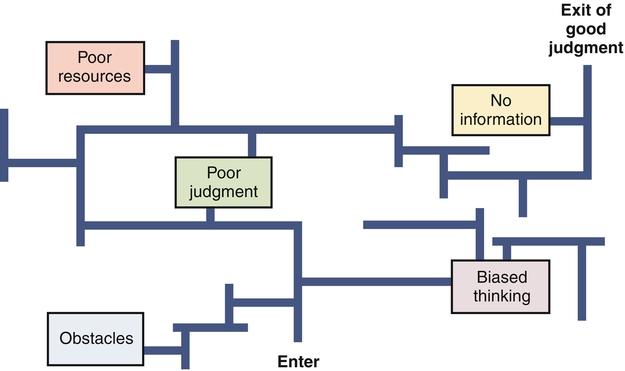
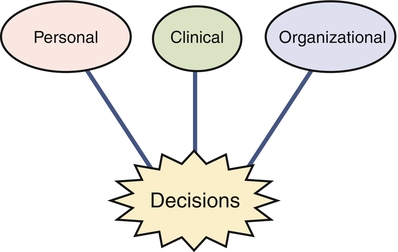
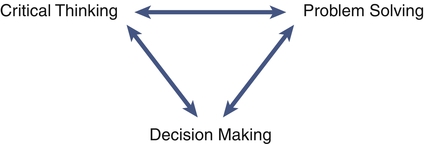
In an era of changing reimbursements, value based purchasing, and expanded roles for nursing in the health care delivery system, critical thinking and decision making are important skills for nurses caring for patients and for nurse leaders and managers. Both the American Nurses Association’s (2009) and American Association of Nurse Executives’ (2005) standards for practice for nurse administrators and executives support the fact that in a fast-paced health care delivery environment, staff nurses, leaders, and managers must be able to analyze and synthesize a large array of information, use critical thinking and decision making skills to deliver effective day to day patient care, and solve complex problems that occur in complex health care delivery systems (see Figure 4-1). Furthermore, the Magnet Hospital initiative and the Institute of Medicine’s (Committee on the Robert Wood Johnson Foundation, 2011) Future of Nursing report highlight the need for nurses to be able to be fully involved and even take the lead in decision making from the unit level to the larger health care delivery system. Nurses are a cadre of knowledge workers within the health care system. As such, they need information, resources, and support from their environment. In fact, the nurse manager’s expertise in critical thinking and shared decision making are essential for creating healthy work environments where quality and effective care can be delivered (Kramer et al., 2010; Zori et al., 2010). Critical thinking and decision-making competences include analytical skills as well as intuition. Just as intuition is part of expert clinical practice (Benner, 1984), intuition plays an important role in developing managerial and leadership expertise (Shirey, 2007). Critical thinking can be defined as a set of cognitive skills including “interpretation, analysis, evaluation, inference, explanation, and self-regulation” (Facione, 2007, p. 1). Using these skills, nurses in direct patient care and leaders and managers can reflect analytically, reconceptualize events, and avoid the tendency to make decisions and problem solve hastily or on the basis of inadequate information. Facione also pointed out that critical thinking is not only a skill but also a disposition that is grounded in a strong ethical component. Critical thinking in nursing can be defined as “purposeful, informed, outcomes focused thinking…[that] applies logic, intuition, creativity and is grounded in specific knowledge, skills, and experience” (Alfaro-LeFevre, 2009, p. 7). Alfaro-LeFevre noted that outcomes-focused thinking helps to prevent, control, and solve problems. Tanner (2000) noted that critical thinking is much more than just the five steps of the nursing process. Problem solving involves moving from an undesirable to a desirable state (Chambers, 2009). Problem solving occurs in a variety of nursing contexts, including direct client care, team-level leadership, and systems-level leadership. Nurses and nurse managers are challenged to move from step-by-step problem-solving techniques to incorporating creative thinking, which involves considering the context when meeting current and future challenges in health care delivery (Chambers, 2009; Rubenfeld & Scheffer, 2006). Decision making is the process of making choices that will provide maximum benefit (Drummond, 2001). Decision making can also be defined as a behavior exhibited in selecting and implementing a course of action from alternative courses of action for dealing with a situation or problem. It may or may not be the result of an immediate problem. Critical thinking and effective decision making are the foundation of effective problem solving. If problems require urgent action, then decisions must be made rapidly; if solutions do not need to be identified immediately, decision making can occur in a more deliberative way. Because problems change over time, decisions made at one point in time may need to be changed (Choo, 2006). For example, decisions about how to staff a unit when a nurse calls in sick have to be made immediately. However, if a unit is chronically short-staffed, a decision regarding long-term solutions will have to be made. The process of selecting one course of action from alternatives forms the basic core of the definition of decision making. Choo (2006) noted that all decisions are bounded by cognitive and mental limits, how much information is processed, and values and assumptions. In other words, no matter the decision-making process, all decisions are limited by a variety of known and unknown factors. In a chaotic health care delivery environment, where regulations and standards of care are always changing, any decision may cause an unanticipated future problem. Critical thinking is both an attitude toward handling issues and a reasoning process. Critical thinking is not synonymous with problem solving and decision making (Figure 4-1), but it is the foundation for effective decision making that helps to solve problems (Fioratou et al., 2011). Figure 4-2 illustrates the way obstacles such as poor judgment or biased thinking create detours to good judgment and effective decision making. Critical thinking helps overcome these obstacles. Critical thinking skills may not come naturally. The nurse who is a critical thinker has to be open-minded and have the ability to reflect on present and past actions and to analyze complex information. Nurses who are critical thinkers also have a keen awareness of their surroundings (Fioratou et al., 2011). Critical thinking is a skill that is developed for clarity of thought and improvement in decision-making effectiveness. The roots of the concept of critical thinking can be traced to Socrates, who developed a method of questioning as a way of thinking more clearly and with greater logical consistency. He demonstrated that people often cannot rationally justify confident claims to knowledge. Confused meanings, inadequate evidence, or self-contradictory beliefs may lie below the surface of rhetoric. Therefore it is important to ask deep questions and probe into thinking sequences, seek evidence, closely examine reasoning and assumptions, analyze basic concepts, and trace out implications. Other thinkers, such as Plato, Aristotle, Thomas Aquinas, Francis Bacon, and Descartes, emphasized the importance of systematic critical thinking and the need for a systematic disciplining of the mind to guide it in clarity and precision of thinking. In the early 1900s, Dewey equated critical thinking with reflective thought (The Critical Thinking Community, 2008). Critical thinking, then, is characterized by thinking that has a purpose, is systematic, considers alternative viewpoints, occurs within a frame of reference, and is grounded in information (The Critical Thinking Community, 2008). Questioning is implicit in the critical thinking process. The following are some of the questions to be asked when thinking critically about a problem or issue (Elder & Paul, n.d.): • What is the question being asked? • Is there another question that must be answered first? • Given the information, what conclusions are justified? No matter what questions are asked, critical thinkers need to know the “why” of the thinking, the mode of reasoning (inductive or deductive), what the source and accuracy of the information is, what the underlying assumptions and concepts are, and what might be the outcome of the thinking (The Critical Thinking Community, 2008). Nurses in clinical practice continually make judgments and decisions based on the assessment and diagnosis of client needs and practice problems or situations. Clinical judgment is a complex skill grounded in critical thinking. Clinical judgment results in nursing actions directed toward achieving health outcomes (Alfaro-LeFevre, 2009). Scheffer and Rubenfeld (2000) have stated that habits of the mind that are characteristic of critical thinking by nurses include confidence, contextual perspective, creativity, flexibility, inquisitiveness, intellectual integrity, open-mindedness, perseverance, and reflection. Emphasizing the value of expert experience and holistic judgment ability, Benner (2003) cautioned that clinical judgments must not rely too heavily on technology and that the economic incentives to use technology must not come at the expense of human critical thinking and reasoning in individual cases. Critical thinkers have been distinguished from traditional thinkers in nursing. A traditional thinker, thought to be the norm in nursing, preserves status quo. Critical thinkers go beyond the step-by-step processes outlined in the nursing process and traditional problem solving. A critical thinker challenges and questions the norm and considers in the context of decision making potential unintended consequences. Unlike traditional thinkers, critical thinkers are creative in their thinking and anticipate the consequences of their thinking (Rubenfeld & Scheffer, 2006). Creativity is necessary to deal with the complex twenty-first century health care delivery environment. Nurse leaders and managers have an obligation to create care delivery climates that promote critical thinking, which leads to innovative solutions to problems within the system of care (Committee on the Robert Wood Johnson Foundation Initiative on the Future of Nursing, at the Institute of Medicine; Institute of Medicine, 2011; Porter-O’Grady, 2011). Such a climate encourages deep reflection, especially so that nurses feel safe to learn from mistakes, and encourages nurses to ask questions and consider a variety of viewpoints and alternative solutions to problems. What specific strategies can be used to promote a climate in which critical thinking is fostered? First and foremost, the nurse manager/leader, in the role of mentor, coach, or preceptor, should encourage questions such as “Is what you are doing or proposing based on sound evidence?” (Ignatavicius, 2008). However, Snowden and Boone (2007) cautioned that “best practice, by definition is past practice” (p. 71). Therefore use of best practices needs to be examined carefully in order to use them appropriately. Staff nurses and managers must use critical thinking skills in order to determine the appropriateness of implementing recommended practice protocols. As managers, allowing staff and self “think time” is essential for reflection and is a key component of critical thinking (Zori & Morrison, 2009). Nurse managers’ critical thinking abilities promotes a positive practice environment which can lead to better patient outcomes (Zori, Nosek, & Musil, 2010). Coaching new and experienced nurses to develop expertise in clinical judgment is critically important. Many new nurses, in particular, need to further develop their critical thinking skills (Fero et al., 2008; Forneris & Peden-McAlpine, 2009). In addition to having preceptors and others ask questions of new nurses, nurse managers and leaders can use other strategies to enhance critical thinking in nursing staff. Developing concept maps is another useful strategy to promote critical thinking. Although typically used in prelicensure programs (Ellermann et al., 2006), nurse managers can encourage their preceptors to use concept maps with orientees (Toofany, 2008). Developing concept maps in concert with others further develops a nurse’s critical thinking through the process of dialogue. Simulations also promote critical thinking or “thinking like a nurse” (Tanner, 2006). According to Tanner, simulations can promote clinical reasoning, which leads to making conclusions in the form of clinical judgments and, thus, effective problem solving. The use of human patient simulators is well known in educational settings. Simulators may also be useful in orienting new graduates to the acute care setting (Leigh, 2011). Pulman and colleagues (2009) have reported on the use of simulators to promote critical thinking role development in inter-professional environments. Decision making is the essence of leadership and management. It is what leaders and managers are expected to do (Keynes, 2008). Thus decisions are visible outcomes of the leadership and management process. The effectiveness of decision making is one criterion for evaluating a leader or manager. Yet staff nurses and nurse managers and leaders must make decisions in uncertain and complex environments (Clancy & Delaney, 2005). Within a climate of uncertainty and complexity, nurse managers and leaders must also understand that all decision making involves high-stakes risk taking (Clancy & Delaney, 2005; Keynes, 2008). If poor decisions are made, progress can be impeded, resources wasted, harm caused, and a career adversely affected. The results of poor decisions may be subtle and not appear until years later. Take, for instance, a decision to reduce expenses by decreasing the ratio of registered nurses to nurses’ aides. There may be a short-term cost savings, but if not implemented appropriately, this tactic may result in the gradual erosion of patient care over time (Kane et al., 2007). Unintended effects may include higher turnover of experienced nurses, increased adverse events such as medication errors, decreased staff morale, and lower patient satisfaction scores. The long-term outcome of this decision may actually result in increased expenses not reduced expenses. Thus it is vital for nurses to understand decision making and explore styles and strategies to enhance decision-making skills. Decision making, like traditional problem solving, has been traditionally thought of as a process with identifiable steps yet influenced by the context and by whether there is an intuitive grasp of the situation. However, Effken and colleagues (2010) stated that decision making is much more. Nurses make decisions in personal, clinical, and organizational situations and under conditions of certainty, uncertainty, and risk. Various decision-making models and strategies exist. Nurses’ control over decision making may vary as to amount of control and where in the process they can influence decisions. Although decision-making is more than a step-by-step process as noted by Effken and colleagues (2010), awareness of the components, process, and strategies of decision making contributes to effectiveness in nursing leadership and management decision making. The basic elements of decision making, which enhances day to day activities, contributes to strategic planning and solves problems can be summarized into the following two parts: (1) identifying the goal for decision-making, and (2) making the decision. According to Guo (2008, p. 120), the steps of the decision-making process can be illustrated as follows, using DECIDE: • Define the problem and determine why anything should be done about it and explore what could be happening. • Establish desirable criteria for what you want to accomplish. What should stay the same and what can be done to avoid future problems? • Consider all possible alternative choices that will accomplish the desired goal or criteria for problem solution. • Identify the best choice or alternative based on experience, intuition, experimentation. • Develop and implement an action plan for problem solution. • Evaluate decision through monitoring, troubleshooting, and feedback. Whether nurse managers are the sole decision makers or facilitate group decision making, all the factors that influence the problem-solving process also impact how decisions are made: who owns the problem that will result in a decision, what is the context of the decision to be made, and what lenses or perspectives influence the decision to be made? For example, the chief executive officer may frame issues as a competitive struggle not unlike a sports event. The marketing staff may interpret problems as military battles that need to be won. Nurse executives may view concerns from a care or family frame that emphasizes collaboration and working together. Learning and understanding which analogies and perspectives offer the best view of a problem or issue are vital to effective decision making. It may be necessary for nurse managers to expand their frame of reference and be willing to consider even the most outlandish ideas. Obviously, it is important to begin the goal definition phase with staff members who are closest to the issue. That includes staff nurses in concert with their managers. Often, decisions can originate within the confines of the shared governance system that may be in place within an organization (Dunbar et al., 2007). It is wise, also, to consider adding individuals who have no connection with the issue whatsoever. Often it is these “unconnected” staff members who bring new decision frames to the meeting and have the most unbiased view of the problem. One of the core competencies for all health professionals is working in interprofessional teams (Interprofessional Education Collaborative Expert Panel, 2011). Therefore using interprofessional teams for problem solving and decision making can be assumed to be more effective than working in disciplinary silos. No matter who is involved in the decision-making process, the basic steps to arrive at a decision to resolve problems remain the same. One critical aspect to note, however, is that in making decisions, nurse managers must have situational awareness (Sharma & Ivancevic, 2010). That is, decision makers must always consider the context in which the outcome of the decision is to occur. A decision that leads to a desired outcome on one patient care unit may lead to undesirable outcomes on another unit because the patient care environment and personnel are different. When looking at outcomes, one critical aspect of decision making is to determine the desired outcome. The desired outcome may vary, according to Guo (2008), from an ideal or short-term resolution to covering up a situation. What is desired may be (1) for a problem to go away forever, (2) to make sure that all involved in this problem are satisfied with the solution and gain some benefit from it, or (3) to obtain an ideal solution. Sometimes a quick decision is desired, and researching different aspects of the problem or allowing for participation in decision making is not appropriate. For example, in disaster management, the nurse leader will use predetermined procedures for determining roles of the various personnel involved (Coyle et al., 2007). Desired decisions can be categorized into two end points: minimal and optimal. A minimal decision results in an outcome that is sufficient, satisfies basic requirements, and minimally meets desired objectives. This is sometimes called a “satisficing” decision. An optimizing decision includes comparing all possible solutions with desired objectives and then selecting the optimal solution that best meets objectives (Choo, 2006; Guo, 2008). In addition to these two strategies, Layman (2011) drawing from Etzioni (1986), discussed two other strategies: mixed scanning and incrementalism. Incrementalism is slow progress toward an optimal course of action. Mixed scanning combines the stringent rationalism of optimizing with the “muddling through” approach of incrementalism to form substrategies. Optimizing has the goal of selecting the course of action with the highest payoff (maximization). Limitations of time, money, or people may prevent the decision maker from selecting the more deliberative and slower process of optimizing. Still, the decision maker needs to focus on techniques that will enhance effectiveness in decision-making situations. Barriers to effective decision making exist and, once identified, can lead to going back through the decision-making process. Flaws in thinking can create hidden traps in decision making. These are common psychological tendencies that create barriers or biases in cognitive reflection and appraisal. Six common distortions are as follows (Hammond et al., 1998; 2006): 1. Anchoring trap: When a decision is being considered, the mind gives a disproportionate weight to the first information it receives. Past events, trends, and numbers outweigh current and future realities. All individuals have preconceived notions and biases that influence decisions in a variety of ways. For instance the Institute of Medicine (IOM, 2001) endorsed the use of computerized physician order entry (CPOE) as one solution to reduce medication errors. Furthermore, The Centers for Medicare and Medicaid Services has set forth meaningful use criteria for implementation of CPOE as well as electronic health records (EHR). Despite incentive payments for implementing EHR (HFMA P & P Board, 2012), the financial costs involved, human-factor errors and work-flow issues can hamper successful implementation (Campbell et al., 2006). 2. Status-quo trap: Decision makers display a strong bias toward alternatives that perpetuate the status quo. In the face or rapid change in the environment, past practices that exhibit any sense of permanence provide managers with a feeling of security. 3. Sunk-cost trap: Past decisions become sunk costs, and new choices are often made in a way that justifies past choices. This may result in becoming trapped by an escalation of commitment. Because of rapid, ongoing advances in medical technology, managers are frequently pressured to replace existing equipment before it is fully depreciated. If the new equipment provides a higher level of quality at a lower cost, the sunk cost of the existing equipment is irrelevant to the decision-making process. However, managers may delay purchasing new equipment and forgo subsequent savings because the equipment has yet to reach the end of its useful life. 4. Confirming-evidence trap: Kahneman and colleagues (2011) noted that decision makers also fall into the trap of confirmation bias where contradictory data are ignored. This bias leads people to seek out information that supports an existing instinct or point of view while avoiding contradictory evidence. A typical example is favoring new technology over less glamorous alternatives. A decision maker may become so enamored by technological solutions (and slick vendor demonstrations) that he or she may unconsciously decide in favor of these systems even though strong evidence supports implementing less costly solutions first. 5. Framing trap: The way a problem is initially framed profoundly influences the choices made. Different framing of the same problem can lead to different decision responses. A decision frame can be viewed as a window into the varied reasons a problem exists. As implied by the word frame, individuals may perceive problems only within the boundaries of their own frame. The human resources director may perceive a staffing shortage as a compensation problem, the chief financial officer as an insurance reimbursement issue, the director of education as a training issue, and the chief nursing officer as a work environment problem. Obviously all these issues may contribute, in part, to the problem; however, each person, in looking through his or her individual frame, sees only that portion with which he or she is most familiar (Layman, 2011). 6. Estimating and forecasting traps: People make estimates or forecasts about uncertain events, but their minds are not calibrated for making estimates in the face of uncertainty. The notion that experience is the parent of wisdom suggests that mature managers, over the course of their careers, learn from their mistakes. It is reasonable to assume that the knowledge gained from a manager’s failed projects would be applied to future decisions. Whether right or wrong, humans tend to take credit for successful projects and find ways to blame external factors on failed ones. Unfortunately, this form of overconfidence often results in overly optimistic projections in project planning. This optimism is usually buried in the analysis done before ranking alternatives and recommendations. Conversely, excessive cautiousness or prudence may also result in faulty decisions. This is called aversion bias (Kahneman et al., 2011). Dramatic events may overly influence decisions because of recall and memory, exaggerating the probability of rare but catastrophic occurrences. It is important that managers objectively examine project planning assumptions in the decision-making process to ensure accurate projections. Because misperceptions, biases, and flaws in thinking can influence choices, actions related to awareness, testing, and mental discipline can be employed to ferret out errors in thinking before the stage of decision making (Hammond et al., 1998). Data-driven decision making is important (Dexter et al., 2011; Lamont, 2010; Mick, 2011). The electronic health record can be mined for valuable data, upon which fiscal, human resource, and patient care decisions can be made. However, the data derived can be overwhelming and cause decision makers to make less than optimal decisions. Shared decision making can help ameliorate decision traps (Kahneman et al., 2011) because dissent within the group may help those accountable for the decision to prevent errors that are “motivated by self-interest” (p. 54). More alternatives can be generated by a group and more data can be gathered upon which to base the decision, rather than just using data that is more readily apparent. The situations in which decisions are made may be personal, clinical, or organizational (Figure 4-3). Personal decision making is a familiar part of everyday life. Personal decisions range from multiple small daily choices to time management and career or life choices. Clinical decision making in nursing relates to quality of care and competency issues. According to Tanner (2006), decision making in the clinical arena is called clinical judgment. In nursing, as with all health professions, clinical judgments should be patient-centered, use available evidence from research and other sources, and use available informatics tools (IOM, 2003). These crucial judgments should take place within the context of interprofessional collaboration. Within a hospital or other health care agency, a social network forms that is interprofessional (Tan et al., 2005). This social network has to collaborate for positive change within the organization and to make clinical decisions of the highest quality. Readily accessible information related to evidence-based practice and information gleaned from human resources records and clinical systems can overwhelm nurse managers and leaders. Nurse leaders are coming to understand that innovation and new technology are the driving forces behind the discovery of new knowledge and improvements in patient care. Overlapping, unclear, and changing roles for nurses as a result of new technology and services create complex decision-making situations and impact the quality of care delivered (IOM, 2003). In addition, workflow interruptions can inhibit critical thinking, particularly in a chaotic environment (Cornell et al., 2011; Sitterding et al., 2012). According to Choo (2006), organizations use information to “make decisions that commit resources and capabilities to purposeful action” (p. 1). Nurse managers, for example, make staffing decisions and thus commit financial resources for the purpose of delivering patient care. Hospital administrators may decide to add additional services to keep up with external forces. These decisions subsequently have financial implications related to reimbursement, staffing, and the like. Etzioni (1989) noted that the traditional model for business decisions was rationalism. However, he further asserted that as information flow became more complex and faster-paced, a new decision-making model based on the use of partial information that has not been fully analyzed had begun to evolve. He called this model “humble decision making.” This approach arises in response to the need to make a decision when the amount of data exceeds the time available to analyze it. For instance, predicting the outcome of clinical and administrative decisions in health care is problematic because such processes are collectively defined as complex adaptive systems (CASs). A CAS is characterized by groups of individuals who act in unpredictable, nonlinear (not cause and effect) ways, such that one person’s actions affect all the others (Holden, 2005). In CASs, humans do behave in unpredictable ways (Tan et al., 2005). Critical thinking can help all health care personnel to examine these complex systems, wherein groups solve problems through complex, continually altering interactions between the environment and all involved in the decision making (Fioratou et al., 2011). Situations within the environment constantly change and decision makers need to reframe their thinking as they broaden their awareness of the context of their decisions (Sharma & Ivancevic, 2010). Having situation awareness is a must (Fioratou et al., 2011; Sitterding et al., 2012). Decision making is also influenced by the manager’s leadership style. A democratic/collaborative style of leadership and decision making works best in a complex adaptive system, such as a hospital, which is characterized by a large array of social relationships that can have an economic impact on an organization. Staff nurses who are not engaged in shared decision making may experience less job satisfaction and subsequently may leave an organization, leading to loss of expertise in patient care (Gromley, 2011). However, the full array of leadership styles may at some time be used in the decision-making process. Vroom and Yetton (1973) proposed a classic managerial decision-making model that identified five managerial decision styles on a continuum from minimal subordinate involvement to delegation. Their model uses a contingency approach, which assumes that situational variables and personal attributes of the leader influence leader behavior and thus can affect organizational effectiveness. To diagnose the situation, the decision maker examines the following seven problem attributes: 1. The importance of the quality of the decision 2. Whether there is sufficient information/expertise 3. The amount of structure to the problem 4. The extent to which acceptance/commitment of followers is critical to implementation 5. The probability that an autocratic decision will be accepted 6. The motivation of followers to achieve organizational goals 7. The extent to which conflict over preferred solutions is likely
Critical Thinking and Decision-Making Skills
![]() http://evolve.elsevier.com/Huber/leadership/
http://evolve.elsevier.com/Huber/leadership/
DEFINITIONS
BACKGROUND
Critical Thinking
Critical Thinking in Nursing
Decision Making
DECISION OUTCOMES
DECISION-MAKING SITUATIONS
ADMINISTRATIVE AND ORGANIZATIONAL DECISION MAKING
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Nurse Key
Fastest Nurse Insight Engine
Get Clinical Tree app for offline access