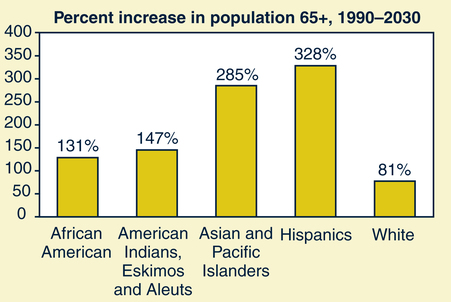
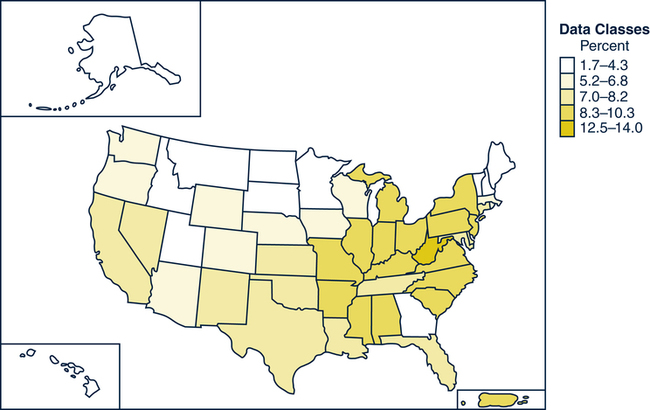
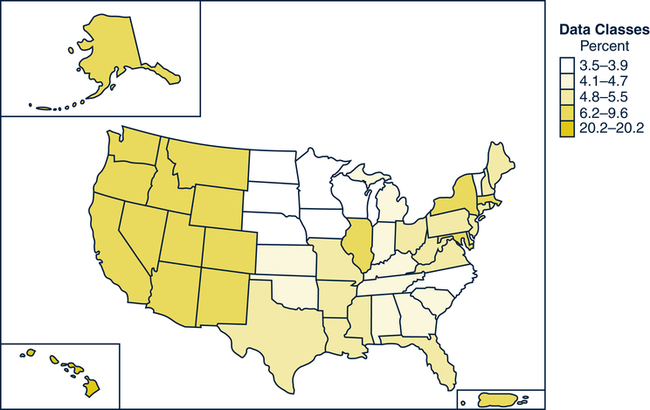
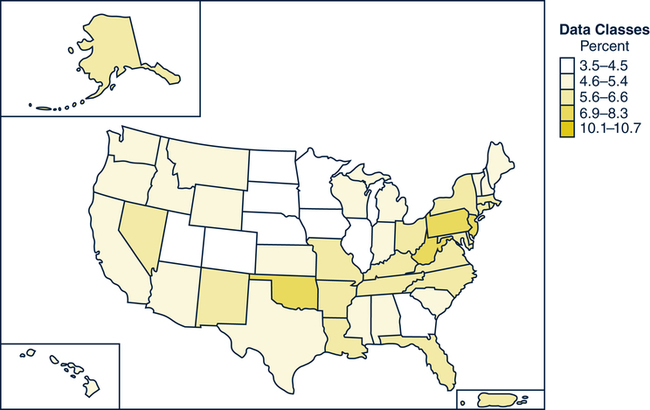
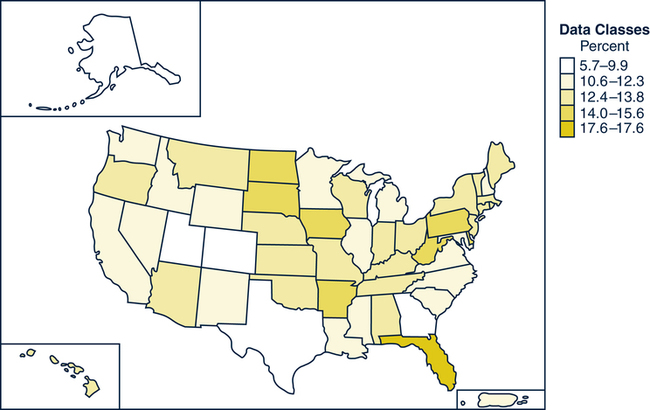
Kathleen F. Jett, BSN, MSN, PhD, GNP-BC On completion of this chapter, the reader will be able to: 1. Discuss the major demographic trends in the United States in relation to the various older adult ethnic populations. 2. Analyze the nursing implications of ethnic demographic changes. 3. Differentiate among culture, ethnicity, and race. 4. Identify potential barriers to care for the ethnic older person. 5. Discuss cultural variations in beliefs about health, illness, and treatment. 6. Describe how differences in cultural patterns may result in a potential conflict between a gerontologic nurse and an older person or his or her family member. 7. Propose how to increase the quality of the interaction between the nurse and the older adult through the nurse’s knowledge of the concept of context as it relates to relationships and behavior. 8. Apply linguistically appropriate techniques in communicating with an ethnic older person. 9. Discuss ways in which planning and implementation of nursing interventions can be adapted to older adults’ ethnicity. Although older adults of color will still be outnumbered by their white counterparts for years to come, tremendous growth is anticipated (Gelfand, 2003). Between 2007 and 2050 the percentage of older African Americans is projected to grow from 8.3% to 11%; Asian/Pacific Islanders from 2.3% to 7.8%; American Indians/Alaskan Natives from 0.6% to 1.0%. Finally, Hispanics of any race will increase from 6.6% to19.8% (Administration on Aging, 2009). By 2030 the number of older Hispanics is expected to be the largest of any other group described as a minority (Fig. 5-1). Adding to the diversity in the United States is the influx of immigrants. The immigrant population is growing at a faster rate than that of the native born. Although access to the United States varies with global politics, older adults are continually being reunited with their adult children; they may live in their adult children’s households, where they assist with homemaking and care for younger children in the family and are cared for in return. It is becoming increasingly common for communities to support senior centers with activities and meals reflective of their diverse participants (McCaffrey, 2007). Certain communities and regions in the United States are decidedly more diverse than others. Figs. 5–2 to 5–5 provide information about the geographic distribution of older persons from each census group. Today and in the future, nurses may provide care to older adults from multiple ethnic groups in the course of a single day. It is likely that many of these elders will not speak the same language as the nurse. The diversity of values, beliefs, languages, and historical life experiences of older adults today challenges nurses to gain new awareness, knowledge, and skills to provide culturally and linguistically appropriate care. When language becomes a barrier to care, working with interpreters may be helpful. To give the most sensitive care it is necessary to step outside of cultural bias and accept that other cultures have different ways of perceiving the world that are as valid as one’s own. Increasing awareness, knowledge, and skills are the tools needed to begin to overcome the barriers to culturally compassionate care and, as a consequence, to reduce health disparities (see Evidence-Based Practice Box). Culture is a universal phenomenon. It is the shared and learned beliefs, expectations, and behaviors of a group of people. Style of dress, food preferences, language, and social systems are expressions of culture. Cultures may share similarities, but no two are exactly alike. Cultural knowledge is transmitted from one member to another through the process called enculturation. It provides individuals with a sense of security and a blueprint for interacting within the family, community, and country. Culture allows members of the group to predict each other’s behavior and respond appropriately, including during one’s own aging and that of community members. Culture is universal, adaptive, and exists at the microlevel of the individual or family and at the macrolevel in terms of a region, country, or a specific group. Review Boxes 5–1 through 5–4. Acculturation is a process that occurs when a member of one cultural group adopts the values, beliefs, expectations, and behaviors of another group, usually in an attempt to become recognized as a member of the new group. Issues surrounding acculturation are particularly relevant for ethnic older persons. Many emigrate to join their children’s families who have established themselves in a new homeland. They may live in ethnically homogeneous neighborhoods of “Little Italy,” “Little Havana,” “Chinatown,” or other locations. They may have little interest or need to adopt the mainstream culture of the new country and may retain practices and expectations of the “old country.” Their children, on the other hand, may live in two cultures, that of their parents and that of the workplace. This phenomenon has produced a considerable amount of intergenerational conflict. The book The Bonesetter’s Daughter by Amy Tan (2002) provides an excellent example of this. Gerontologic nursing care is provided to all persons in all settings, without regard to personal characteristics (see Home Care Box). However, there is evidence of racial and ethnic disparities in health care and health outcomes across the range of illness and services and all age groups (Smedley, Stith, & Nelson, 2003). Socioeconomic factors account for some of these differences, but so do racism and ageism in the health care encounter. Significant for older adults, alarming differences are seen in the rate of angioplasty, use of pain medication, timing of mammograms, and mortality associated with prostate cancer, to name only a few (Betancourt & Maina, 2004; Mudano, Casebeer, & Patino, 2003; Smedley, Stith, & Nelson, 2003). Gerontologic nurses who provide culturally sensitive care can contribute to the reduction of health disparities through awareness of, sensitivity to, and knowledge of, both overt and covert barriers to our caring (Galanti, 2008). Among these barriers are ethnocentrism and racism. Both are triggers to cultural conflict in the nursing situation. In gerontologic nursing the barriers are furthered by ageism.
Cultural Influences
Diversity of the Older Adult Population in the United States
Culturally Sensitive Gerontologic Nursing Care
Cultural Concepts
Cultural Influences
Get Clinical Tree app for offline access