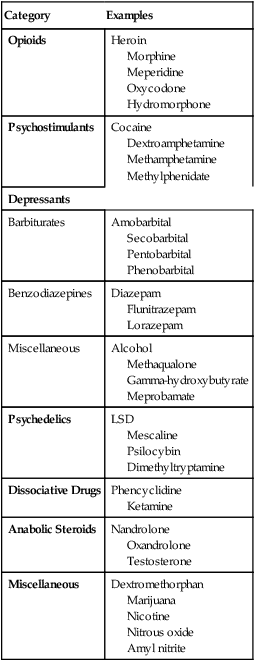
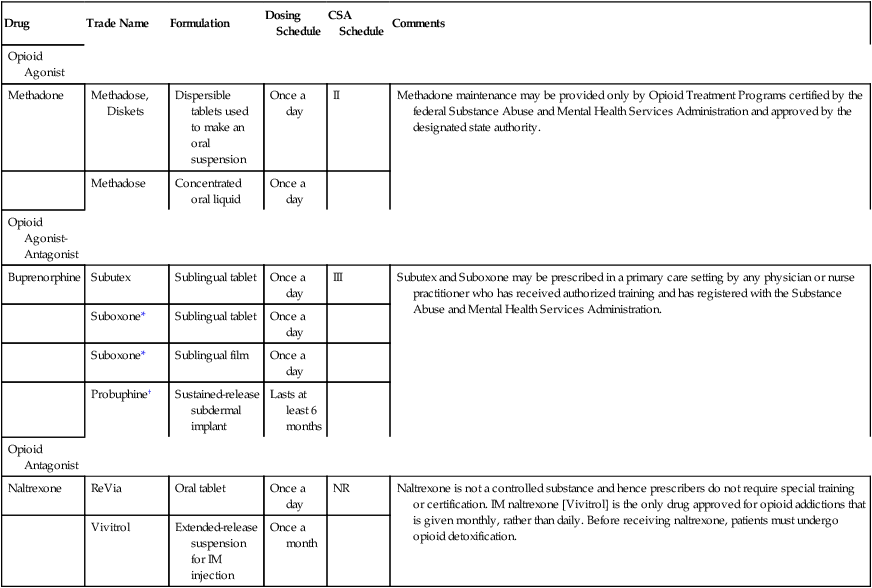
CHAPTER 40 In this chapter, we discuss all of the major drugs of abuse except alcohol (Chapter 38) and nicotine and tobacco (Chapter 39). As indicated in Table 40–1, abused drugs fall into seven major categories: (1) opioids, (2) psychostimulants, (3) depressants, (4) psychedelics, (5) dissociative drugs, (6) anabolic steroids, and (7) miscellaneous drugs of abuse. The basic pharmacology of many of these drugs is presented in previous chapters, and hence their discussion here is brief. Agents that have not been addressed previously (eg, marijuana, d-lysergic acid diethylamide [LSD]) are discussed in depth. Structural formulas of representative controlled substances are shown in Figure 40–1. Street names for abused drugs are given in Table 40–2. TABLE 40–1 Pharmacologic Categorization of Abused Drugs TABLE 40–2 Some Street Names for Abused Drugs The opioids (eg, heroin, oxycodone, meperidine) are major drugs of abuse. As a result, most opioids are classified as Schedule II substances. The basic pharmacology of the opioids is discussed in Chapter 28. In an effort to reduce OxyContin abuse, the controlled-release tablets were reformulated in 2010. The new formulation bears the imprint OP, rather than OC, which appeared on the old formulation. Compared with the old tablets, OxyContin OP tablets are much harder to crush into a powder. And if exposed to water or alcohol, the tablets just form a gummy blob, rather than a solution that can be drawn into a syringe and injected. However, there is no evidence that OxyContin OP tablets are less subject to abuse, diversion, overdose, or addiction than the old tablets. As noted in Chapter 28, oxycodone is also available in a tamper resistant immediate-release formulation, sold as Oxecta. Treatment of acute opioid toxicity is discussed at length in Chapter 28 and summarized here. Overdose produces a classic triad of symptoms: respiratory depression, coma, and pinpoint pupils. Naloxone [Narcan], an opioid antagonist, is the treatment of choice. This agent rapidly reverses all signs of opioid poisoning. However, dosage must be titrated carefully. Why? Because if too much is given, the addict will swing from a state of intoxication to one of withdrawal. Owing to its short half-life, naloxone must be re-administered every few hours until opioid concentrations have dropped to nontoxic levels, which may take days. Failure to repeat naloxone dosing may result in the death of patients who had earlier been rendered symptom free. Three kinds of drugs are employed for long-term management: opioid agonists, opioid agonist-antagonists, and opioid antagonists. Opioid agonists (methadone) and agonist-antagonists (buprenorphine) substitute for the abused opioid and are given to patients who are not yet ready for detoxification. In contrast, opioid antagonists (naltrexone) are used to discourage renewed opioid use after detoxification has been accomplished. Drugs used for long-term management of opioid addiction are summarized in Table 40–3. TABLE 40–3 Drugs for Long-Term Management of Opioid Addiction CSA = Controlled Substances Act, NR = not regulated under the CSA. *In addition to buprenorphine, Suboxone contains naloxone, an opioid antagonist, to discourage IV dosing. Buprenorphine [Subutex, Suboxone], an agonist-antagonist opioid, was approved for treating addiction in 2002. As discussed in Chapter 28, the drug is a partial agonist at mu receptors and a full antagonist at kappa receptors. Buprenorphine can be used for maintenance therapy and to facilitate detoxification (see above). When used for maintenance, buprenorphine alleviates craving, reduces use of illicit opioids, and increases retention in therapeutic programs. The basic pharmacology of buprenorphine is presented in Chapter 28. The family of CNS depressants consists of barbiturates, benzodiazepines, alcohol, and other agents. With the exception of the benzodiazepines, all of these drugs are more alike than different. The benzodiazepines have properties that set them apart. The basic pharmacology of the benzodiazepines, barbiturates, and most other CNS depressants is presented in Chapter 34; the pharmacology of alcohol is presented in Chapter 38. Discussion here is limited to abuse of these drugs. Two CNS depressants notorious for their roles in date rape are discussed in Box 40–1.
Drug abuse IV: major drugs of abuse other than alcohol and nicotine

Category
Examples
Opioids
Heroin
Morphine
Meperidine
Oxycodone
Hydromorphone
Psychostimulants
Cocaine
Dextroamphetamine
Methamphetamine
Methylphenidate
Depressants
Barbiturates
Amobarbital
Secobarbital
Pentobarbital
Phenobarbital
Benzodiazepines
Diazepam
Flunitrazepam
Lorazepam
Miscellaneous
Alcohol
Methaqualone
Gamma-hydroxybutyrate
Meprobamate
Psychedelics
LSD
Mescaline
Psilocybin
Dimethyltryptamine
Dissociative Drugs
Phencyclidine
Ketamine
Anabolic Steroids
Nandrolone
Oxandrolone
Testosterone
Miscellaneous
Dextromethorphan
Marijuana
Nicotine
Nitrous oxide
Amyl nitrite

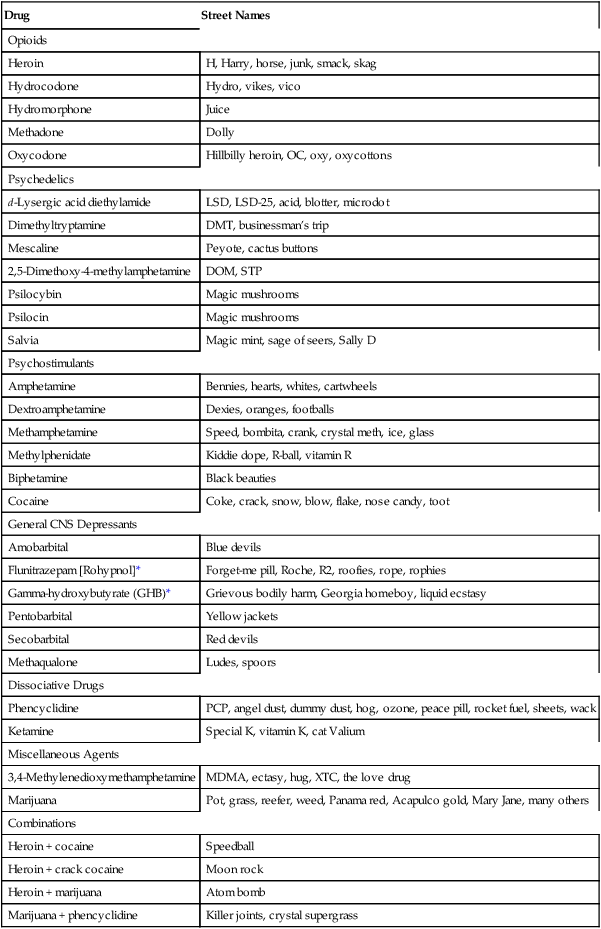
Drug
Street Names
Opioids
Heroin
H, Harry, horse, junk, smack, skag
Hydrocodone
Hydro, vikes, vico
Hydromorphone
Juice
Methadone
Dolly
Oxycodone
Hillbilly heroin, OC, oxy, oxycottons
Psychedelics
d-Lysergic acid diethylamide
LSD, LSD-25, acid, blotter, microdot
Dimethyltryptamine
DMT, businessman’s trip
Mescaline
Peyote, cactus buttons
2,5-Dimethoxy-4-methylamphetamine
DOM, STP
Psilocybin
Magic mushrooms
Psilocin
Magic mushrooms
Salvia
Magic mint, sage of seers, Sally D
Psychostimulants
Amphetamine
Bennies, hearts, whites, cartwheels
Dextroamphetamine
Dexies, oranges, footballs
Methamphetamine
Speed, bombita, crank, crystal meth, ice, glass
Methylphenidate
Kiddie dope, R-ball, vitamin R
Biphetamine
Black beauties
Cocaine
Coke, crack, snow, blow, flake, nose candy, toot
General CNS Depressants
Amobarbital
Blue devils
Flunitrazepam [Rohypnol]*
Forget-me pill, Roche, R2, roofies, rope, rophies
Gamma-hydroxybutyrate (GHB)*
Grievous bodily harm, Georgia homeboy, liquid ecstasy
Pentobarbital
Yellow jackets
Secobarbital
Red devils
Methaqualone
Ludes, spoors
Dissociative Drugs
Phencyclidine
PCP, angel dust, dummy dust, hog, ozone, peace pill, rocket fuel, sheets, wack
Ketamine
Special K, vitamin K, cat Valium
Miscellaneous Agents
3,4-Methylenedioxymethamphetamine
MDMA, ectasy, hug, XTC, the love drug
Marijuana
Pot, grass, reefer, weed, Panama red, Acapulco gold, Mary Jane, many others
Combinations
Heroin + cocaine
Speedball
Heroin + crack cocaine
Moon rock
Heroin + marijuana
Atom bomb
Marijuana + phencyclidine
Killer joints, crystal supergrass
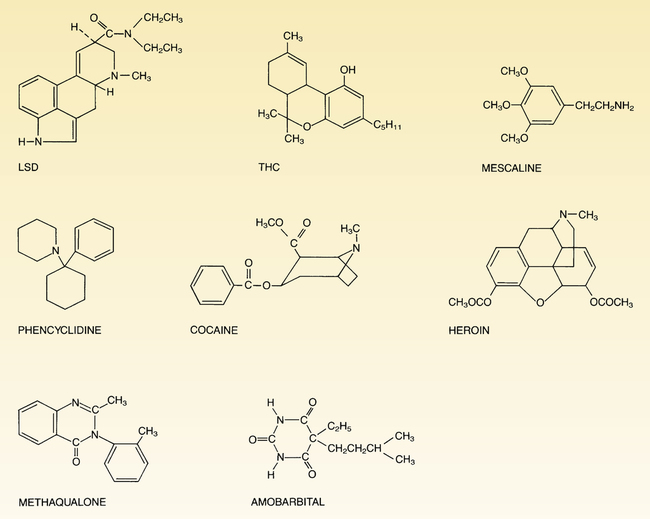
 Structural formulas of representative drugs of abuse.
Structural formulas of representative drugs of abuse.
(LSD = d-lysergic acid diethylamide; THC = tetrahydrocannabinol.)
Heroin, oxycodone, and other opioids
Preferred drugs and routes of administration
Oxycodone.
Tolerance and physical dependence
Treatment of acute toxicity
Drugs for long-term management of opioid addiction

Drug
Trade Name
Formulation
Dosing Schedule
CSA Schedule
Comments
Opioid Agonist
Methadone
Methadose, Diskets
Dispersible tablets used to make an oral suspension
Once a day
II
Methadone maintenance may be provided only by Opioid Treatment Programs certified by the federal Substance Abuse and Mental Health Services Administration and approved by the designated state authority.
Methadose
Concentrated oral liquid
Once a day
Opioid Agonist-Antagonist
Buprenorphine
Subutex
Sublingual tablet
Once a day
III
Subutex and Suboxone may be prescribed in a primary care setting by any physician or nurse practitioner who has received authorized training and has registered with the Substance Abuse and Mental Health Services Administration.
Suboxone*
Sublingual tablet
Once a day
Suboxone*
Sublingual film
Once a day
Probuphine†
Sustained-release subdermal implant
Lasts at least 6 months
Opioid Antagonist
Naltrexone
ReVia
Oral tablet
Once a day
NR
Naltrexone is not a controlled substance and hence prescribers do not require special training or certification. IM naltrexone [Vivitrol] is the only drug approved for opioid addictions that is given monthly, rather than daily. Before receiving naltrexone, patients must undergo opioid detoxification.
Vivitrol
Extended-release suspension for IM injection
Once a month
Buprenorphine.
General CNS depressants
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Drug abuse IV: major drugs of abuse other than alcohol and nicotine
Get Clinical Tree app for offline access

