Disorders
Acute respiratory distress syndrome
Description
• Severe form of alveolar or acute lung injury resulting in damage to alveolar capillary membrane.
• Pulmonary edema in the absence of cardiac failure.
• Hallmark sign: hypoxemia despite increased supplemental oxygen
• Also called adult respiratory distress syndrome; ARDS; and shock, stiff, wet, or Da Nang lung (see Understanding ARDS)
Causes
Acute miliary tuberculosis
Anaphylaxis
Aspiration of gastric contents
Coronary artery bypass grafting
Disseminated intravascular coagulation
Drug overdose
Idiosyncratic drug reaction
Indirect or direct lung trauma (most common)
Massive blood transfusions
Near drowning
Oxygen toxicity
Pancreatitis
Pulmonary infection
Sepsis
Thoracic trauma
Toxic inhalation of noxious gases and vapors
Venous air embolism, fat embolism
Signs and symptoms
Stage I
Shortness of breath, especially on exertion
Normal to increased respiratory and pulse rates
Anxiety, restlessness
Stage II
Respiratory distress
Thick, frothy sputum; bloody, sticky secretions
Bibasilar crackles
Cool, clammy skin; tachycardia; elevated blood pressure
Stage III
• Respiratory rate more than 30 breaths/minute, productive cough, crackles, and rhonchi
• Tachycardia with arrhythmias, labile blood pressure, pale, cyanotic skin
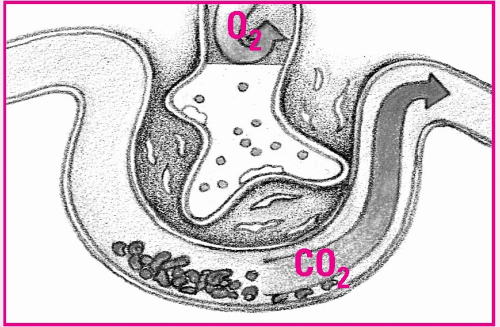
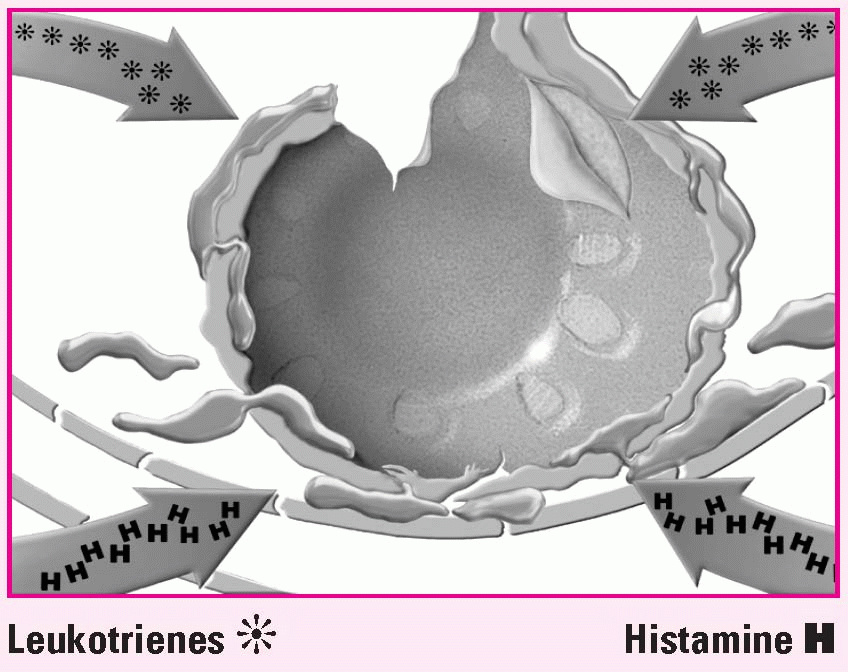
Understanding ARDS
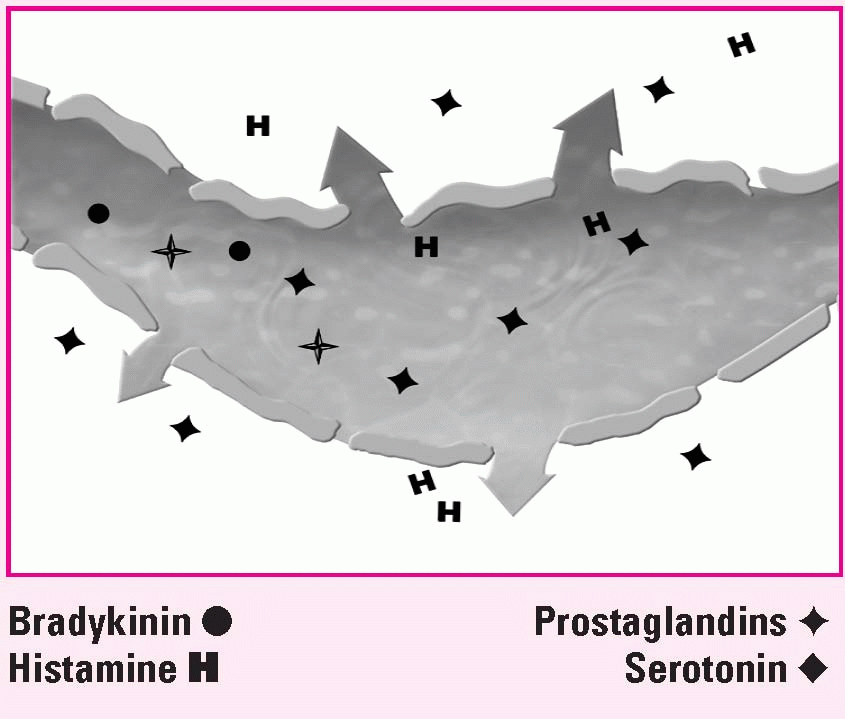
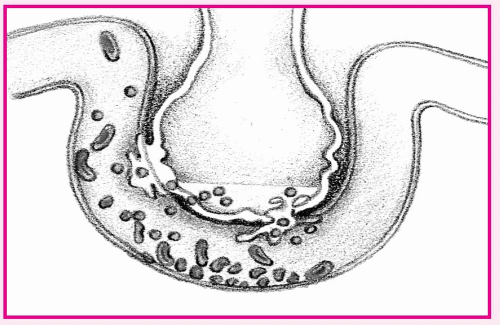
 Phase 1. Injury reduces normal blood flow to the lungs. Platelets aggregate and release neutrophils (N), histamine (H), serotonin (S), and bradykinin (B). |
 Phase 2. The released substances inflame and damage the alveolar capillary membrane, increasing capillary permeability. Fluids then shift into the interstitial space. |
 Phase 3. Capillary permeability increases and proteins and fluids leak out, increasing interstitial osmotic pressure and causing pulmonary edema. |
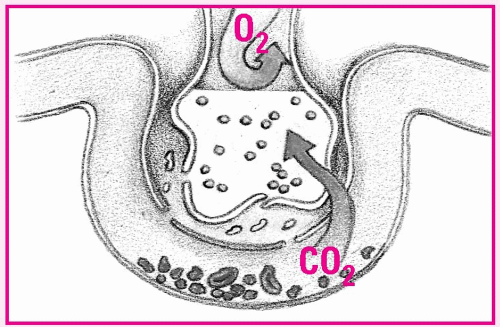 Phase 5. Oxygenation is impaired, but carbon dioxide (CO2) easily crosses the alveolar capillary membrane and is expired. Blood oxygen (O2) and CO2 levels are low. |
• Mental status changes
Stage IV
Acute respiratory failure with severe hypoxia
Metabolic and respiratory acidosis
Deteriorating mental status
Pale, cyanotic skin
Cardiac arrhythmias; hypotension
Potential multi-organ failure
Management
• Oxygen therapy, mechanical ventilation with positive end-expiratory pressure (PEEP)
PEEP may lower cardiac output, so monitor for hypotension, tachycardia, and decreased urine output. To maintain PEEP, suction only as needed.
• Treatment of underlying cause
• Correction of electrolyte and acid-base imbalances
• Fluid restriction
• Tube feedings or parenteral nutrition
• Medications: antimicrobials, bronchodilators, mucolytics, corticosteroids, diuretics, fluids, neuromuscular blockers, opioids, sedatives, and vasopressors
• Frequent repositioning
• Frequent mouth care
Acute respiratory failure
Description
• Inadequate gas exchange and ventilation resulting from the inability of the lungs to adequately maintain arterial oxygenation or eliminate carbon dioxide
Causes
Airway irritants
Bronchospasm
Central nervous system depression
Chronic obstructive pulmonary disease exacerbation
Endocrine or metabolic disorders
Excessive secretions
Fluid overload
Gas exchange failure
Heart failure
Myocardial infarction
Pulmonary emboli
Respiratory tract infection
Thoracic abnormalities
Ventilatory failure
Signs and symptoms
Cyanosis of the oral mucosa, lips, and nail beds
Ashen skin; cold, clammy skin
Use of accessory muscles; pursed-lip breathing
Nasal flaring; rapid breathing
Asymmetrical chest movement
Anxiety, restlessness
Hyperresonance
Diminished or absent breath sounds
Wheezes (with asthma)
Rhonchi (with bronchitis)
Crackles (with pulmonary edema)
Management
• Oxygen therapy with mechanical ventilation
• Fluid restriction (with heart failure)
• Medications: antacids, antibiotics, bronchodilators, corticosteroids, diuretics, histamine-receptor antagonists, positive inotropic drugs, vasopressors
• Frequent repositioning
• Frequent mouth care
Anaphylaxis
Description
• Dramatic, acute atopic reaction to an allergen marked by sudden onset of rapidly progressive urticaria and respiratory distress
• Earlier signs and symptoms more severe after exposure to the antigen
• Severe reactions possibly initiating vascular collapse, leading to systemic shock and, possibly, death (see Understanding anaphylaxis, pages 58 and 59)
Causes
Systemic exposure to:
– blood transfusions
– contrast media
– foods (especially shellfish)
– insect venom
– latex
– other specific antigens
– sensitizing drugs
Signs and symptoms
• Anxiety
• Hives
• Angioedema
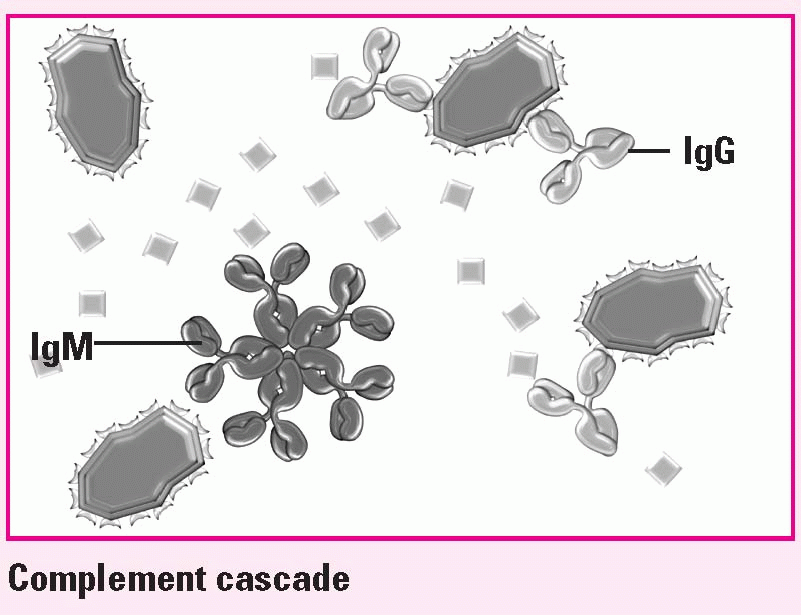
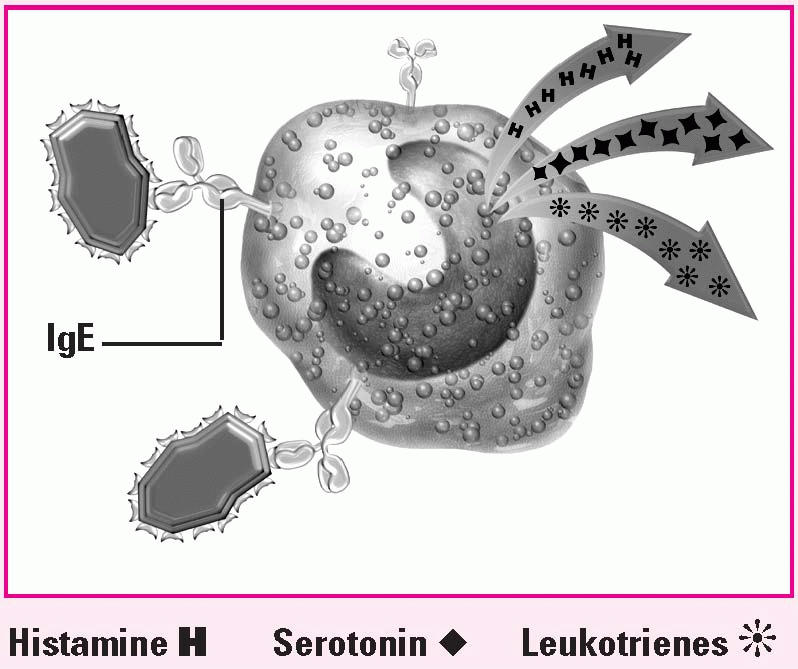
Understanding anaphylaxis
2. Release of chemical mediators
Activated IgE on basophils promotes release of mediators: histamine, serotonin, and leukotrienes.
|
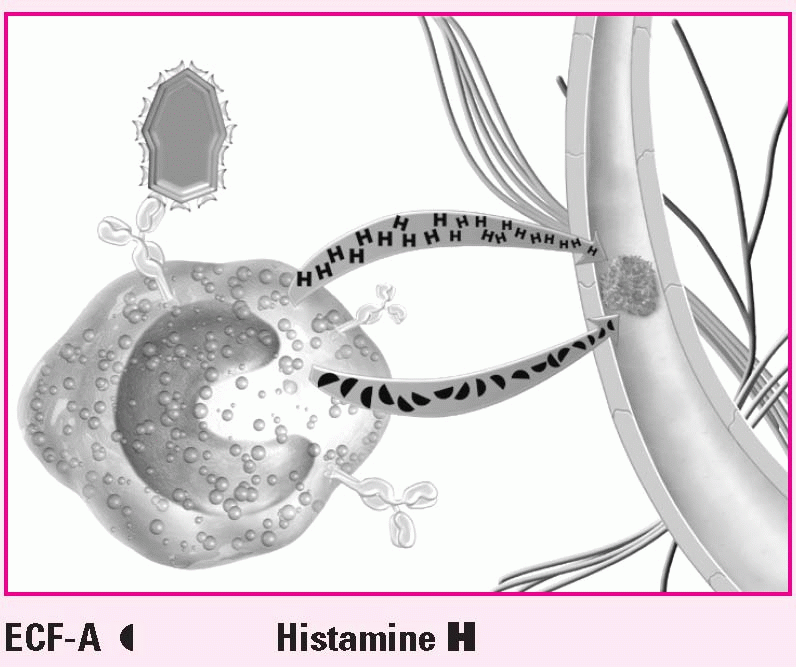
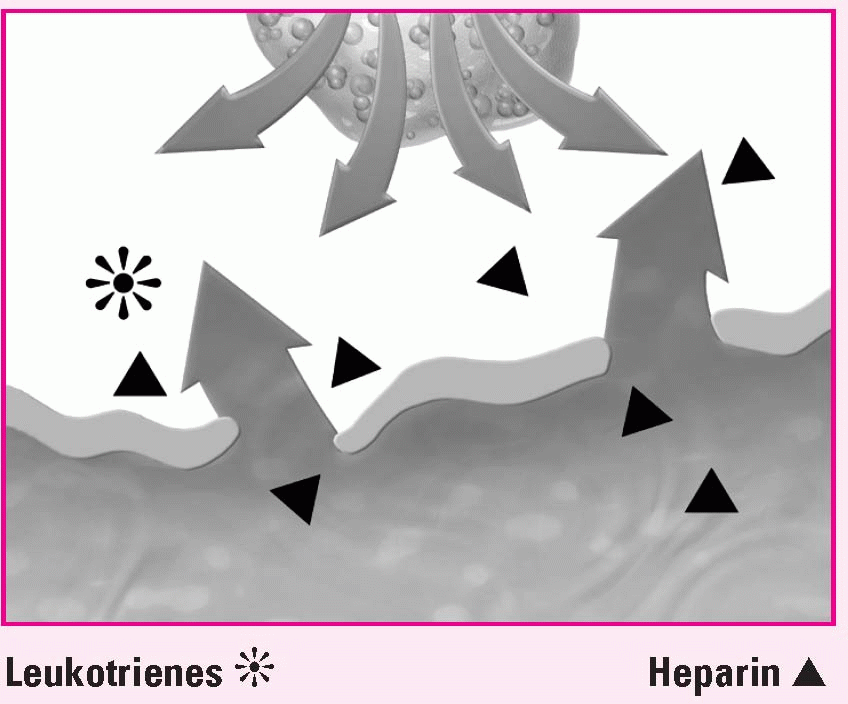
3. Intensified response
Mast cells release more histamine and eosinophil chemotactic factor of anaphylaxis (ECF-A), which create venuleweakening lesions.
|
4. Respiratory distress
In the lungs, histamine causes endothelial cell destruction and fluid leakage into alveoli.
|
5. Deterioration
Meanwhile, mediators increase vascular permeability, causing fluid to leak from the vessels.
|
• Hoarseness or stridor; wheezing
• Severe abdominal cramps, nausea, diarrhea
• Urinary urgency and incontinence
• Altered mental status, dizziness, drowsiness, headache, restlessness, seizures, and unresponsiveness
• Hypotension, shock; sometimes angina and cardiac arrhythmias
Management
• Removal of offending antigen
• Patent airway (establish and maintain); endotracheal intubation or tracheostomy, if indicated
• Cardiopulmonary resuscitation, if cardiac arrest occurs
• Medications: immediate injection of epinephrine 1:1,000 aqueous solution subcutaneously or I.V; corticosteroids; antihistamines, such as diphenhydramine (Benadryl); bronchodilators; volume expander infusions as needed; vasopressors, such as norepinephrine (Levophed), and dopamine (Intropin).
Aneurysm, abdominal aortic
Description
• Abnormal dilation from a weakness in the arterial wall of the aorta, commonly between the renal arteries and iliac branches
• Can be fusiform (spindle-shaped), saccular (pouch like), or dissecting
Causes
Arteriosclerosis or atherosclerosis (95%)
Connective tissue disorders
Hypertension
Syphilis; other infections
Trauma
Signs and symptoms
Intact aneurysm
• Gnawing, generalized, steady abdominal pain; lower back pain unaffected by movement; sudden onset of severe abdominal pain or lumbar pain with radiation to flank and groin
• Gastric or abdominal fullness
• Possible pulsating mass in the periumbilical area
Ruptured aneurysm
• Into the peritoneal cavity: severe, persistent abdominal and back pain; into the duodenum: GI bleeding with massive hematemesis and melena
• Mottled to cyanotic skin, poor distal perfusion, absent peripheral distal pulses
• Decreased level of consciousness, syncope, diaphoresis, hypotension, tachycardia, oliguria
• Distended abdomen, ecchymosis or hematoma in the abdominal, flank, or groin area
• Systolic bruit over the aorta
Management
• Control of hypertension; fluid and blood replacement with rupture
• Medications: analgesics, antibiotics, antihypertensives, beta-adrenergic blockers
• Endovascular grafting or surgical resection for those that produce symptoms; bypass procedures for poor perfusion distal to aneurysm; graft replacement for repair of ruptured aneurysm
If rupture does occur, surgery must be done immediately. A pneumatic antishock garment may be used while transporting the patient to surgery.
After surgery
Pulse assessment
Blood pressure maintenance
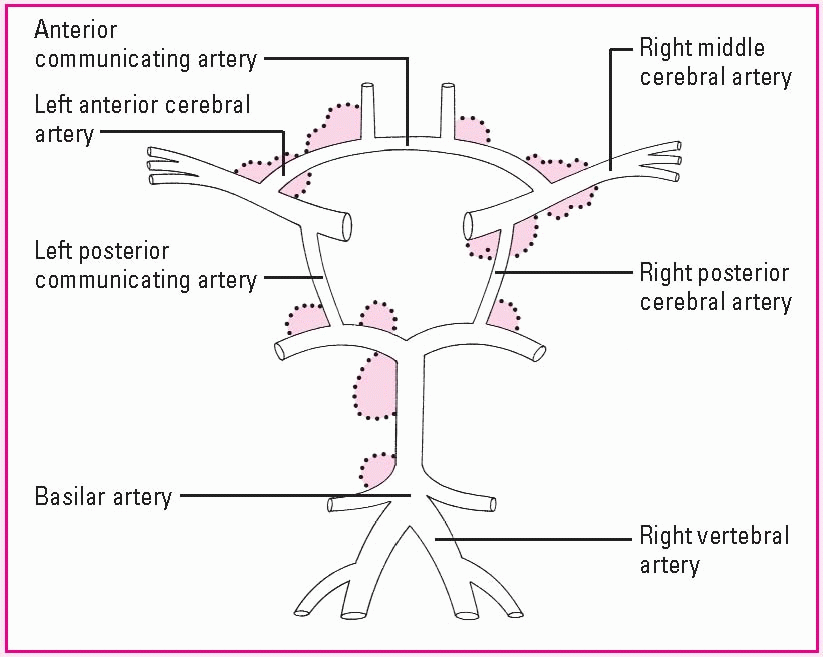
Aneurysm, cerebral
Description
• Weakness in the wall of a cerebral artery causing localized dilation
• Berry aneurysm (most common form); saclike outpouching in a cerebral artery
• Usually occurs at an arterial junction in the Circle of Willis, the circular anastomosis forming the major cerebral arteries at the base of the brain
• Commonly ruptures, causing subarachnoid hemorrhage
Causes
• Congenital defect, degenerative process, or combination (see How a cerebral aneurysm develops, page 62)
• Trauma
Signs and symptoms
• Based on the site and amount of bleeding
• Vision defects
• Grade I (minimal bleeding): no neurologic deficit; possibly having slight headache and nuchal rigidity
How a cerebral aneurysm develops
In an intracranial (cerebral) aneurysm, weakness in the wall of a cerebral artery causes localized dilation. Blood flow exerts pressure against the wall, stretching it like a balloon and making it likely to rupture. Cerebral aneurysms usually arise at the arterial bifurcation in the Circle of Willis and its branches. This illustration shows the most common sites around this circle.
|
• Grade II (mild bleeding): alert with a mild to severe headache and nuchal rigidity; possibly having third-nerve palsy
• Grade III (moderate bleeding): altered mental status, with nuchal rigidity and, possibly, a mild focal deficit
• Grade IV (severe bleeding): stuporous with nuchal rigidity and possibly mild to severe hemiparesis
• Grade V (moribund; commonly fatal): deep coma or decerebrate
Management
• Aneurysm precautions (bed rest in a quiet, darkened room, keeping the head of the bed flat or less than 30 degrees, as ordered; limited visitation; avoidance of strenuous physical activity and straining with bowel movements; and restricted fluid intake)
• Avoidance of coffee, other stimulants, and aspirin
• Medications: aminocaproic acid, analgesics, anticonvulsants, antihypertensives, calcium channel blockers, corticosteroids, sedatives
• Surgical repair by clipping, ligation, or wrapping (before or after rupture)
Arterial occlusive disease
Description
• An obstruction or narrowing of the lumen of the aorta and its major branches; may affect the carotid, vertebral, innominate, subclavian, femoral, iliac, renal, mesenteric, and celiac arteries
• Prognosis dependent on location of the occlusion and development of collateral circulation that counteracts reduced blood flow
Causes
Atheromatous debris (plaques)
Atherosclerosis
Direct blunt or penetrating trauma
Embolism
Fibromuscular disease
Immune arteritis
Indwelling arterial catheter
Raynaud’s disease
Thromboangiitis obliterans
Thrombosis
Signs and symptoms
• Narrowing of lumen may be present; may not cause symptoms
• Trophic changes and diminished or absent pulses of involved arm or leg, pallor with elevation of arm or leg, dependent rubor, ischemic ulcers
• Arterial bruit, hypertension
• Pain, pallor, pulselessness distal to the occlusion, paralysis and paresthesia occurring in the affected arm or leg, poikilothermy
• Sensory or motor deficits, expressive or receptive aphasia, vision disturbances
Management
• General: smoking cessation; hypertension, diabetes, and dyslipidemia control; foot and leg care; weight control; low-fat, low-cholesterol, high-fiber diet; regular walking program
• Medications: anticoagulants, antihypertensives, antiplatelets, hypoglycemics, lipid-lowering drugs, niacin or vitamin B complex, thrombolytics
• Surgery: embolectomy, endarterectomy, atherectomy, laser surgery or angioplasty, endovascular stent placement, percutaneous transluminal angioplasty, patch or bypass grafting, lumbar sympathectomy, amputation, bowel resection
• For chronic arterial occlusive disease use preventive measures, such as minimal pressure mattresses, heel protectors, a foot cradle, or a footboard.
• Preoperative care during an acute episode: circulatory status and pulse monitoring
• Frequent repositioning
• Avoid elevating or applying heat to the affected leg.
After surgery
• Pulse and circulation assessment
• With mesenteric artery occlusion: nasogastric decompression
• Maintaining fluid and electrolyte balance
Cardiac arrhythmias
Description
• Variations in the normal pattern of electrical conduction of the heart
• Vary in severity, from mild, producing no symptoms and requiring no treatment to catastrophic, requiring immediate resuscitation (see Comparing normal and abnormal conduction, pages 66 and 67)
• Classified according to their origin (atrial, junctional, ventricular or supraventricular); clinical significance determined by effect on cardiac output and blood pressure, partially affected by site of origin
Causes
Acid-base imbalances
Cellular hypoxia
Congenital defects
Connective tissue disorders
Degeneration of the conductive tissue
Drug toxicity
Electrolyte imbalances
Emotional stress
Hyperthyroidism
Hypertrophy of the heart muscle
Idiopathic or a combination of causes
Myocardial infarction or ischemia
Organic heart disease
Valvular heart disease
Signs and symptoms
• Circulatory failure along with an absence of pulse and respirations with asystole, ventricular fibrillation and, occasionally, with ventricular tachycardia; reduced urine output
• Pallor, cold and clammy extremities, hypotension
• Dyspnea
• Weakness, chest pain, dizziness, syncope (with severely impaired cerebral circulation)
• Palpitations
Management
• Supportive measures: cardiopulmonary resuscitation, defibrillation, adherence to ACLS protocols
• Medications: antiarrhythmics, electrolyte replacements
• Cardioversion
• Temporary or permanent placement of a pacemaker
• Implantable cardioverter-defibrillator (if indicated)
• Ablation therapy for atrial arrhythmias
• Surgical removal or cryotherapy of an irritable ectopic focus to prevent recurring arrhythmias
• Treatment of the underlying disorder
• ECG monitoring
Cardiac tamponade
Description
• Rapid increase in intrapericardial pressure caused by fluid accumulation in the pericardial sac
• Impaired diastolic filling of the heart (see Understanding cardiac tamponade, page 68)
Causes
Acute myocardial infarction
Acute pericarditis
Acute rheumatic fever (rare)
Bacterial infections
Cardiac catheterization
Cardiac surgery
Chronic renal failure (rare)
Connective tissue disorders (rare)
Drug reaction
Effusion in cancer
Hemorrhage (nontraumatic cause)
Idiopathic
Radiation therapy
Trauma
Thrombolytic therapy
Tuberculosis
Viral pericarditis
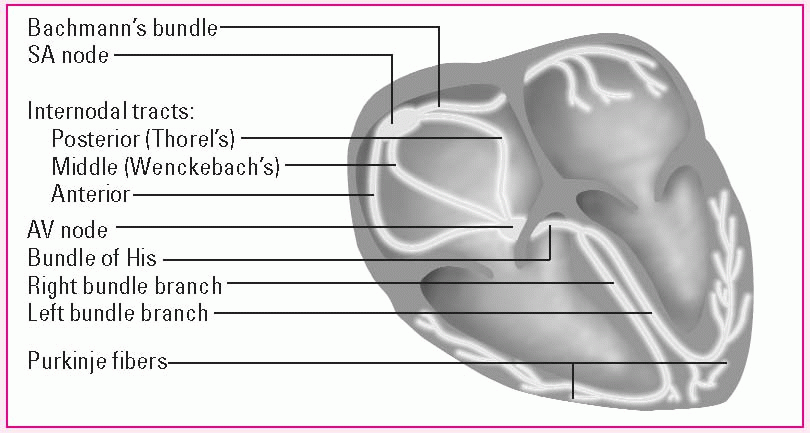
Comparing normal and abnormal conduction
Normal cardiac conduction
The conduction system of the heart, shown below, begins at the heart’s pacemaker, the sinoatrial (SA) node. When an impulse leaves the SA node, it travels through the atria along Bachmann’s bundle and the internodal pathways to the atrioventricular (AV) node and then down the bundle of His, along the bundle branches and, finally, down the Purkinje fibers to the ventricles.
|
Abnormal cardiac conduction
Altered automaticity, irritability, reentry, or conduction disturbances may cause cardiac arrhythmias.
Altered automaticity
Altered automaticity is the result of partial depolarization, which may increase the intrinsic rate of the SA node or latent pacemakers, or may induce ectopic pacemakers to reach threshold and depolarize.
Signs and symptoms
• Anxiety and restlessness, diaphoresis, pallor, or cyanosis
• Beck’s triad (jugular vein distention, hypotension, muffled heart sounds); edema; rapid, weak pulses; increased central venous pressure; pulsus paradoxus; narrow pulse pressure
Automaticity may be altered by such drugs as epinephrine, atropine, and digoxin (Lanoxin), and by such conditions as acidosis, alkalosis, hypoxia, myocardial infarction (MI), hypokalemia, hypermagnesemia, and hypocalcemia. Examples of arrhythmias caused by altered automaticity include atrial fibrillation and flutter, supraventricular tachycardia, ventricular tachycardia and fibrillation, accelerated idioventricular and junctional rhythms, and premature atrial, junctional, and ventricular complexes.
Reentry
Reentry occurs when ischemia or deformation causes an abnormal circuit to develop within conductive fibers. Although current flow is blocked in one direction within the circuit, the descending impulse can travel in the other direction. By the time the impulse completes the circuit, the previously depolarized tissue within the circuit is no longer refractory to stimulation.
Conditions that increase the likelihood of reentry include hyperkalemia, myocardial ischemia, and the use of certain antiarrhythmic drugs. Reentry may be responsible for such arrhythmias as paroxysmal supraventricular tachycardia, ventricular tachycardia, and premature atrial, junctional, and ventricular complexes.
An alternative reentry mechanism depends on the presence of a congenital accessory pathway linking the atria and the ventricles outside the AV junction; for example, Wolff-Parkinson-White syndrome.
Conduction disturbances
Conduction disturbances occur when impulses are conducted too quickly or too slowly. Possible causes include trauma, drug toxicity, myocardial ischemia, MI, and electrolyte abnormalities. The AV blocks occur as a result of conduction disturbances.
• Chest pain
• Hepatomegaly
Management
• Pericardiocentesis, if necessary
• Medications: inotropic drugs, intravascular volume expansion, oxygen
• Surgery: pericardiocentesis, pericardial window, subxiphoid pericardiotomy, complete pericardectomy, thoracotomy
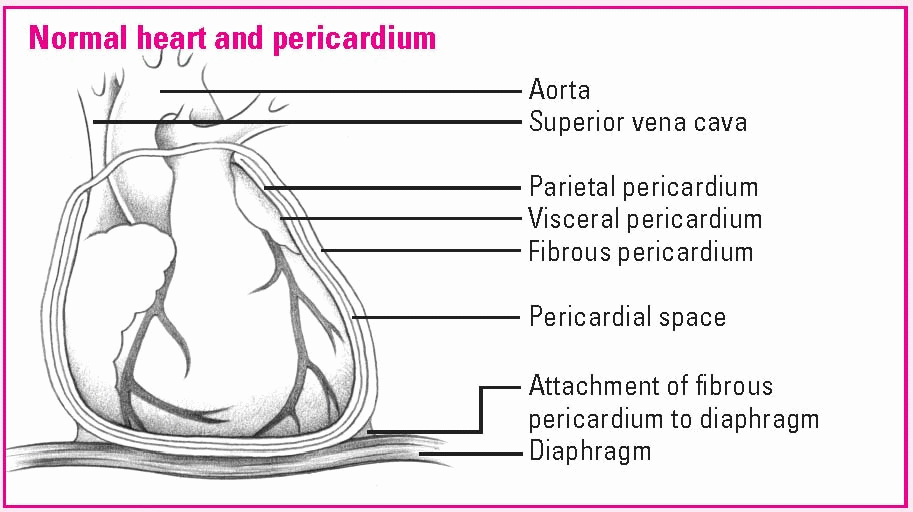
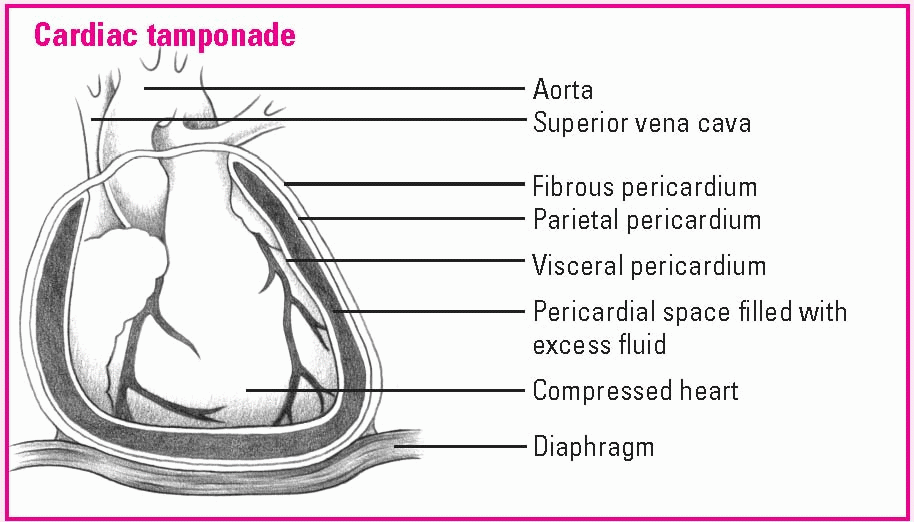
Understanding cardiac tamponade
The pericardial sac, which surrounds and protects the heart, is composed of several layers. The fibrous pericardium is the tough outermost membrane; the inner membrane, called the serous membrane, consists of the visceral and parietal layers. The visceral layer clings to the heart and is also known as the epicardial layer of the heart. The parietal layer lies between the visceral layer and the fibrous pericardium. The pericardial space—between the visceral and parietal layers—contains 10 to 30 ml of pericardial fluid. This fluid lubricates the layers and minimizes friction when the heart contracts.
|
In cardiac tamponade, blood or fluid fills the pericardial space, compressing the heart chambers, increasing intracardiac pressure, and obstructing venous return. As blood flow into the ventricles falls, so does cardiac output. Without prompt treatment, low cardiac output can be fatal.
|
Cerebral contusion
Description
• Ecchymosis of brain tissue resulting from injury to the head
Causes
• Acceleration-deceleration or coup-contrecoup injuries
• Head trauma
Complications may include intracranial hemorrhage, hematoma, tentorial herniation, and increased intracranial pressure (ICP).
Signs and symptoms
• Unconscious patient: pale and motionless; altered vital signs
• Conscious patient: drowsy or easily disturbed
• Scalp wound
• Possible involuntary evacuation of bowel and bladder; hemiparesis
Management
• Establishment of a patent airway and adequate oxygenation and circulation
• Administration of I.V. fluids
Dextrose 5% in water should be avoided because it may increase cerebral edema.
• Minimization of environmental stimuli
• Nothing by mouth until fully conscious
• Medications: nonopioid analgesics
• Surgery: craniotomy, depending on severity or location
• Neurologic status monitoring
• Seizure precautions, if indicated
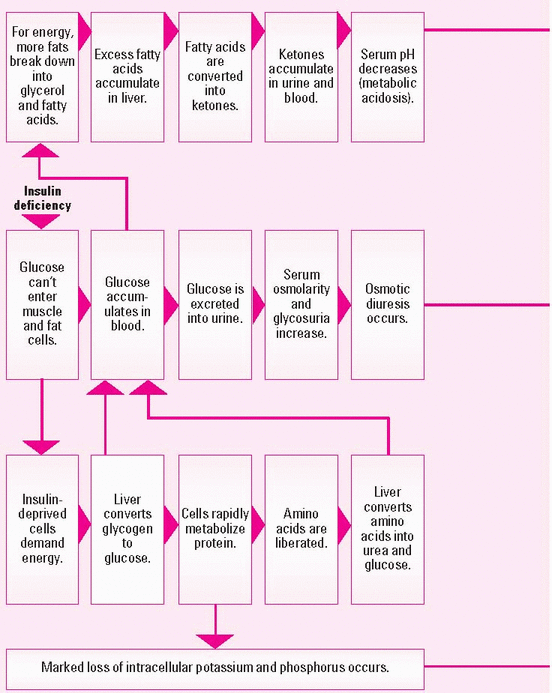
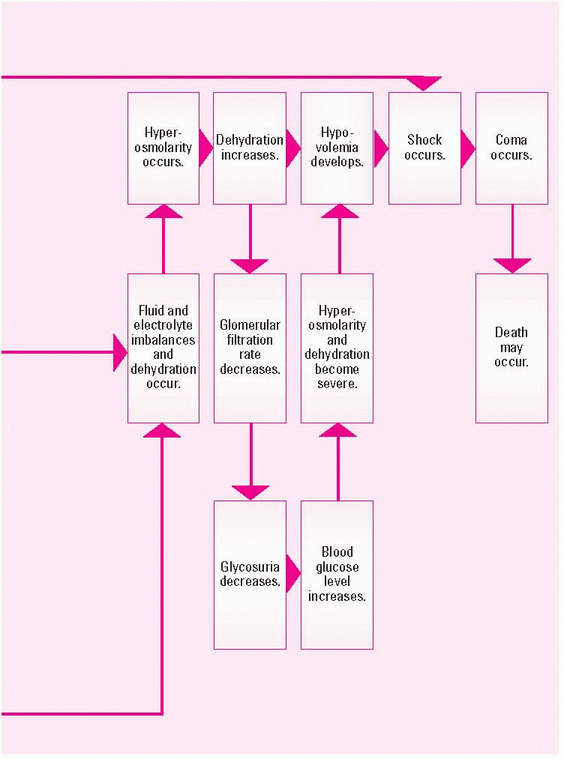
Diabetic ketoacidosis
Description
• Acute complication of hyperglycemic crisis possibly occurring in the patient with diabetes
• If not treated properly, may result in coma or death (see What happens in diabetic ketoacidosis, pages 70 and 71)
• Also called DKA
Causes
• Autoimmune dysfunction
• Failure to take insulin or pump failure for those with insulin pumps
• Illness
• Other endocrine disease
• Recent stress or trauma
• Severe viral infection
• Use of drugs that increase blood glucose levels
Signs and symptoms
• Rapid onset of drowsiness, stupor, and coma
• Polyuria and extreme volume depletion resulting in hypotension, tachycardia, diaphoresis, poor skin turgor, dry mucous membranes, decreased peripheral pulses, cool skin temperature, and decreased reflexes
• Hyperventilation
• Acetone breath odor
• Dry, flushed skin
• Polyuria, polydipsia, polyphagia
Management
• Treatment of underlying cause
• Airway support and mechanical ventilation (for comatose patient)
• Insulin therapy, I.V. and fluid and electrolyte replacements (based on laboratory test results)
Patients with DKA are at high risk for hyperkalemia before treatment due to the movement of potassium out of the cells. After treatment is initiated and potassium begins to move back into the cells, be alert for hypokalemia.
• Fluid resuscitation
• Dietary management, as appropriate
• Medications: oral antidiabetics if stable conversion from insulin
• Blood glucose monitoring
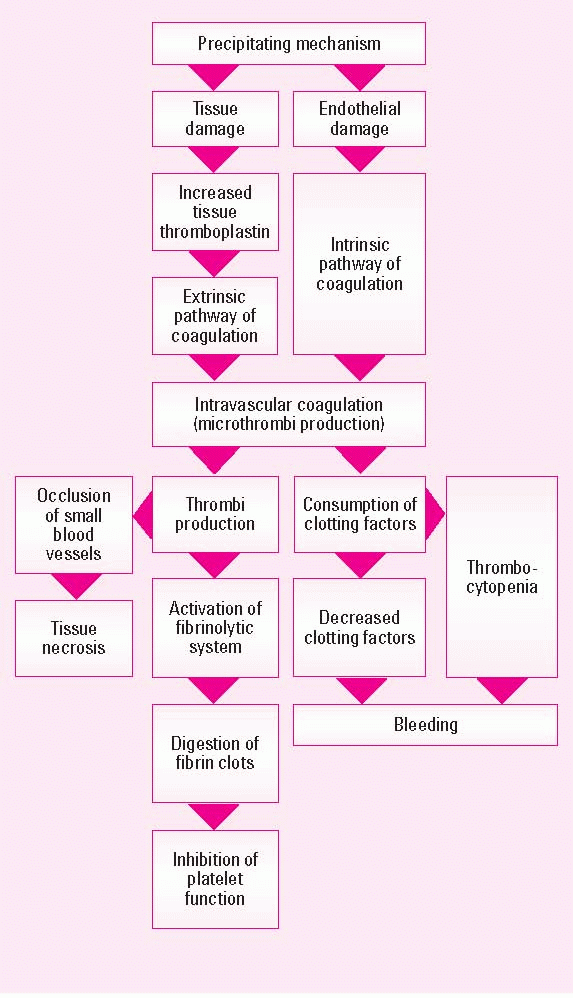
Disseminated intravascular coagulation
Description
• Syndrome of activated coagulation characterized by bleeding, thrombosis, or both
• Complicates diseases and conditions that accelerate clotting, causing occlusion of small blood vessels, organ necrosis, depletion of circulating clotting factors and platelets, and activation of the fibrinolytic system (see How disseminated intravascular coagulation happens)
• Also called DIC, consumption coagulopathy, and defibrination syndrome
Causes
• Acute respiratory distress syndrome
• Cardiac arrest
• Diabetic ketoacidosis
• Disorders that produce necrosis, such as extensive burns and trauma
• Drug reactions
• Heatstroke
• Incompatible blood transfusion
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree