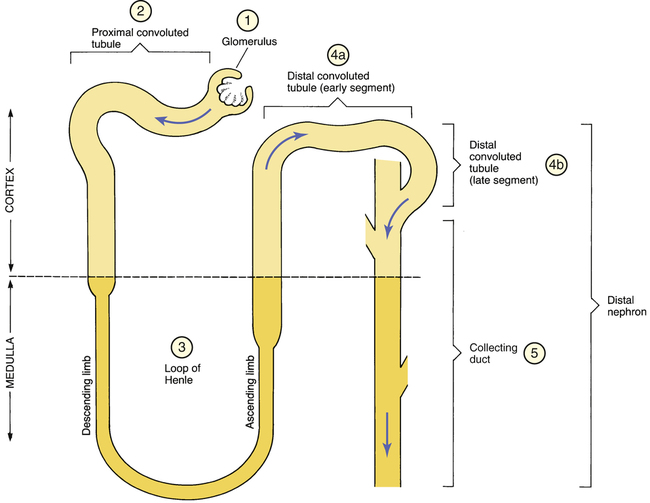
CHAPTER 41 The basic functional unit of the kidney is the nephron. As indicated in Figure 41–1, the nephron has four functionally distinct regions: (1) the glomerulus, (2) the proximal convoluted tubule, (3) the loop of Henle, and (4a, 4b) the distal convoluted tubule. All nephrons are oriented within the kidney such that the upper portion of Henle’s loop is located in the renal cortex and the lower end of the loop descends toward the renal medulla. Without this orientation, the kidney could not produce concentrated urine. In addition to the nephrons, the collecting ducts (the tubules into which the nephrons pour their contents) play a critical role in kidney function. As suggested by Figure 41–1, the final segment of the distal convoluted tubule (4b) plus the collecting duct into which it empties (5) can be considered a single functional unit: the distal nephron. Because most diuretics act by disrupting solute reabsorption, to understand the diuretics, we must first understand the major processes by which nephrons reabsorb filtered solutes. Because sodium and chloride ions are the predominant solutes in the filtrate, reabsorption of these ions is of greatest interest. As we discuss reabsorption, numeric values are given for the percentage of solute reabsorbed at specific sites along the nephron. Bear in mind that these values are only approximate. Figure 41–2 depicts the sites of sodium and chloride reabsorption, indicating the amount of reabsorption that occurs at each site. The proximal convoluted tubule (PCT) has a high reabsorptive capacity. As indicated in Figure 41–2, a large fraction (about 65%) of filtered sodium and chloride is reabsorbed at the PCT. In addition, essentially all of the bicarbonate and potassium in the filtrate is reabsorbed here. As sodium, chloride, and other solutes are actively reabsorbed, water follows passively. Since solutes and water are reabsorbed to an equal extent, the tubular urine remains isotonic (300 mOsm/L). By the time the filtrate leaves the PCT, sodium and chloride are the only solutes that remain in significant amounts. Within the thick segment of the ascending limb of the loop of Henle, about 20% of filtered sodium and chloride is reabsorbed (see Fig. 41–2). Since, unlike the descending limb, the ascending limb is not permeable to water, water must remain in the loop as reabsorption of sodium and chloride takes place. This process causes the tonicity of the tubular urine to return to that of the original filtrate (300 mOsm/L). Aldosterone, the principal mineralocorticoid of the adrenal cortex, stimulates reabsorption of sodium from the distal nephron. At the same time, aldosterone causes potassium to be secreted. Although not directly coupled, these two processes—sodium retention and potassium excretion—can be viewed as an exchange mechanism. This exchange is shown schematically in Figure 41–2. Aldosterone promotes sodium-potassium exchange by stimulating cells of the distal nephron to synthesize more of the pumps responsible for sodium and potassium transport. In addition to the four major categories of diuretics, there is a fifth group: the carbonic anhydrase inhibitors. Although the carbonic anhydrase inhibitors are classified as diuretics, these drugs are employed primarily to lower intraocular pressure (IOP) and not to increase urine production. Consequently, the carbonic anhydrase inhibitors are discussed in Chapter 104 (Drugs for the Eye) rather than here. Furosemide acts in the thick segment of the ascending limb of Henle’s loop to block reabsorption of sodium and chloride (see Fig. 41–2). By blocking solute reabsorption, furosemide prevents passive reabsorption of water. Since a substantial amount (20%) of filtered NaCl is normally reabsorbed in the loop of Henle, interference with reabsorption here can produce profound diuresis. Digoxin is used for heart failure (see Chapter 48) and cardiac dysrhythmias (see Chapter 49). In the presence of low potassium, the risk of serious digoxin-induced toxicity (ventricular dysrhythmias) is greatly increased. Since high-ceiling diuretics promote potassium loss, use of these drugs in combination with digoxin can increase the dysrhythmia risk. This interaction is unfortunate in that most patients who take digoxin for heart failure must also take a diuretic as well. To reduce the risk of toxicity, potassium levels should be monitored routinely, and, when indicated, potassium supplements or a potassium-sparing diuretic should be given.
Diuretics
Review of renal anatomy and physiology
Anatomy
Physiology
Processes of reabsorption that occur at specific sites along the nephron
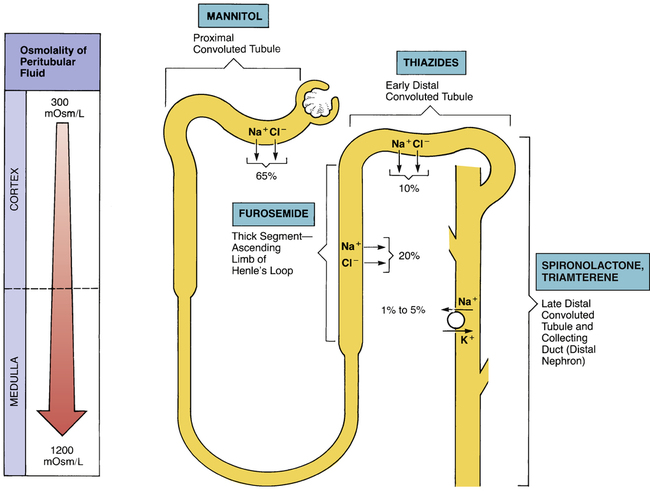
 Schematic diagram of a nephron showing sites of sodium absorption and diuretic action.
Schematic diagram of a nephron showing sites of sodium absorption and diuretic action.
The percentages indicate how much of the filtered sodium and chloride is reabsorbed at each site.
Proximal convoluted tubule.
Loop of Henle.
Distal nephron: late distal convoluted tubule and collecting duct.
Introduction to diuretics
How diuretics work
Classification of diuretics
High-ceiling (loop) diuretics
Furosemide
Mechanism of action
Drug interactions
Digoxin.
Get Clinical Tree app for offline access

Diuretics
Get Clinical Tree app for offline access