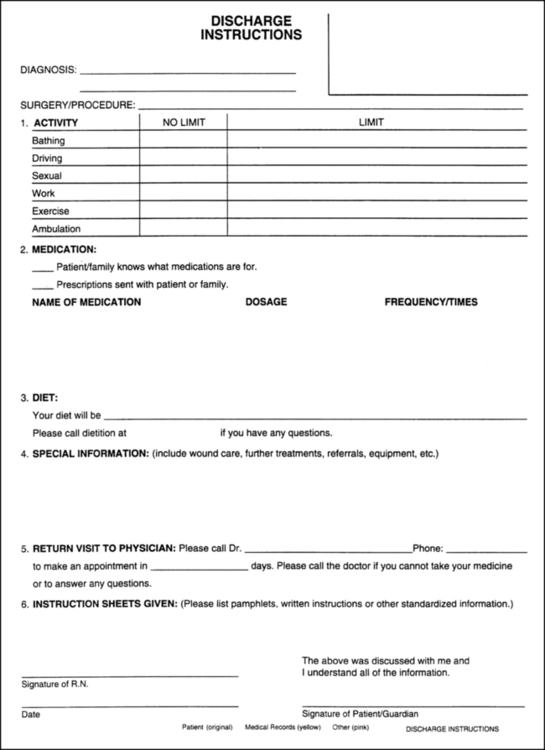
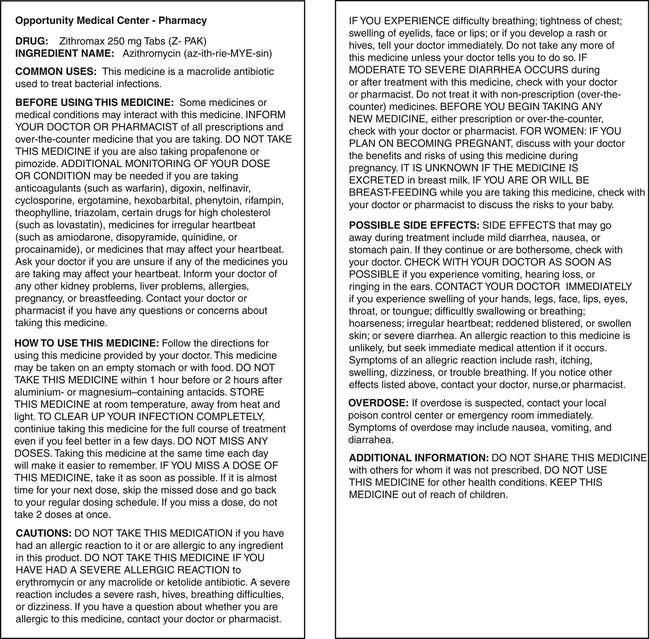
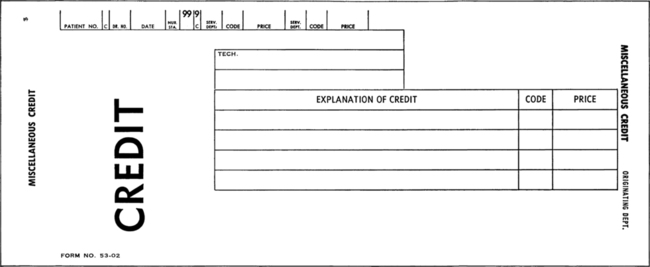
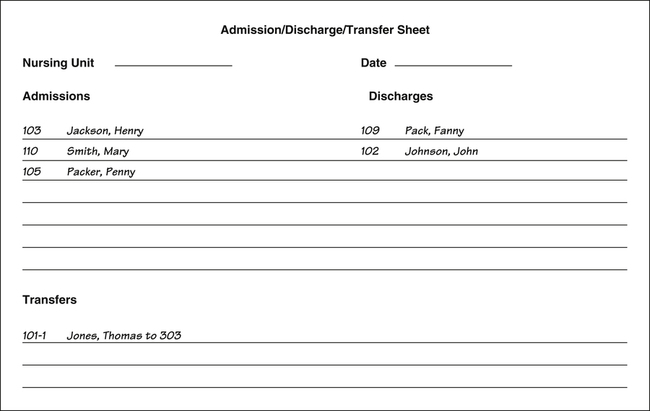
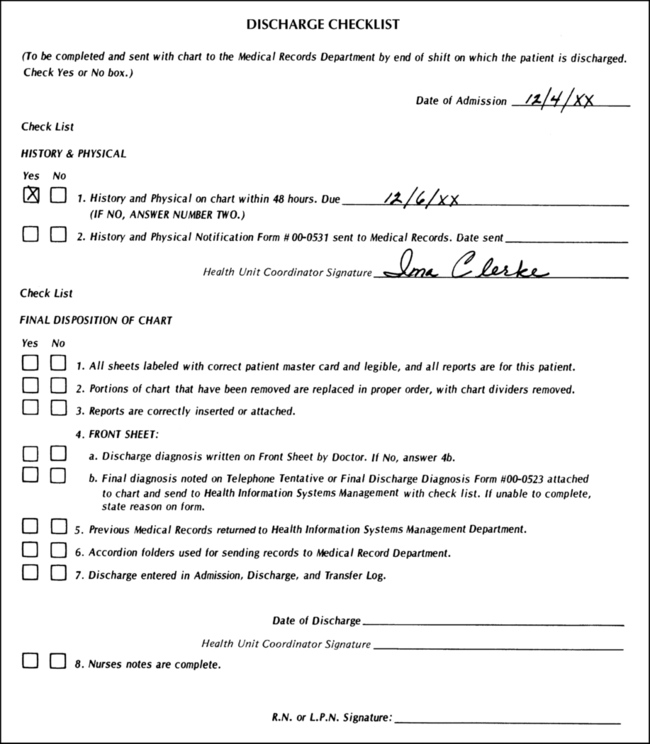
On completion of this chapter, you will be able to: 1. Define the terms in the vocabulary list. 2. Write the meaning of the abbreviations in the abbreviations list. 3. Discuss the purpose of patient discharge planning and patient care conferences, and identify personnel and individuals who would be involved in both. 4. List five types of discharges, and explain the importance of communicating pending discharge information and bed availability to the admitting department or bed placement in a timely manner. 5. List 12 tasks that may be required to complete a routine discharge when paper charts are used. 6. List six additional tasks that may be required when a patient is discharged to another facility and six additional tasks when a patient is discharged home with assistance when paper charts are used. 7. Describe six tasks necessary to prepare the discharged patient’s medical record for the health information management services (HIMS) department when paper charts are used. 8. Explain what the health unit coordinator (HUC) should do when a patient threatens to leave the hospital without a physician’s discharge order. 9. Explain the HUC tasks that may be required and/or requested when a patient dies, and discuss the need for the patient’s death to be verified and the time documented by a doctor or resident. 10. Discuss how the deceased patient is transferred to the morgue, and explain the possible HUC tasks related to the release of remains and organ donation. 11. Explain the usual circumstances regarding a patient’s death that must be met for the patient to be accepted as an organ donor. 12. Explain why an autopsy would be performed and list the circumstances that would define a “coroners case.” 13. List eight tasks performed by the HUC when a patient dies (postmortem) when paper charts are used. 14. List the two primary reasons a doctor would write an order for a patient to be transferred to another room or nursing unit. 15. List nine tasks that are performed when a patient is transferred from one unit to another when paper charts are used. 16. List seven tasks performed by the HUC when a patient is transferred from one room to another room on the same unit when paper charts are used. 17. List seven tasks that are performed by the HUC when a transferred patient is received on the unit when paper charts are used. 18. Discuss the importance of reading the entire set of discharge or transfer orders prior to the patient being discharged or transferred. 19. Describe additional tasks that the HUC may need to carry out to complete a routine discharge procedure when the electronic medical record with computer physician order entry is used. When the EMR is used, the beds are color-coded on the computer census screen as follows: Most discharges from the hospital are routine in nature—that is, the patient is discharged alive to go home in the company of a family member or a friend or alone. See Procedure 20-1 and Figures 20-1 through 20-4.
Discharge, Transfer, and Postmortem Procedures
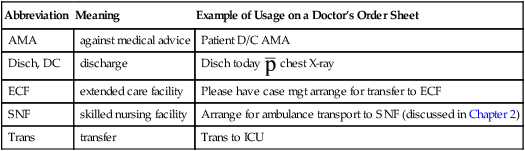
Abbreviation
Meaning
Example of Usage on a Doctor’s Order Sheet
AMA
against medical advice
Patient D/C AMA
Disch, DC
discharge
Disch today  chest X-ray
chest X-ray
ECF
extended care facility
Please have case mgt arrange for transfer to ECF
SNF
skilled nursing facility
Arrange for ambulance transport to SNF (discussed in Chapter 2)
Trans
transfer
Trans to ICU
Discharge of a Patient
Routine Discharge Procedure