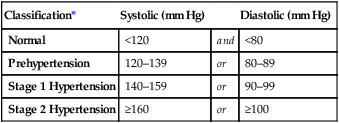
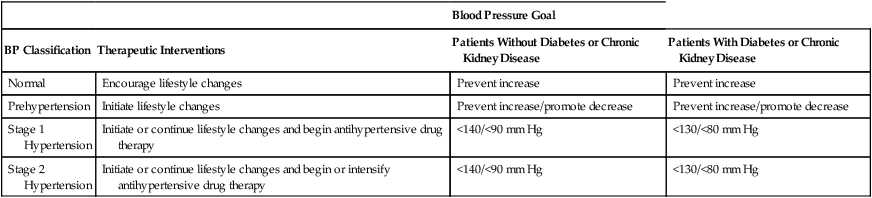
CHAPTER 47 In 2003, the National Heart, Lung, and Blood Institute issued revised clinical guidelines on hypertension. This document—The Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure, known simply as JNC 7—was prepared by a special committee of the National High Blood Pressure Education Program. Recommendations in JNC 7 update and simplify those of JNC 6, released in 1997. Important changes include a new BP classification scheme, increased emphasis on controlling systolic BP, and the recommendation to use thiazide diuretics as initial therapy for most patients. Throughout this chapter, clinical practice recommendations reflect those in JNC 7, except where noted otherwise.* JNC 7 defines four BP categories: normal, prehypertension, stage 1 hypertension, and stage 2 hypertension (Table 47–1). This scheme differs from that of JNC 6 in three ways: TABLE 47–1 Classification of Blood Pressure for Adults Age 18 and Older *Not taking any antihypertensive drugs and not acutely ill. When systolic and diastolic pressures fall into different categories, the higher category should be selected to classify BP status. For example, 160/92 mm Hg should be classified as stage 2 hypertension. Isolated systolic hypertension is defined as systolic BP of 140 mm Hg or higher and diastolic BP below 90 mm Hg and staged appropriately (eg, 170/82 is defined as stage 2 isolated systolic hypertension). Data from The Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. JAMA 289:2560–2572, 2003. • The cutoff values for normal BP have been reduced. • A new category—prehypertension—has been added. • Two classes of hypertension—stages 2 and 3 from JNC 6—have been combined into one—stage 2 in JNC 7—because management of both is much the same. There are two broad categories of hypertension: primary hypertension and secondary hypertension. As indicated in Table 47–2, primary hypertension is by far the most common form of hypertensive disease. Less than 10% of people with hypertension have a secondary form. TABLE 47–2 Types of Hypertension and Their Frequency Chronic hypertension is associated with increased morbidity and mortality. Left untreated, prolonged elevation of BP can lead to heart disease (myocardial infarction [MI], heart failure, angina pectoris), kidney disease, and stroke. The degree of injury is directly related to the degree of pressure elevation: The higher the pressure, the greater the risk. Among people 40 to 70 years old, the risk of cardiovascular disease is doubled for each 20 mm Hg increase in systolic BP or each 10 mm Hg increase in diastolic BP—beginning at 115/75 mm Hg and continuing through 185/155 mm Hg. For people over the age of 50, elevated systolic BP poses a greater risk than elevated diastolic BP (Box 47–1). For patients of all ages, hypertension-related deaths result largely from cerebral hemorrhage, renal failure, heart failure, and MI. As discussed above, some forms of hypertension result from a treatable cause, such as Cushing’s syndrome, pheochromocytoma, and use of oral contraceptives (see Table 47–2). Patients should be evaluated for these causes and managed appropriately. In many cases, direct treatment of the underlying cause can control BP, thereby eliminating the need for further antihypertensive therapy. We can reduce BP in two ways: We can implement healthy lifestyle changes and we can treat with antihypertensive drugs. As shown in Table 47–3, for people with prehypertension, lifestyle changes are all that is needed. In contrast, for those with hypertension—either stage 1 or stage 2—a combination of lifestyle changes and drugs is indicated. Lifestyle changes and drug therapy are discussed in detail below. TABLE 47–3 Overview of Blood Pressure Management in Adults 18 Years and Older Recommendations from The Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. JAMA 289:2560–2572, 2003. There is a direct relationship between obesity and elevation of BP. Fortunately, weight loss can reduce BP in 60% to 80% of overweight hypertensive individuals. In addition, weight loss can enhance responses to antihypertensive drugs. Consequently, a program of calorie restriction and exercise is recommended for all patients who are overweight. The goal is to achieve a body mass index in the normal range (18.5 to 24.9).* Two studies have shown that we can reduce BP by adopting a healthy diet, known as the Dietary Approaches to Stop Hypertension (DASH) eating plan. This diet is rich in fruits, vegetables, and low-fat dairy products, and low in total fat, saturated fats, and cholesterol. In addition, the plan encourages intake of whole-grain products, fish, poultry, and nuts, and recommends minimal intake of red meat and sweets. Details are available online at www.nhlbi.nih.gov/health/public/heart/hbp/dash. Smoking is a major risk factor for cardiovascular disease. Each time a cigarette is smoked, BP rises. In patients with hypertension, smoking can reduce the effects of antihypertensive drugs. Clearly, all patients who smoke should be strongly encouraged to quit. (Pharmacologic aids to smoking cessation are discussed in Chapter 39.) As a rule, use of nicotine replacement products (eg, nicotine gum, nicotine patch) does not elevate BP. The cardiovascular benefits of quitting become evident within 1 year. The principal determinants of BP are summarized in Figure 47–1. As indicated, arterial pressure is the product of cardiac output and peripheral resistance. An increase in either will increase BP. As discussed in Chapter 43, the kidney plays a central role in long-term regulation of BP. When BP falls, glomerular filtration rate (GFR) falls too, thereby promoting retention of sodium, chloride, and water. The resultant increase in blood volume increases venous return to the heart, causing an increase in cardiac output, which in turn increases arterial pressure. We can neutralize renal effects on BP with diuretics. The major mechanisms for lowering BP are summarized in Figure 47–2 and Table 47–4. The figure depicts the principal sites at which antihypertensive drugs act. The table summarizes the effects elicited when drugs act at these sites. The numbering system used below corresponds with the system used in Figure 47–2 and Table 47–4. TABLE 47–4 Summary of Antihypertensive Effects Elicited by Drug Actions at Specific Sites *Site numbers in this table correspond with site numbers in Figure 47–2.
Drugs for hypertension
Basic considerations in hypertension
Classification of blood pressure

Classification*
Systolic (mm Hg)
Diastolic (mm Hg)
Normal
<120
and
<80
Prehypertension
120–139
or
80–89
Stage 1 Hypertension
140–159
or
90–99
Stage 2 Hypertension
≥160
or
≥100
Types of hypertension

Type of Hypertension
Frequency (%)
Primary (Essential) Hypertension
92
Secondary Hypertension
Chronic renal disease
4
Renovascular disease
2
Oral contraceptive–induced
1
Coarctation of the aorta
0.3
Primary aldosteronism
0.2
Cushing’s syndrome
0.1
Pheochromocytoma
0.1
Sleep apnea
?
Thyroid or parathyroid disease
?
Consequences of hypertension
Management of chronic hypertension
Basic considerations
Patient evaluation
Hypertension with a treatable cause.
Therapeutic interventions

Blood Pressure Goal
BP Classification
Therapeutic Interventions
Patients Without Diabetes or Chronic Kidney Disease
Patients With Diabetes or Chronic Kidney Disease
Normal
Encourage lifestyle changes
Prevent increase
Prevent increase
Prehypertension
Initiate lifestyle changes
Prevent increase/promote decrease
Prevent increase/promote decrease
Stage 1 Hypertension
Initiate or continue lifestyle changes and begin antihypertensive drug therapy
<140/<90 mm Hg
<130/<80 mm Hg
Stage 2 Hypertension
Initiate or continue lifestyle changes and begin or intensify antihypertensive drug therapy
<140/<90 mm Hg
<130/<80 mm Hg
Lifestyle modifications
Weight loss.
The DASH eating plan.
Smoking cessation.
Drug therapy
Review of blood pressure control
Principal determinants of blood pressure
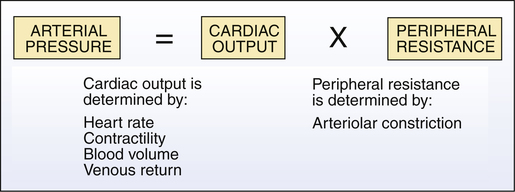
 Primary determinants of arterial blood pressure.
Primary determinants of arterial blood pressure.
Systems that help regulate blood pressure
Renal regulation of blood pressure.
Antihypertensive mechanisms: sites of drug action and effects produced

Site of Drug Action*
Representative Drug
Drug Effects
1.Brainstem
Clonidine
Suppression of sympathetic outflow decreases sympathetic stimulation of the heart and blood vessels.
2.Sympathetic ganglia
Mecamylamine†
Ganglionic blockade reduces sympathetic stimulation of the heart and blood vessels.
3.Adrenergic nerve terminals
Reserpine
Reduced norepinephrine release decreases sympathetic stimulation of the heart and blood vessels.
4.Cardiac beta1 receptors
Propranolol
Beta1 blockade decreases heart rate and myocardial contractility.
5.Vascular alpha1 receptors
Prazosin
Alpha1 blockade causes vasodilation.
6.Vascular smooth muscle
Hydralazine
Relaxation of vascular smooth muscle causes vasodilation.
7.Renal tubules
Hydrochlorothiazide
Promotion of diuresis decreases blood volume.
Components of the renin-angiotensin-aldosterone system (8a to 8e)
8a. Beta1 receptors on juxtaglomerular cells
Propranolol
Beta1 blockade suppresses renin release, resulting in (1) vasodilation secondary to reduced production of angiotensin II, and (2) prevention of aldosterone-mediated volume expansion.
8b. Renin
Aliskiren
Inhibition of renin suppresses formation of angiotensin I, which in turn decreases formation of angiotensin II, and thereby reduces (1) vasoconstriction and (2) aldosterone-mediated volume expansion
8c. Angiotensin-converting enzyme (ACE)
Captopril
Inhibition of ACE decreases formation of angiotensin II and thereby prevents (1) vasoconstriction, and (2) aldosterone-mediated volume expansion.
8d. Angiotensin II receptors
Losartan
Blockade of angiotensin II receptors prevents angiotensin-mediated vasoconstriction and aldosterone-mediated volume expansion.
8e. Aldosterone receptors
Eplerenone
Blockade of aldosterone receptors in the kidney promotes excretion of sodium and water, and thereby reduces blood volume.
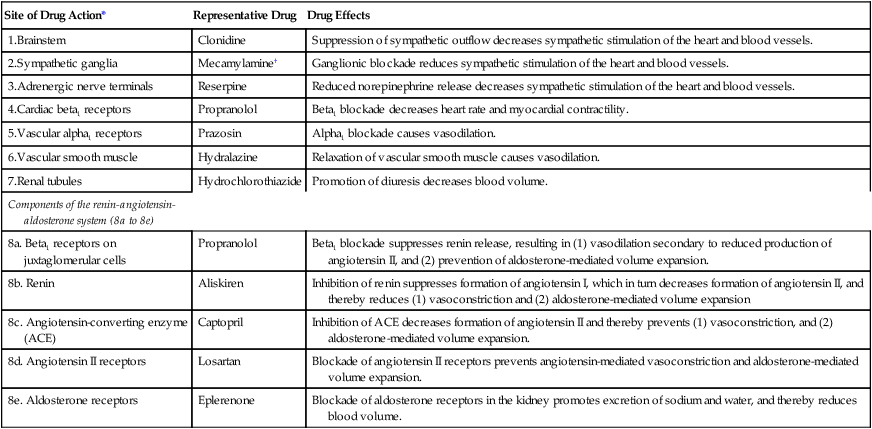
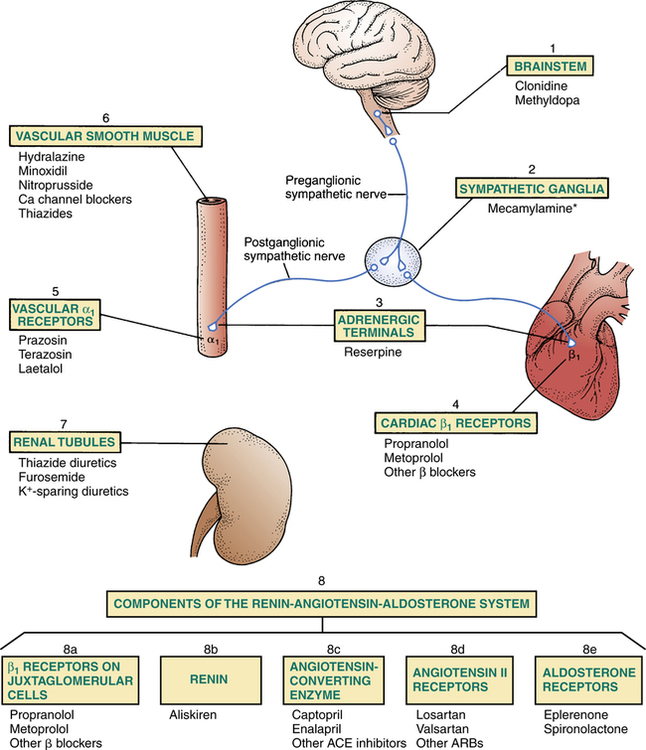
 Sites of action of antihypertensive drugs.
Sites of action of antihypertensive drugs.
Note that some antihypertensive agents act at more than one site: beta blockers act at sites 4 and 8a, and thiazides act at sites 6 and 7. The hemodynamic consequences of drug actions at the sites depicted are summarized in Table 47–4. (ACE = angiotensin-converting enzyme, ARB = angiotensin II receptor blocker.)
*No longer available in the United States.
< div class='tao-gold-member'>
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Drugs for hypertension
Only gold members can continue reading. Log In or Register to continue
Get Clinical Tree app for offline access

