ECGs
Normal ECG
Analyzing the ECG waveform
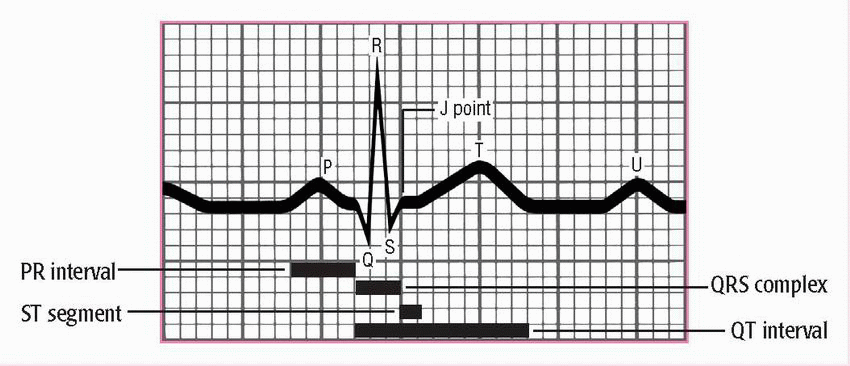
An electrocardiogram (ECG) complex represents the electrical events occurring in one cardiac cycle. A complex consists of five waveforms labeled with the letters P, Q, R, S, and T. The letters Q, R, and S are referred to as a unit known as the QRS complex. The ECG tracing represents the conduction of electrical impulses from the atria to the ventricles. (See Components of an ECG waveform.)
♦ The P wave is the first component of the normal ECG waveform. It represents atrial depolarization.
♦ The PR interval tracks the atrial impulse from the atria through the atrioventricular (AV) node, the bundle of His, and the right and left bundle branches. It begins with atrial depolarization and ends with the beginning of ventricular depolarization.
♦ The QRS complex follows the P wave and represents ventricular depolarization.
♦ The ST segment represents the end of ventricular depolarization and the beginning of ventricular repolarization. The J point marks the end of the QRS complex and the beginning of the ST segment.
♦ The T wave represents ventricular repolarization.
♦ The QT interval measures the time needed for ventricular depolarization and repolarization.
♦ The U wave represents His-Purkinje repolarization.
How to read an ECG rhythm strip: The 8-step method
Analyzing a rhythm strip is a skill that’s developed through practice. You can use several methods, as long as you’re consistent. (See The 8-step method of rhythm strip analysis, pages 150 and 151.)
Normal sinus rhythm
When the heart functions normally, the sinoatrial (SA) node acts as the
primary pacemaker, initiating the electrical impulses. The SA node assumes this role because its automatic firing rate exceeds that of the heart’s other pacemakers, allowing cells to depolarize spontaneously.
primary pacemaker, initiating the electrical impulses. The SA node assumes this role because its automatic firing rate exceeds that of the heart’s other pacemakers, allowing cells to depolarize spontaneously.
The 8-step method of rhythm strip analysis
Rhythm strip analysis requires a sequential and systematic approach. The following eight steps provide a good outline for you to follow.
Step 1: Determine rhythm
To determine the heart’s atrial and ventricular rhythms, use either the pen-andpencil method or the caliper method.
To determine the atrial rhythm, measure the P-P intervals, the intervals between consecutive P waves. These intervals should occur regularly, with only small variations associated with respirations. Then compare the P-P intervals in several cycles. Consistently similar P-P intervals indicate regular atrial rhythm; dissimilar P-P intervals indicate irregular atrial rhythm.
To determine the ventricular rhythm, measure the intervals between two consecutive R waves in the QRS complexes. If an R wave isn’t present, use either Q waves or S waves of consecutive QRS complexes. The R-R intervals should occur regularly. Then compare the R-R intervals in several cycles. As with atrial rhythms, consistently similar intervals mean a regular rhythm; dissimilar intervals point to an irregular rhythm.
After completing your measurements, ask yourself:
♦ Is the rhythm regular or irregular? Consider a rhythm with only slight variations (up to 0.04 second) to be regular.
♦ If the rhythm is irregular, is it slightly irregular or markedly irregular? Does the irregularity occur in a pattern (a regularly irregular pattern)?
Step 2: Calculate rate
You can use one of three methods to determine the atrial and ventricular heart rates from an ECG waveform. Although these methods can provide accurate information, you shouldn’t rely solely on them when assessing your patient. Keep in mind that the ECG waveform represents electrical, not mechanical, activity. Therefore, although an ECG can show that ventricular depolarization has occurred, it doesn’t mean that ventricular contraction has occurred. To determine this, you must evaluate the patient’s pulse.
♦ Times-ten method. The simplest, quickest, and most common way to calculate rate is the times-ten method, especially if the rhythm is irregular. ECG paper is marked in increments of 3 seconds, or 15 large boxes. To calculate the atrial rate, obtain a 6-second strip, count the number of P waves that appear on it, and multiply this number by 10. Ten 6-second strips equal 1 minute. Calculate the ventricular rate the same way, using the R waves.
♦ 1,500 method. If the heart rhythm is regular, use the 1,500 method, so named because 1,500 small squares equal 1 minute. Count the number of small squares between identical points on two consecutive P waves, and then divide 1,500 by that number to determine the atrial rate. To obtain the ventricular rate, use the same method with two consecutive R waves.
♦ Sequence method. The third method of estimating heart rate is the sequence method, which requires memorizing a sequence of numbers. For the atrial rate, find a P wave that peaks on a heavy black line, and assign the following numbers to the next six heavy black lines: 300, 150, 100, 75, 60, and 50. Then find the next P-wave peak and estimate the atrial rate, based on the number assigned to the nearest heavy black line. Estimate the ventricular rate the same way, using the R wave.
Step 3: Evaluate P waves
When examining a rhythm strip for P waves, ask yourself:
♦ Are P waves present?
♦ Do the P waves have a normal configuration?
♦ Do all of the P waves have a similar size and shape?
♦ Is there one P wave for every QRS complex?
Step 4: Determine PR interval duration
To measure the PR interval, count the small squares between the start of the P wave and the start of the QRS complex; then multiply the number of squares by 0.04 second. After you perform this calculation, ask yourself:
♦ Does the duration of the PR interval fall within normal limits, 0.12 to 0.20 second (or 3 to 5 small squares)?
♦ Is the PR interval constant?
Step 5: Determine QRS complex duration
When determining QRS complex duration, make sure to measure straight across from the end of the PR interval to the end of the S wave, not just to the peak. Remember, the QRS complex has no horizontal components. To calculate duration, count the number of small squares between the beginning and the end of the QRS complex and multiply this number by 0.04 second. Then ask yourself the following questions:
♦ Does the duration of the QRS complex fall within normal limits, 0.06 to 0.10 second?
♦ Are all QRS complexes the same size and shape? (If not, measure each one and describe them individually.)
♦ Does a QRS complex appear after every P wave?
Step 6: Evaluate T wave
Examine the T waves on the ECG strip. Then ask yourself:
♦ Are T waves present?
♦ Do all of the T waves have a normal shape?
♦ Could a P wave be hidden in a T wave?
♦ Do all of the T waves have a normal amplitude?
♦ Do the T waves have the same deflection as the QRS complexes?
Step 7: Determine QT interval duration
Count the number of small squares between the beginning of the QRS complex and the end of the T wave, where the T wave returns to the baseline. Multiply this number by 0.04 second. Ask yourself:
♦ Does the duration of the QT interval fall within normal limits, 0.36 to 0.44 second?
Step 8: Evaluate other components
Note the presence of ectopic or aberrantly conducted beats or other abnormalities. Also, check the ST segment for abnormalities and look for the presence of a U wave. Next, interpret your findings by classifying the rhythm strip according to one or all of the following features:
♦ Site of origin of the rhythm. For example, sinus node, atria, atrioventricular node, or ventricles.
♦ Rate. Normal (60 to 100 beats/minute), bradycardia (less than 60 beats/minute), or tachycardia (greater than 100 beats/minute).
♦ Rhythm. Normal or abnormal; for example, flutter, fibrillation, heart block, escape rhythm, or other arrhythmias.
Normal sinus rhythm records an impulse that starts with the sinus node and progresses to the ventricles through a normal conduction pathway —from the sinus node to the atria and AV node, through the bundle of His, to the bundle branches, and onto the Purkinje fibers. Normal sinus rhythm is the standard against which all other rhythms are compared; you must be able to recognize normal sinus rhythm before you can recognize an arrhythmia.
Based on the location of the electrical disturbance, arrhythmias can be classified as sinus, atrial, junctional, or ventricular arrhythmias, or as AV blocks. Functional disturbances in the SA node produce sinus arrhythmias. Enhanced automaticity of atrial tissue or reentry may produce atrial arrhythmias, the most common arrhythmias.
Characteristics of normal sinus rhythm
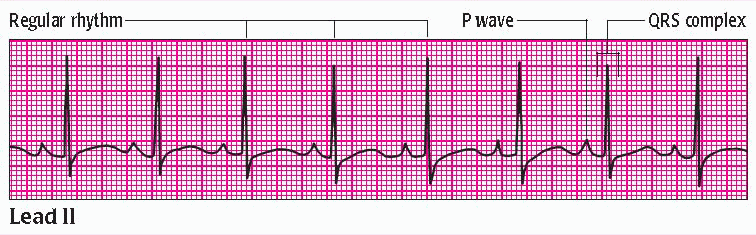 |
Atrial rhythm: regular
Ventricular rhythm: regular
Atrial rate: 60 to 100 beats/minute (80 beats/minute shown)
Ventricular rate: 60 to 100 beats/minute (80 beats/minute shown)
P wave: normally shaped (All P waves have similar size and shape; a P wave precedes each QRS complex.)
PR interval: within normal limits (0.12 to 0.20 second) and constant (0.20-second duration shown)
QRS complex: within normal limits (0.06 to 0.10 second) (All QRS complexes have the same configuration. The duration shown here is 0.12 second.)
T wave: normally shaped; upright and rounded in lead II (Each QRS complex is followed by a T wave.)
QT interval: within normal limits (0.36 to 0.44 second) and constant (0.44-second duration shown)
Junctional arrhythmias originate in the area around the AV node and bundle of His. These arrhythmias usually result from a suppressed higher pacemaker or from blocked impulses at the AV node.
Ventricular arrhythmias originate in ventricular tissue below the bifurcation of the bundle of His. These rhythms may result from reentry or enhanced automaticity or may occur after depolarization.
Arrhythmias
Sinus arrhythmia
In sinus arrhythmia, the heart rate stays within normal limits, but the rhythm is irregular and corresponds to the respiratory cycle and to variations in vagal tone. During inspiration, an increased volume of blood returns to the heart, reducing vagal tone and increasing sinus rate. During expiration, venous return decreases, vagal tone increases, and sinus rate slows.
Characteristics of sinus arrhythmia
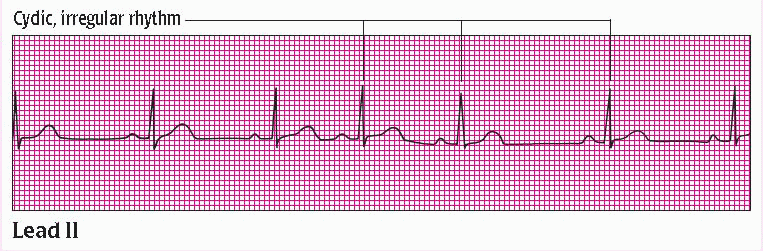 |
Atrial rhythm: irregular, corresponding to the respiratory cycle
Ventricular rhythm: irregular, corresponding to the respiratory cycle
Atrial rate: within normal limits; varies with respiration (60 beats/minute shown)
Ventricular rate: within normal limits; varies with respiration (60 beats/minute shown)
P wave: normal size and configuration (One P wave precedes each QRS complex.)
PR interval: within normal limits (0.16-second, constant interval shown)
QRS complex: normal duration and configuration (0.06-second duration shown)
T wave: normal size and configuration
QT interval: within normal limits (0.36-second interval shown)
Other: phasic slowing and quickening of the rhythm
Conditions unrelated to respiration may also produce sinus arrhythmia. These conditions include inferior wall myocardial infarction (MI) and digoxin toxicity.
Sinus arrhythmia is easily recognized in elderly, pediatric, and sedated patients. The patient’s pulse rate increases with inspiration and decreases with expiration. Usually, the patient is asymptomatic.
Intervention
Treatment isn’t necessary unless the patient is symptomatic or the sinus arrhythmia stems from an underlying cause. If symptoms are associated with symptomatic bradycardia, atropine may be administered.
Sinus bradycardia
Characterized by a sinus rate of less than 60 beats/minute, sinus bradycardia usually occurs as the normal response to a reduced demand for blood flow. It’s common among athletes, whose well-conditioned hearts can maintain stroke volume with reduced effort. It may also be caused by drugs, such as cardiac glycosides, calcium channel blockers, and beta-adrenergic blockers. Sinus bradycardia may occur after an inferior wall MI involving the right coronary artery, which supplies the blood to the SA node. This rhythm may develop during sleep and in patients with increased intracranial pressure. It may also result from vagal stimulation caused by vomiting or defecating. Pathologic sinus bradycardia may occur with sick sinus syndrome.
Characteristics of sinus bradycardia
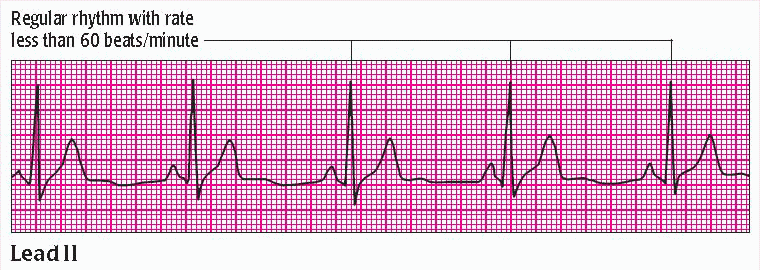 |
Atrial rhythm: regular
Ventricular rhythm: regular
Atrial rate: less than 60 beats/minute (50 beats/minute shown)
Ventricular rate: less than 60 beats/minute (50 beats/minute shown)
P wave: normal size and configuration (One P wave precedes each QRS complex.)
PR interval: within normal limits and constant (0.14-second duration shown)
QRS complex: normal duration and configuration (0.08-second duration shown)
T wave: normal size and configuration
QT interval: within normal limits (0.40-second interval shown)
The patient with sinus bradycardia is asymptomatic if he can compensate for the decrease in heart rate by increasing stroke volume. If he cannot, he may have signs and symptoms of decreased cardiac output, such as hypotension, syncope, confusion, and blurred vision.
Intervention
If the patient is asymptomatic, treatment isn’t necessary. If he has signs and symptoms, the goal of treatment is to identify and correct the underlying cause. The heart rate may be increased with drugs such as atropine. A temporary (transcutaneous or transvenous) or permanent pacemaker may be necessary if bradycardia persists.
Sinus tachycardia
Sinus tachycardia is an acceleration of firing of the SA node beyond its normal discharge rate. In an adult, it’s characterized by a sinus rate of more than 100 beats/minute. The rate rarely exceeds 180 beats/minute except during strenuous exercise. The maximum rate achieved with exercise decreases with age.
A normal response to cellular demands for increased oxygen delivery and blood flow commonly produces sinus tachycardia. Conditions that cause such a demand include heart failure, shock, anemia, exercise, fever, hypoxia, pain, and anxiety. Drugs that stimulate the beta receptors in the heart also cause sinus tachycardia. They include aminophylline, epinephrine, dobutamine, and dopamine. Alcohol, caffeine, and nicotine may also produce sinus tachycardia.
Characteristics of sinus tachycardia
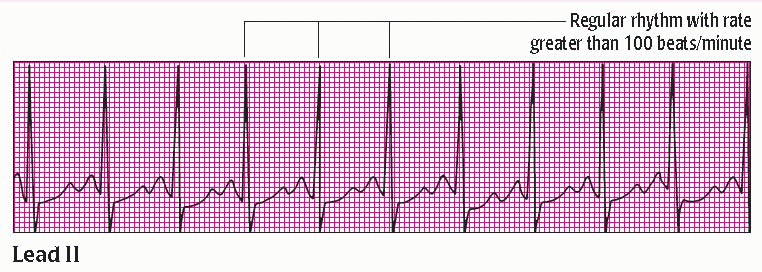 |
Atrial rhythm: regular
Ventricular rhythm: regular
Atrial rate: 100 to 160 beats/minute (110 beats/minute shown)
Ventricular rate: 100 to 160 beats/minute (110 beats/minute shown)
P wave: normal size and configuration (One P wave precedes each QRS complex. As the sinus rate reaches about 150 beats/minute, the P wave merges with the preceding T wave and may be difficult to identify. Examine the descending slope of the preceding T wave closely for notches, indicating presence of the P wave. The P wave shown is normal.)
PR interval: within normal limits and constant (0.16-second duration shown)
QRS complex: normal duration and configuration (0.10-second duration shown)
T wave: normal size and configuration
QT interval: within normal limits and constant (0.36-second duration shown)
Other: gradual onset and cessation
An elevated heart rate increases myocardial oxygen demands. If the patient can’t meet these demands (for example, because of coronary artery disease), ischemia and further myocardial damage may occur.
Intervention
Treatment focuses on finding the primary cause. If it’s high catecholamine levels, a beta-adrenergic blocker may slow the heart rate. After MI, persistent sinus tachycardia may precede heart failure or cardiogenic shock.
Sinus arrest
In sinus arrest, the normal sinus rhythm is interrupted by an occasional, prolonged failure of the SA node to initiate an impulse. Therefore, sinus arrest is caused by episodes of failure in the automaticity of impulse formation of the SA node. The atria aren’t stimulated, and an entire PQRST complex is missing from the ECG strip. Except for the missing complex, or pause, the ECG usually remains normal.
During a sinus arrest, the sinus node resets itself so that when the impulse is initiated, the complex that occurs after the pause will be out of the cycle and the rate will usually be different from the rate before the pause.
Sinus arrest may result from an acute inferior wall MI, increased vagal tone, or the use of certain drugs, such as cardiac glycosides, calcium channel blockers, and beta-adrenergic blockers. The arrhythmia may also be linked to sick sinus syndrome. The patient has an irregular pulse rate associated with the pauses in sinus rhythm. If the pauses are infrequent, the patient is asymptomatic. If they occur frequently and last for several seconds, however, the patient may have signs of decreased cardiac output.
Characteristics of sinus arrest
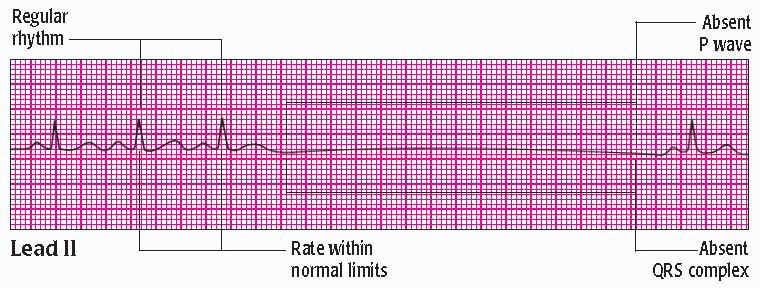 |
Atrial rhythm: regular, except for the missing complex
Ventricular rhythm: regular, except for the missing complex
Atrial rate: within normal limits but varies because of pauses (94 beats/minute shown)
Ventricular rate: within normal limits but varies because of pauses (94 beats/minute shown)
P wave: normal size and configuration (One P wave precedes each QRS complex but is absent during a pause.)
PR interval: within normal limits and constant when the P wave is present; not measurable when the P wave is absent (0.20-second duration shown on all complexes surrounding the arrest)
QRS complex: normal duration and configuration; absent during pause (0.08-second duration shown)
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Get Clinical Tree app for offline access