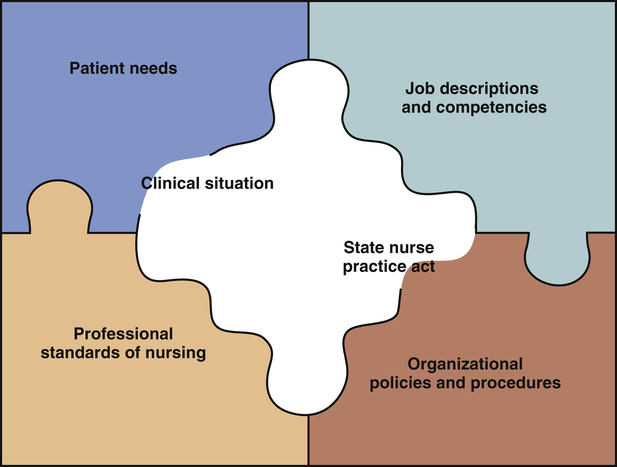
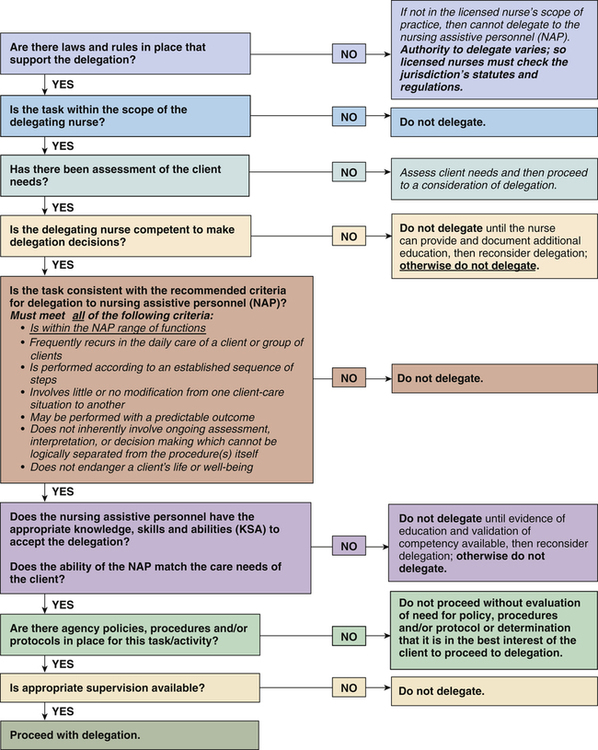
Barbara Cherry, DNSc, MBA, RN, NEA-BC and Margaret Elizabeth Strong, MSN, RN, NE-BC After studying this chapter, the reader will be able to: 1. Evaluate the effect of changes in the current health care system on nurse staffing patterns and responsibilities. 2. Outline six topic areas that the professional nurse should consider when making delegation decisions. 3. List nine essential requirements for safe and effective delegation. 4. Incorporate principles of delegation and supervision in professional nursing practice to ensure safe and legal patient care. In the context of delegation, accountability means bearing responsibility for both the action and inaction of the nurse and those to whom he or she delegates tasks (National Council of State Boards of Nursing [NCSBN], 2005). The distribution of work that each staff member is responsible for during a given work period; when making assignments, the RN supervisor directs a staff member to do something that he or she is authorized to do and is within the staff member’s scope of practice and/or job description (American Nurses Association [ANA] and NCSBN, 2006). The ability of an individual to perform defined behaviors proficiently by demonstrating the appropriate knowledge, skills, attitudes, and professional judgment required for a specific role or setting. Transferring to a competent staff member the authority and responsibility to perform a selected nursing task that the staff member would not normally be allowed to perform; the RN retains accountability for the delegated task (ANA and NCSBN, 2006). Unlicensed assistive personnel (UAP): An unlicensed individual who is trained to function in an assistive role to the RN by performing patient care activities as delegated by the nurse; may include nursing assistants, clinical assistants, orderlies, health aides, or other titles designated within the work setting. The active process of directing, guiding, and influencing the outcome of an individual’s performance of an activity or task (ANA, 2005). Additional resources are available online at: http://evolve.elsevier.com/Cherry/ Vignette 502: Mr. A. is ventilator dependent with an infection that requires IV antibiotics every 12 hours. He needs to be out of bed in a chair twice a day. He has a stage I sacral decubitus ulcer and a PEG tube with bolus feedings. He is very hard of hearing, tries to speak, and becomes very frustrated and uncooperative. 504: Mr. C., age 52, is to be discharged to a rehabilitation hospital today. Discharge records need to be prepared for the transfer. The family is at his bedside and is extremely anxious. 508: Mr. E., age 72, is a ventilator-dependent patient who will start weaning this am. He is on continuous tube feedings and IV antibiotics and needs to be assessed for a PICC line. He is to begin ambulation in the hall twice a day per physician’s orders. He also needs to have a pharyngeal speech evaluation scheduled. 510: Mr. G., age 52, has been off the ventilator for the past 24 hours and is doing very well. He continues on respiratory treatments every 4 hours. His TPN is being decreased, and his PEG feedings are increasing. He has glucose monitoring ordered every 4 hours, an indwelling urinary catheter to gravity drainage, and IV antibiotics every 12 hours. He needs to be out of bed, ambulating in the hall with assistance. If he stays off the ventilator, he will be discharged in 5 days. The family needs to find a nursing home for him; however, the family has not visited Mr. G. since his admission 18 days ago. 511: Mr. H., age 49, is a new admission that will be coming from ICU sometime during the shift. In addition to the tasks mentioned, routine activities of taking vital signs, giving scheduled medications, updating care plans, and answering call lights must be assigned. When reviewing the tasks to be accomplished, Ms. Miller must consider several issues to make safe and effective assignment and delegation decisions. Questions to Consider While Reading This Chapter 1. Which of the above tasks must the RN perform as required by your state’s nurse practice act? 2. Which of the above tasks can be delegated to the nursing assistant? 4. How can other members of the interprofessional health care team contribute most effectively to meet patients’ needs? The issue of health care errors and the RN’s essential role in keeping patients safe was brought to the nation’s attention through the Institute of Medicine’s (IOM) report Keeping Patients Safe: Transforming the Work Environment of Nurses. This report effectively highlights how nurses improve patient outcomes through the ongoing monitoring of patients’ health status, coordinating care, educating patients and families, providing essential therapeutic care, and intercepting health care errors before they can adversely affect patients (IOM, 2004). RNs must learn to delegate nursing tasks safely and effectively so that they will be available to deliver these most important aspects of professional nursing care. In support of the role of UAP in delivering patient care, the Joint Statement on Delegation (ANA and NCSBN, 2006) states, “There is a need and a place for competent, appropriately supervised, unlicensed assistive personnel in the delivery of affordable, quality health care” (p. 2). As health care facilities continue to seek more cost-effective ways to provide care, RNs must learn new ways of managing care and delegating tasks. Delegation is a legal and management concept that involves assessment, planning, intervention, and evaluation. Delegation as defined by the American Nurses Association (ANA, 2005) is “the transfer of responsibility for the performance of an activity from one individual to another while retaining accountability for the outcome” (p. 4). Although RNs can transfer the responsibility and authority for the performance of an activity, they remain accountable for the overall nursing care. When delegating tasks, the nurse should understand the delegatee’s competencies, communicate succinctly, offer clear guidelines in advance, monitor progress, and remain accountable for the final outcomes of care. • Supervising the performance of the delegated task • Assessment and follow-up evaluation • Any intervention or corrective actions that may be required to ensure safe and effective care The delegatee is accountable for the following: • Accepting delegation within the parameters of his or her training and education • Communicating the appropriate information to the delegator Unfortunately there is no easy answer as to what can and cannot be delegated. The answer varies, depending on the (1) nursing practice acts and other applicable state laws, (2) patient needs, (3) job descriptions and competencies of staff members, (4) policies and procedures of the health care organization, (5) clinical situation, and (6) professional standards of nursing practice. To establish a safe, effective delegation practice, the RN must seek guidance and integrate information regarding each of these areas as discussed in the following paragraphs (Figure 19-1). Each state’s nurse practice act provides the legal authority for nursing practice, including delegation. However, each state’s nurse practice act expresses delegation criteria differently, and the criteria often are not clearly spelled out in the act, or they may be presented in various parts of the act. It is absolutely essential that every RN be familiar with his or her state nurse practice act and know the delegation criteria contained within the act. Johnson (1996) has identified 10 essential elements related to delegation criteria in nurse practice acts, as follows: 2. Items that cannot be delegated 3. Items that cannot be routinely delegated 4. Guidelines for the RN about what can be delegated 5. Description of professional nursing practice 6. Description of LPN or LVN and nursing assistive personnel roles 7. Degree of supervision required 8. Guidelines for decreasing the risks associated with delegation 9. Warnings about inappropriate delegation 10. Restricted use of the word nurse to licensed nurses only Although not every state’s nurse practice act contains all 10 elements, the RN can use this list to assist in understanding delegation criteria in his or her own nurse practice act and apply the information to enhance delegation activities. Box 19-1 presents policies common to many nurse practice acts. If the nurse practice act does not provide clear direction regarding delegation, the state board of nursing may be able to offer guidance. The board of nursing may have developed definitions, rulings, advisory opinions, or interpretations of the law to provide guidance regarding delegation activities. Many state boards of nursing may also have practical tools available, such as delegation decision trees or delegation checklists. Figure 19-2 is a delegation decision tree recommended by the NCSBN and provides an excellent framework for the four steps in the delegation process—assessment and planning, communication, surveillance and supervision, and evaluation and feedback.
Effective Delegation and Supervision
Delegation and Supervision in the Health Care System
What is Delegation?
What Should and Should Not be Delegated?
State Nurse Practice Acts
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Nurse Key
Fastest Nurse Insight Engine
Get Clinical Tree app for offline access

