get Clinical Tree app for offline access