Chapter 28. Drugs and the eye
Structure of the eye372
Conditions affecting the eye372
Types of drugs used374
Antifungal drugs377
Antiviral agents377
Steroids and non-steroidal anti-inflammatory drugs (NSAIDs)378
Drugs used in the treatment of age-related macular degeneration (AMD)383
Summary387
Guidance for use of ophthalmic preparations in hospital and care homes387
LEARNING OBJECTIVES
At the end of this chapter, the reader should be able to:
• list the different types of local preparations used in the eye
• state which antibiotics and antivirals are used to treat conditions affecting the eyes and list some of the more common infections treated
• explain what is meant by protozoan infections and how they are treated
• list steroids used topically to treat eye conditions
• explain what is meant by mydriasis and miosis; give examples of drugs that produce these effects and their uses for patients with eye conditions
• describe the different types of glaucoma and how they are treated
• list the local anaesthetics that can be topically applied to the eyes
• list that stains are used during when the eyes are examined and explain their purposes
Structure of the eye
The structure of the eye and orbit are shown in Figure 28.1.
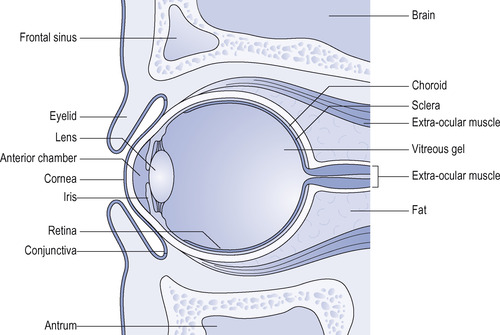 |
| Figure 28.1 Cross-sectional anatomy of the eye and orbit. |
Conditions affecting the eye
Eyecare includes eye disorders and their prevention, treatment and patient education. This is an important area of practice. Eye problems and traumatic disorders of the eye account for over 6% of all attendances at the Accident and Emergency Department in the UK, while worldwide, approximately 5 000 000 blinding injuries occur annually. Eye disorders are particularly common in older people and as the population ages, the number of people affected is increasing rapidly. Examples are cataracts, glaucoma and macular degeneration. Glaucoma and macular degeneration are both chronic conditions and it is very imprtant that patients should be able to apply their own medication if at all possible in order to maintain independence. Cataract removal is a common operation, now usually undertaken as a day-case procedure. The nurse plays an important role preparing patients undergoing cataract extraction preoperatively and teaching them how to use local medication during the postoperative period at home.
Local use of drugs on the eye – types of applications
The following preparations are used in the local treatment of eye diseases:
• eye lotions
• eye drops
• eye ointments
• subconjunctival injections
• injections into the anterior chamber at operation.
Whenever administering local preparations to the eye it is of paramount importance to ensure that the eye to receive treatment is clearly designated. Patients going to theatre for eye operations will usually have an arrow marked on the forehead pointing to the eye to be treated to avoid any confusion. Often only one eye is to be treated or the two eyes are to be treated differently. For example, after an operation for angle closure glaucoma in one eye, it may be necessary to dilate the pupil with mydriatic drugs. Instilling mydriatic eye drops into the incorrect eye could impair vision in the normal eye and be very disabling for the patient.
Eye lotions prescribed as collyrium
These are used to wash foreign material and irritants from the eye and some have a mild antiseptic action. They are applied using a giving set, eye bath or a soft plastic irrigation bottle. In an emergency the priority is to administer treatment quickly to the contaminated eye before damage is done to the conjunctiva and cornea.
The patient should lie back or sit in a chair with the head extended back. The lotion should preferably be warmed to body temperature and before washing the eye the lotion should be run into the medial canthus, the lids being firmly separated by the fingers. A towel held by the patient close to the face will absorb the run off. This is less unpleasant than pouring the lotion directly onto the cornea. The lotion should be irrigated slowly but steadily from the irrigation receptacle, the patient being instructed to move the eyes in all directions.
In emergency cases, as in chemical contamination, it is better to use plenty of running cold tap water at once rather than to lose time in starting the treatment. The irrigating fluid most commonly used in the clinical situation is normal saline. Alkaline chemical contamination can penetrate the eye by saponifying cell membranes, causing local production of soap and causing erosion to the cornea, tissue destruction and secondary vascular thrombosis; therefore, immediate treatment should be sought. At least 1 litre of normal saline solution should be used. Afterward use litmus paper to check the pH of the eye. If it is over pH 7, repeat with another irrigation of 1 litre of normal saline solution until the pH is 7 or below.
In cases of corneal damage, topical citrate and potassium ascorbate eye drops can improve the prognosis, though patients should be warned they do produce stinging. They can be used for acid or alkali burns to the cornea and are often supplemented with oral ascorbic acid (vitamin C) at high doses of 1.5 g a day to promote healing.
Eye drops prescribed as guttae
A number of drugs can be applied to the eyes by means of drops which should be instilled into the lower conjunctival sac. The patient is told to look upwards away from the dropper and the lower lid is held down with the finger. One drop only is instilled into the lower fornix and the patient is then told to close the eye for a short while and the excess is wiped away. When two or more eye-drop preparations are used at the same time of day, an interval of 3–5 minutes should be left between instilling two preparations, in order to avoid dilution and the overflow effect.
All drops and ointment should be sterile when supplied, and once opened can no longer be considered so.
Single dose unit packs are particularly useful for patients who require medication over long periods and who may develop sensitivity to benzalkonium chloride, the preservative present in most eye drops.
Nursing point
Nursing point
Drugs or preservatives in eye drops may become absorbed into or onto hydrophilic contact lenses and cause irritation. Therefore, lenses should be removed before eye drops are instilled and not worn again until the treatment is finished. Similarly, contact lenses should not be used with eye ointments. If a patient develops an eye infection, he or she should be advised to use disposable lenses until it has resolved or to use spectacles.
Eye ointments prescribed as oculentum
These are usually supplied in 4 or 5 g tubes with a long plastic nozzle. To apply, the lower lid is pulled down and the ointment is placed in the lower fornix of the eye. About half an inch or 1 cm of ointment is squeezed from the tube at each application. It is important to twist the tube upward so that the strip of ointment remains in the fornix as the tube is moved away from the eye.
Subconjunctival injections
This method of application is used to obtain immediately a high concentration of drugs such as anti-infective agents, corticosteroids or mydriatics in the anterior chamber. This would be appropriate in the treatment of an acute intraocular infection. This treatment is painful and the eye must first be thoroughly anaesthetized by the instillation of several drops of local anaesthetic. The injection is given with a hypodermic syringe and a fine needle. Some drugs are manufactured in a depot form and are bound to a base substance from which they are released slowly. For example, Depo-Medrone (methylprednisolone acetate) can be used as a steroid preparation for the local treatment of iridocyclitis (inflammation of the iris and ciliary body). It is given as a subconjunctival injection and its action is continuous over a period of 3–4 days.
Intracameral administration
For some diagnoses, it may be desirable to achieve high therapeutic concentrations of antibiotic drugs with a minimum of delay. This calls for delivery of the drug directly into the globe of the eye, either into the anterior chamber or the vitreous cavity.
Anterior chamber administration is frequently used during cataract operations, when, to constrict the pupil, the iris is irrigated directly with Miochol-E, which is an acetylcholine preparation. In severe intraocular infections – for example, postoperative endophthalmitis (inflammation within the eye, usually due to infection) – it may be necessary to remove a sample of the vitreous humour for bacteriological examination. It is timely to inject the vitreous cavity with broad-spectrum antibiotics. Antibiotics effective against a range of organisms can be used in this way, although care is needed to avoid any toxic effects on delicate intraocular structures such as the retina. Consequently, the injections need to be carefully prepared and used only in the recommended dosage, in volumes not exceeding 0.05–0.1 ml, and administration should generally be under sterile theatre conditions.
Types of drugs used
The following types of drug are in frequent use in the treatment of eye disorders:
• anti-infectives:
– antibiotics
– antifungals
– antivirals
• steroids and other anti-inflammatory drugs
• those which affect pupil size
• those used in the treatment of glaucoma
• local anaesthetics
• stains
• miscellaneous preparations.
Drugs can be administered to the eye by either local or systemic routes.
Antibacterial agents used in the eye
The three main classes of anti-infectives used in the eye are: antibacterials (also known as antibiotics), antivirals and antifungals. There are also anti-amoebics and antiprotozoals, which are commonly grouped with the antifungals. While many of the dose forms are available from proprietary manufacturers as mainline medicines, some must be ordered from special manufacturers who manufacture limited quantities in batches.
The antibiotics are summarized in Table 28.1.
| Drug(s) | Spectrum |
|---|---|
| Amikacin | Gram-negative, mycobacteria |
| Bacitracin zinc+polymixin B sulphate | Broad, Gram-negative, coliforms |
| Benzylpenicillin | Streptococcus |
| Ceftazidime | Broad, Pseudomonas |
| Cefuroxime | Broad, Staphylococcus |
| Chloramphenicol | Broad |
| Ciprofloxacin | Broad, Gram-negative |
| Erythromycin | Broad, Streptococcus Chlamydia |
| Framycetin sulphate | Broad, Gram-negative |
| Fusidic acid | Staphylococcus |
| Gentamicin | Broad, Gram-negative, Pseudomonas |
| Levofloxacin | Broad, Gram-negative |
| Neomycin sulphate+gramicidin+polymixin B sulphate | Broad |
| Ofloxacin | Broad, Gram-negative |
| Trimethoprim+polymixin B sulphate | Broad, Gram-negative, coliforms |
| Vancomycin | Staphylococcus, Clostridium |
Antibiotics are used to treat a wide range of eye infections and they may be administered in three ways:
• Drops are satisfactory for superficial inflammation such as conjunctivitis, but rapid dilution occurs because of the tears. The drops should be instilled at 2-hourly intervals at least, if a reasonable concentration of antibiotic is to be maintained.
• Ointments release the antibiotic more slowly and their action is helped by the eye being covered; they are especially useful for over-night use.
• Subconjunctival injection is the best way of ensuring a rapid and high concentration of antibiotic within the anterior ocular segment. The maximum volume which can be injected at one time is 1.0 ml.
Although, owing to the accessibility of the eye, diseases of the anterior segment can usually be effectively treated by means of the local administration of drugs, for those diseases which affect the posterior part, or the deeper intraocular structures, systemic administration is generally necessary.
Eye infections may be due to a variety of agents, both bacterial and viral. The correct antibiotic in the case of bacterial infections can be selected as a result of clinical observation and should be validated by bacterial or viral diagnostic tests.
Chloramphenicol and the quinolones are widely used in the treatment of superficial eye infections. They are active against a broad spectrum of bacteria and are particularly suitable for local administration as this avoids systemic toxicity. They include:
• chloramphenicol 0.5% drops or 1.0% ointment
• ciprofloxacin 0.3% drops and ointment
• levofloxacin 0.5% drops
• ofloxacin 0.3% drops.
These drugs are active against both Gram-positive and Gram-negative organisms.
Nursing point
Nursing point
The use of chloramphenicol has been questioned on account of its tendency to cause blood dyscrasias when given systemically. The evidence that these can arise as a result of local administration to the eye is still far from conclusive and it is widely used as first-line empirical therapy in most eye infections. Chloramphenicol remains in general use as it is by far the most effective drug for short-term use in bacterial infections of the eye and for prophylaxis. It functions by inhibiting peptidyl transferase, thus preventing peptide bond formation causing misreading of messenger RNA, which leaves the bacteria unable to synthesize proteins vital to their growth.
Ofloxacin, levofloxacin and ciprofloxacin, members of the quinolone group, have a broad spectrum of antibacterial action, including activity against Pseudomonas aeruginosa. The fluoroquinolones work by inhibiting DNA gyrase, an enzyme necessary to separate replicated DNA, thereby inhibiting cell division. They have a broader spectrum of activity than chloramphenicol and fewer local side-effects than gentamicin while maintaining a similar spectrum of activity to those agents. Ofloxacin rivals chloramphenicol as a general prophylactic antibiotic.
Antibiotics of the penicillin group are rarely, if ever, used as local eye applications as they have a marked tendency to cause allergic reactions. However, they have an important place in the treatment of spreading infections of the eyelids, which are commonly of staphylococcal origin (provided the infection has not developed resistance). In such cases the infection is deep in the tissues, requiring systemic rather than local administration. In general, a broad-spectrum penicillin is best, but if the infection is acquired in hospital, one of the penicillinase-resistant types is preferable. β-Lactam antibiotics work by inhibiting the formation of peptidoglycan cross-links in the bacterial cell wall. The β-lactam part of the molecule of penicillin binds to the enzyme (DD-transpeptidase) that links the peptidoglycan molecules in bacteria, and this weakens the cell wall of the bacterium, leading to cell death.
Erythromycin eye ointment 0.5% is mainly used for chlamydial conjuctivitis although it is also active against superficial streptococcal infections.
Sodium fusidate is particularly active against penicillin-resistant staphylococci. It has the property of being concentrated in bone and other connective tissues, including the sclera of the eye and the vitreous, and is therefore useful in treating intraocular infections, especially those acquired in the operating theatre, which can often be due to resistant organisms. Fusidic acid is also used as eye drops in gel, which liquefies on contact with the conjunctiva, for a variety of superficial infections. Frequently after major intraocular operations, antibiotics are injected subconjunctivally. Fusidic acid works by interfering with bacterial protein synthesis, preventing the translocation of the elongation factor G (EF-G) from the ribosome, thus inhibiting bacterial replication.
Prophylaxis against postoperative infection is a routine part of eye surgery. Common procedures such as removal of cataracts are now performed as day cases. It is important to ensure that the eye is protected from infection; therefore, broad-spectrum agents are preferred, such as gentamicin, which interrupts protein synthesis in Gram-negative bacteria, and cefuroxime, a cephalosporin with effectiveness against both Gram-positive and Gram-negative organisms.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


