Chapter 26. Drugs used in the treatment of malignant disease
LEARNING OBJECTIVES
At the end of this chapter, the reader should be able to:
• describe the main stages of the cell cycle
• explain how the main classes of drugs for cancer are classified
• give some examples of each class and which cancers they are used for
• give an account of the important general adverse effects of anticancer drugs, e.g. myelosuppression
• describe the advantages of combination chemotherapy and be aware of newer developments in monoclonal antibody treatments
• define the terms palliative and adjuvant therapy
• appreciate the problems of administering drugs, e.g. extravasation and dangers to staff
• give an account of the nurse’s involvement in cancer chemotherapy and in patient counselling and care
Introduction
A great deal has been discovered about normal cell function and cell division, but after many years of research it is still not known exactly why malignant cells behave as they do. The pattern of their behaviour is familiar. Instead of differentiating in an orderly fashion to take their place in the formation of some tissue, they multiply in a haphazard way showing little, if any, attempt at differentiation and, further, instead of remaining in their organ of origin they invade neighbouring structures. Cell emboli from new growths are swept in the blood or lymphatic circulation to distant parts of the body, take root, and set up further tumours, known as secondary deposits or metastases.
Nuclear division and cytotoxic drugs
The cells of the body vary enormously in appearance and function, but all share some common characteristics. With very few exceptions (e.g. erythrocytes), cells consist of a nucleus surrounded by cytoplasm. The most vital component of the nucleus is deoxyribonucleic acid (DNA), which consists of two chains of molecules arranged into a double helix. DNA contains the code which, through production of messenger RNA, determines the types of proteins that are made by the cell and thus ultimately how the cell functions.
Most cytotoxic drugs interfere with DNA or RNA and thus they have a profound effect on cells and their functions. Unfortunately, these actions are not confined to the malignant cells, but affect normal cells as well.
Some cells in the body divide frequently to replace those that have become worn out, particularly the cells of the bone marrow, the lymphatic system and the lining of the intestinal tract, and these are particularly sensitive to the action of cytotoxic drugs.
The cell cycle
The cell goes through the following phases:
• G 1 phase
• S phase
• G 2 phase
• mitotic phase.
During its life the cell passes through a series of changes. The newly formed cell enters the G1phase, which is a period of protein synthesis and intense metabolic activity. This may last for a variable time, from a few hours to many years. Many cells remain in this phase throughout the life of the organism, but some undergo division and enter the S phase. This phase is short and is concerned with DNA and RNA synthesis so that the DNA strands may split when cell division occurs. It is a period of great metabolic activity. The G2phase which follows is a short period of consolidation before cell division occurs. In the mitotic phase the DNA spiral splits longitudinally so that each daughter cell has its full complement of DNA, which is exactly the same as that in the parent cell (Fig. 26.1). A proportion of the cells in a cancer are in a resting phase, sometimes called the G0phase, when they are not dividing. This is important because at this stage they are very resistant to chemotherapy.
 |
| Figure 26.1 Phases of the cell cycle. |
Drugs and the cell cycle
Some cytotoxic drugs will affect cells at any phase in their life cycle; others will only act at a single phase of the cell cycle, usually when the cell is dividing, and are called phase-specific. It follows therefore that when using phase-specific drugs repeated dosage is necessary if the maximum effect is to be achieved.
The term neoplastic growth, incidentally, refers to any new and abnormal growth, which may be either benign or malignant.
.
Treatment with drugs
Current aims of chemotherapy
The aim of treating neoplastic disease with drugs is to find a drug that will kill the neoplastic cells while leaving the normal cells of the body unharmed. However, the metabolic process of the neoplastic cells is so very similar to or perhaps even the same as that of normal cells that so far it has been impossible to reach this ideal. Nearly all drugs that have so far been discovered, although having a marked toxic effect on neoplastic cells, have some adverse effect on the normal cells of the body, especially those of the bone marrow. The best that can be done is to give the cytotoxic drug or drugs at repeated intervals so arranged that the recovery of normal cells can occur but little recovery of cancer cells is possible. It may then be possible progressively to reduce the number of malignant cells without unduly reducing the normal cells until ultimately all the malignant cells are eradicated (Fig. 26.2).
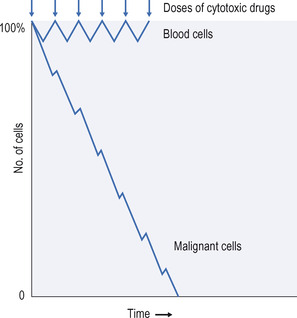 |
| Figure 26.2 Progressive reduction in the number of malignant cells produced by repeated doses of a cytotoxic drug, with recovery of the normal blood cells. An ideal therapeutic response. |
There are now, however, newer types of drugs on the market that are designed to target certain cells more specifically. It has long been the dream of the drug designers to design the successful ‘magic bullet’ – the drug that affects only the cancer cell. In practical terms, this involves attaching a cytotoxic drug to another chemical that will bind only to some marker on the surface of a cancer cell, and kill it while sparing normal dividing cells that do not have the marker. This dream has not yet been realized, although so-called biologic drugs have been developed that target specific antigens on the cancer cell and block the production of growth factors that promote cancer cell proliferation (see below).
.
The natural history of cancer
The growth rate of tumours varies considerably and the development of clinical symptoms and signs occurs at a late stage in the disease process (Fig. 26.3). Note particularly the long subclinical period and the fact that after chemotherapy, although the patient is apparently in full clinical remission, a small amount of tumour may remain.
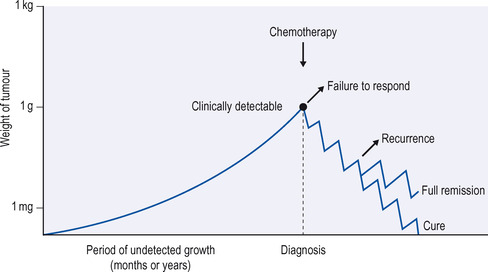 |
| Figure 26.3 Tumour growth and possible responses to chemotherapy. Modified from Ritter et al, A textbook of clinical pharmacology, 3rd edn, Edward Arnold, London. |
As a result of these considerations and a large amount of work on animal models of cancer, certain general principles and features of treatment have emerged:
• Cytotoxic drugs are usually given in intermittent high-dose treatments over long periods.
• The smaller the mass of tumour treated, the better the result, because small tumours have less resting cells which are insensitive to chemotherapy.
• Suppression of the bone marrow is very common, as cytotoxic drugs have to be given at the maximum tolerated dose.
Main classes of drugs
There are several different classes of drugs for the treatment of cancer:
• cytotoxic drugs
• sex hormones and hormone antagonists
• drugs affecting the immune response
• other immunomodulating drugs.
Cytotoxic drugs
Drugs in this group kill dividing cells and are therefore toxic not only to cancer cells but also to healthy dividing cells in the body. It is, nevertheless, perhaps the most widely used group, and there are several different types of drug within this group:
• alkylating agents
• cytotoxic antibiotics
• antimetabolites
• topoisomerase I inhibitors (campothecins).
.
Alkylating agents
These are chemically very active substances that combine with the DNA in the cell nucleus and thus damage or kill the cell. Unfortunately, although these substances have a marked effect on certain types of malignant cells, they also damage normal cells, particularly those of the bone marrow and gastrointestinal tract, which have a high rate of division. There are a number of alkylating agents now available.
Chlormethine (mustine) is related to mustard gas and is used in the treatment of neoplastic diseases of the lymphoreticular system such as Hodgkin’s disease, and with less success in certain carcinomas such as those of the ovary and bronchus. Because of toxicity its use is decreasing and it is now rarely used.
Therapeutic use. Chlormethine is given by intravenous injection, and as it is very irritant it is common practice to set up an intravenous infusion of saline and inject chlormethine into the infusion tubing and flush it through the vein with saline.
Adverse effects. Most patients experience nausea and vomiting for some hours after treatment. Bone marrow suppression is an ever-present risk, usually affecting the white cells and platelets.
Chlormethine may also be injected into malignant effusions and may either slow down or prevent their formation.
Cyclophosphamide was developed in an attempt to improve the therapeutic effectiveness of this type of drug. Cyclophosphamide itself is non-toxic, but in the liver it is split by enzymes which release cytotoxic metabolites. It can be given orally or intravenously, either daily or weekly, and is frequently combined with other cytotoxic agents. The therapeutic effect is usually delayed for a week or more.
Adverse effects. These include depression of the bone marrow and loss of hair (alopecia). A metabolite called acrolein is excreted in the urine, which can cause severe cystitis. This may be avoided by giving a high fluid intake (4 litres a day) or combining it with the drug mesna, which binds to acrolein and neutralizes it (see also later).
Ifosfamide is closely related to cyclophosphamide, from which it differs slightly in efficacy. It is less likely to depress the blood count than cyclophosphamide, but is more likely to damage the kidneys and bladder. To prevent this adverse effect it is, like cyclophosphamide, combined with mesna.
Chlorambucil is a useful drug of the chlormethine group. It is effective by mouth and although depression of the bone marrow can occur, vomiting is unusual.
Therapeutic use. Chlorambucil is given orally over long periods. It is one of the few cytotoxic drugs that is used continuously rather than as high-dose intermittent treatment. It has been used on an outpatient basis but community chemotherapy is now being introduced. Nevertheless, the patient should have regular blood counts; if severe bone marrow suppression occurs, recovery may be slow. It is effective against various forms of Hodgkin’s disease and non-Hodgkin’s lymphoma and is probably the drug of choice in chronic lymphatic leukaemia.
Busulfan is used particularly in chronic myeloid leukaemia, where it has a selective depressing action on the abnormal white cells. Excessive dosage will produce dangerous depression of normal white cells and platelets.
Therapeutic use. Busulfan is given orally. Treatment is continued over weeks or months and is modified by the response of the patient.
Adverse effects. In addition to bone marrow depression, it can cause pigmentation and fibrosis of the lungs.
Melphalan is used particularly in multiple myelomatosis. It is usually given daily for a week, and may be repeated if the blood count is satisfactory. Melphalan is a powerful depressant of white cells and platelets.
Lomustine (CCNU) is similar in many ways to the alkylating agents and, although its mode of action is different, it is effective against the same types of cancer. It is given orally as a single dose and should not be repeated for 4 or preferably 6 weeks, as depression of white cells and platelets may be delayed.
Adverse effects. Nausea and sometimes vomiting is common for about 12 hours after dosage.
Carmustine is similar to lomustine.
Estramustine is a combination of chlormethine and an estrogen. It is an example of the magic-bullet approach. The drug is meant to be concentrated in tissues that have estrogen receptors and both the estrogen and the cytotoxic chlormethine attack the cancer cell. Unlike many other cytotoxic agents. estramustine does not destroy the DNA.
Therapeutic use. Estramustine is used in some cases of prostate cancer, for which estrogens have long been used. It is administered orally in capsule form.
Adverse effects. These include gynaecomastia because of the estrogenic effect, and heart and liver toxicity. The drug is contraindicated in heart and liver disease, and in patients with peptic ulcer.
Cytotoxic antibiotics
This is also a group of very widely used anticancer drugs. They are drugs derived from microorganisms and they work mainly by preventing cell division either through a direct action on the DNA itself or by blocking the enzymes involved in DNA replication, or through both actions. Some important ones are:
Doxorubicin ( Adriamycin) is probably the most widely used cytotoxic antibiotic. It has been used successfully to treat lymphomas, leukaemias and solid tumours. It has two actions: it binds to the DNA itself, thus preventing both DNA and RNA synthesis; more importantly for this drug, it inhibits the action of an enzyme called topoisomerase II that allows DNA to be reproduced (see also below).
Therapeutic use. It is given by intravenous injection, every 3 weeks, usually in combination with other cytotoxic drugs. It can be instilled directly into the bladder.
Adverse effects. It can depress bone marrow and this occurs about 2 weeks after treatment, rather later than with most cytotoxic drugs. It is toxic to heart muscle and this requires regular ECG monitoring. Toxicity is dose related. Other effects are nausea, vomiting and hair loss.
Mitoxantrone and epirubicin are both structurally related to doxorubicin. Mitoxantrone is given as a single injection at 3-weekly intervals. It is used in a variety of cancers. The incidence of adverse effects is relatively low and it is useful in controlling the disease, particularly on an outpatient basis. It does, however, cause bone marrow suppression and has a dose-related cardiotoxicity. Epirubicin is less cardiotoxic than is doxorubicin. Idarubicin has similar properties to those of doxorubicin and may replace it. It is indicated for acute leukaemias and advanced breast cancer. It is given by mouth or intravenously. Like many of the cytotoxic antibiotics it is cardiotoxic. Daunorubicin, too, has similar properties to those of doxorubicin and is used to treat acute leukaemias. It is administered by intravenous infusion. There is a liposomal preparation of daunorubicin that is licensed for use in treating HIV-related Kaposi’s sarcoma.
Bleomycin, another antibiotic with relatively weak anticancer effects, is used in combination to treat lymphomas and testicular cancers. However, unlike all the drugs already discussed, it does not depress the bone marrow. It is usually injected at weekly intervals, and a spike of fever may follow injection. Prolonged use leads to lung fibrosis.
Nursing point
Nursing point
Cytotoxic drugs, especially antibiotics, can be necrotic to local tissue if they leak into extravascular compartments. Therefore when given intravenously, only specially trained staff should administer them.
Antimetabolites
These agents resemble substances used by the cells for their metabolic processes. They thus become incorporated in the cells and because they cannot be metabolized they normally cause the cell to die. Malignant cells often have a very rapid metabolic turnover and thus incorporate antimetabolites more rapidly than do normal cells. It is thus possible to kill the majority of malignant cells without interfering too drastically with normal cells. Excessive dosage will inhibit normal cell production, particularly in the bone marrow. Many antimetabolites resemble the purines or pyrimidines, which are the building blocks of DNA. They become incorporated in the growing strand of DNA and stop the process. Examples include:
• methotrexate
• mercaptopurine (purine analogue)
• fluorouracil (pyrimidine analogue)
• capecitabine
• raltitrexed
• tegafur
• tioguanine (purine analogue)
• cytarabine (pyrimidine analogue)
• fludarabine (purine analogue)
• cladribine (purine analogue)
• gemcitabine (pyrimidine analogue).
Methotrexate is similar in structure to folic acid and it blocks one of the chemical processes necessary for the production of cell nuclear material from folic acid.
Therapeutic use. Methotrexate can be given orally, intravenously or intrathecally, but large doses are not well absorbed from the intestine and must be given by injection. Dosage schedules depend on the type of cancer being treated. It is excreted via the kidney and it is essential that renal function is measured before starting treatment. With impaired function, the dose is reduced. The drug is prescribed together with folic acid as a supplement.
In certain types of malignant disease, a very large and potentially lethal dose of methotrexate is given; then, after 24 hours, giving folinic acid reverses the action of the drug. It is extremely important that this is carried out precisely. This method is known as folinic acid rescue.
Adverse effects. In addition to bone marrow suppression, methotrexate can cause liver damage and mouth ulceration (Van Outryve et al 2002).
Methotrexate in low doses is also used as an immunosuppressant in rheumatoid arthritis and psoriasis (see p. 116).
Mercaptopurine is closely related chemically to adenine and hypoxanthine, two substances used in the formation of the cell nucleus. It is believed that mercaptopurine replaces these substances in the nucleus of cells and thereby prevents their further division. It is used in combination with other drugs in the treatment of acute leukaemia, a disease where the bone marrow is rapidly overgrown by very malignant white cells. Mercaptopurine can also be used in chronic myeloid leukaemia.
Therapeutic use. Mercaptopurine is given daily by mouth, and the course of treatment is determined by the response of the patient. Excessive or prolonged treatment will produce depression of normal white cells.
Fluorouracil is another antimetabolite that is used with some benefit in a wide variety of tumours, including those of the gastrointestinal tract. It is given by intravenous infusion or as a bolus; the dose varies with circumstances. It can also be applied locally to certain skin cancers. It produces leucopenia and, in particular, ulceration of the mouth.
Cytarabine is a drug that interferes with the nuclear function in the malignant cell and is used in acute leukaemia. It can cause bone marrow depression.
Raltitrexed blocks one of the enzymes involved in DNA synthesis, namely thymidylate synthetase. It is administered intravenously to treat advanced colorectal cancer when drugs such as fluorouracil cannot be used. It is usually well tolerated by patients, but can cause gastrointestinal upsets and myelosuppression (a reduction in blood cell production by the bone marrow).
Plant and animal-derived drugs
These drugs can be divided into:
• vinca alkaloids
• etoposide
• trastuzumab
• taxanes
• campothecins.
Vinca alkaloids comprise:
• vinblastine
Get Clinical Tree app for offline access



