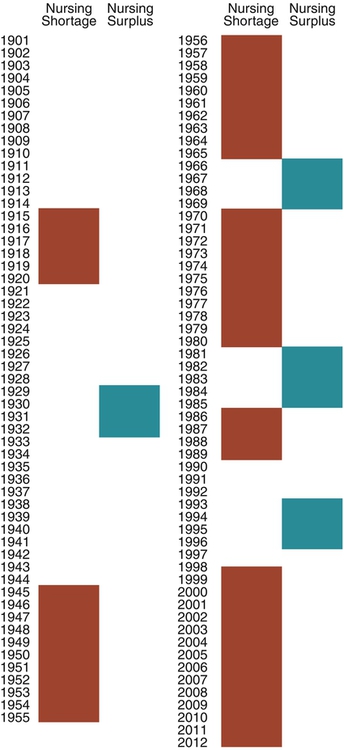
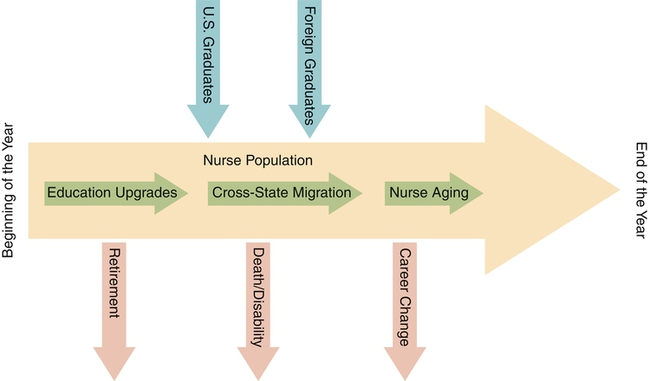
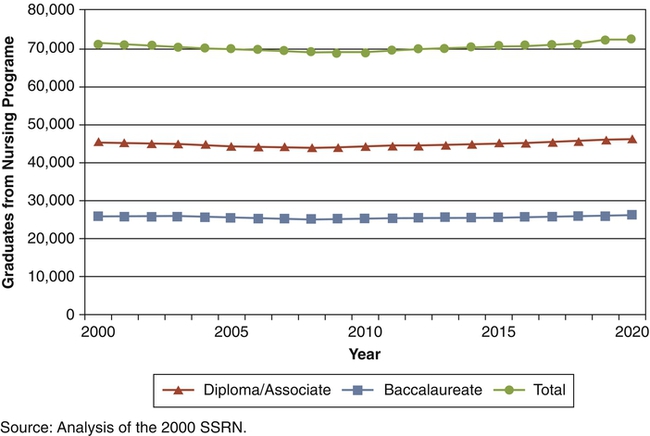
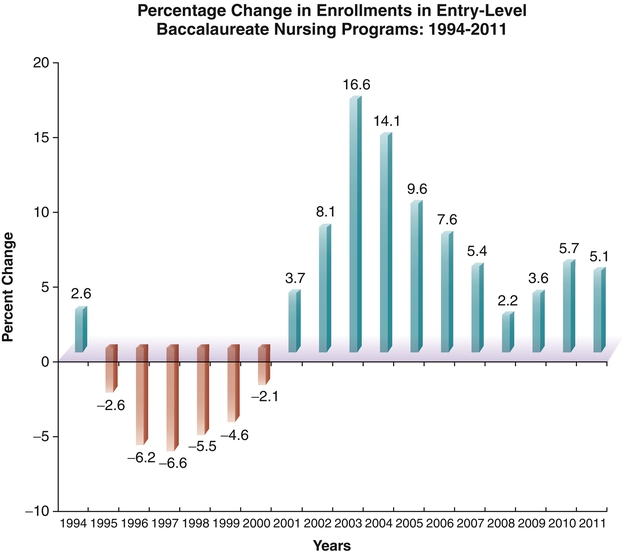
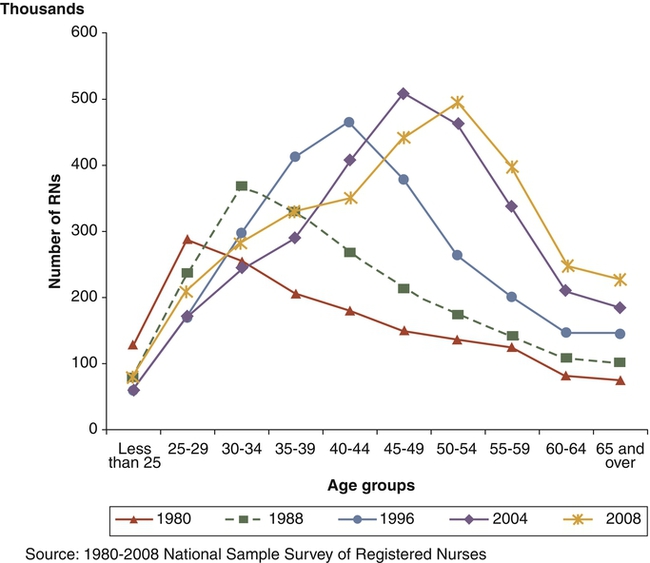
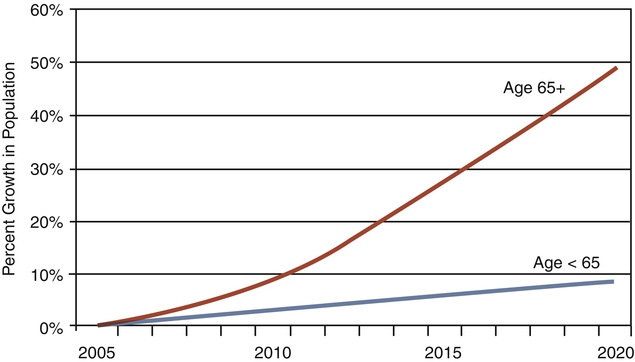
Issues surrounding the nursing shortage have highlighted the important leadership and management interventions related to recruitment and retention of nursing personnel. Civility is authentic respect for others requiring time, presence, engagement, and intention to seek common ground. Incivility is low-intensity deviant behavior with ambiguous intent to harm the target, characteristically rude, discourteous, and displaying a lack of respect for others. Recruitment, defined as replenishment, is the process used by organizations to seek out or identify applicants for potential employment. The impact is to ensure that an adequate number and quality of workers are available for selection and employment. Retention is the ability to continue the employment of qualified individuals, that is, nurses and/or other health care providers/associates who might otherwise leave the organization. The impact of this action is to maintain stability and enhance quality of care while reducing cost to the organization. Selection is defined as the job of determining the most qualified candidate for a job. This process includes reviewing, sorting, ranking, and offering of candidates recruited for a job. Staff vacancy is defined as an employee position—full-time or part-time equivalent—that is budgeted but not filled. Transformational leadership refers to a leader who inspires and transforms followers by raising their sense of the value of the task and their sense of importance (Bass, 1998). Bass (1998) outlined four components of transformational leadership: (1) charisma or idealized influence, (2) inspirational motivation, (3) intellectual stimulation, and (4) individualized consideration. Turnover is defined as the loss of an employee because of transfer, termination, or resignation. The turnover rate is derived by dividing the total number of nurses who left a work unit in 1 year by the total number of nurses employed on that unit. Transfer is the movement of an employee whose performance is satisfactory from one area to another within the same institution or corporation. Termination is the discharge of an employee who is performing at a less-than-satisfactory level or is not a good match for the organization. Resignation/voluntary turnover is the failure to retain an employee who is performing at or above satisfactory level. Although all turnovers have an associated cost to the organization, the most costly are those dealing with termination and resignations. Historically, the nursing shortage has been cyclical, vacillating between a supply shortage and a demand glut as noted in the nursing timeline discussed later. However, never before has the problem reached the magnitude that is presented by the United States Registered Nurse Workforce Report Card and Shortage Forecast, published in the January 2012 issue of the American Journal of Medical Quality (Juraschek et al., 2012), predicted to last through 2030. Cycles of nursing shortages and surpluses have been the focus of study and discussion for many decades. Multiple factors contribute to these phenomena. Just as numerous factors contribute to the nursing shortage, multiple possible solutions are needed to resolve it. An analysis of these factors will highlight the nursing shortage as a current and future issue, then leadership and management implications will be discussed. • Aging of current nurses in the workforce and their preparation for retirement • Lower numbers of students entering nursing as a career and a shift in need for both BSN and MSN/DNP prepared nurses • Aging of nursing faculty and inability of schools of nursing to meet education demands • Aging of the American population and struggles to expand capacity to meet demand for care • Significant changes in health care delivery system as the nation moves into health care reform Figures 20-1 and 20-2 show nursing supply and demand models. The 3.1 million U.S. registered nurses make up the largest health care occupation in the United States, holding about 2.6 million jobs in 2008, with about 63% of jobs in hospitals and more than 1 in 5 (21%) working part-time (American Nurses Association [ANA], 2011; Bureau of Health Professions [BHPr], 2010; Bureau of Labor Statistics [BLS], 2007). Despite large numbers, the supply of RNs has not been in balance with demand, nor has it been stable over time. Since the early 1900s, the U.S. nursing shortage and surplus has gone through phases. Although the length of each phase varies, clearly the alternation between shortage and surplus has been more frequent since the mid-1960s. Shortage phases have lasted longer, with only brief periods of surplus. Figure 20-3 shows the cycles of nursing shortages and surpluses from 1901 to 2012. However, the game changed in 2007 with the onset of the second recession in the new millennium that lasted longer than all previous recessions since World War II and resulted in high unemployment (Buerhaus et al., 2009a). These cycles are interrelated with social and economic forces, shifts, and changes. For example, the nursing shortage from about 1915 to 1920 resulted from the inability to recruit qualified and suitable students, because students provided most of the service on hospital wards (King, 1989). A little more than a decade later, in the context of the Great Depression (1929-1932), a surplus prevailed (Carlson et al., 1992). The 20 years after World War II (1945-1965) saw yet another nursing shortage (Grando, 1998). 1964 – Nurse Training Act financial aid program increases nursing enrollment and lowered job vacancy rates for next 6 years 1970 – Job vacancy rate steadily climbs through 1980, sparking the next shortage (Carlson et al., 1992) 1981 – Recession converts the vacancy rate to a surplus 1985 – Implementation of diagnosis-related groups (DRGs) passes and more patients are housed in hospitals prompting the next decline 1986 –Through 1992, hospital RN vacancy rate at national level of 11% (Buerhaus et al., 2005) 1992 – Managed care, capped reimbursements, cost containment, and downsizing hit the hospital industry again, boosting a nursing surplus 1998 – Cycle again shows evidence of reversal into shortage and marks the beginning of the shortage lasting into 2008 2000 – Average age of registered nurses is 45.2 years, with only 9% younger than 30 years 2001 – Recession: hospital RN vacancy rate at a national average of 13%, ranging up to 20% 2001 – American Nurses Association/American Organization of Nurse Executives (ANA/AONE) held Nursing Professional Summit to analyze shortage and develop strategic plan for future • Institute of Medicine (IOM) releases Crossing the Quality Chasm: A New Health System for the 21st Century 2002 – The number of new licenses in nursing is projected to be 17% lower in 2020 than in 2002 (BHPr, 2002) 2002 – ANA releases report, Nursing’s Agenda for the Future: A Call to the Nation, addressing shortage through education and workforce policy 2003 – Nursing shortage predictions continue 2004 – Average age of registered nurses is 46.8 years, and now only 8% report, being under age 30; BHPr predicted that by the year 2015, all 50 contiguous states will experience a nursing shortage 2005 – The average age of nurse educators is 55 years (Davidhizar, 2005) 2006 – In April, the BHPr’s Health Resources and Services Administration (HRSA) released projections of shortfall of more than 1 million nurses by 2020 (BHPr, 2006) 2006 – International Council of Nurses (, 2007a) report indicated that an aging population is a worldwide issue through first quarter of the twenty-first century, projecting more than 1 billion people over age 60 years, with Japan, Italy, Greece. and Switzerland at highest risk with 31% older than 60 years 2007 – Great recession hits and lasts into 2012. According to the U.S. Government (BHPr, 2006; BLS, 2007) more than 1 million nurses will be needed by 2016. Projected shortage growth: 2007 – The American Association of Colleges of Nursing (AACN, 2007) 2007 Survey on Faculty Vacancies report showed a national nurse faculty vacancy rate of 8.8%, which equates to approximately 2.2 faculty vacancies per school. 2007 – 71.4% of U.S. nursing schools turning away 40,285 qualified applicants to baccalaureate and graduate nursing programs because of faculty shortages 2007 – Buerhaus and colleagues revise and reduce their prediction of shortage for 2020 from 1 million to 800,000 2008 – Recession results in unprecedented rise in hospital employment of nurses, with estimates at 243,000 FTEs and more than 100,000 RNs older than age 50 years (Staiger et al., 2012), with average age of 46 years 2009 – Since 2002, RN FTEs increase 62% for nurses ages 23 to 26 years to approximately 165,000 (Auerbach et al., 2011) 2010 – 12.7% of U.S. population currently age 65 years or older 2010 – Enactment of the Patient Protection and Affordable Care Act to transform health care delivery 2011 – Enrollments in entry-level baccalaureate programs in nursing increased by 5.1% (AACN, 2011) 2011 – Institute of Medicine (IOM) releases The Future of Nursing: Leading Change, Advancing Health, calling for increased numbers of advanced-degree educated nurses to promote patient safety and quality of care (IOM, 2011) 2012 – AACN 2011–2012 Survey reports that 75,587 qualified applicants from baccalaureate and graduate nursing are turned away because of insufficient number of faculty, clinical sites, classroom space, and clinical preceptors and budget constraints 2012 – Current nursing workforce average age now is 44.2 years (Auerbach et al., 2011) 2012 – Nursing workforce now projected to grow at roughly the same rate as the population through 2030 (Auerbach et al., 2011) 2012 – Bureau of Labor Statistics (BLS) identifies registered nursing as one of the leading occupations in terms of job growth through 2020 (AACN, 2012a, b) Factors that affect nursing supply include the following: • Nursing education: Those impacting the number of new nursing graduates • Demographics: Those affecting the nature of the current RN workforce, thus the number of practitioners who can continue to work • Work environment: Those influencing the ability of the workplace to recruit and retain nurses The ability of the educational system to produce new graduates is affected by limited enrollment, a shift from associate degree to baccalaureate-prepared RNs, and a shortage of nursing school faculty, compounded by an insufficient number of clinical sites, classroom space, and clinical preceptors, as well as budget constraints (AACN, 2011–2012). Adding complexity, the average age of nurse faculty (60% age 50 + years; ANA, 2011) suggests a probable large surge of retirements in the near future. AACN’s report, 2010-2011 Salaries of Instructional and Administrative Nursing Faculty in Baccalaureate and Graduate Programs in Nursing, shows the following average ages of doctoral-prepared and master’s-prepared nurse faculty: • Professors: 60.5 years (PhD); 57.7 years (master’s) • Associate professors: 57.1 years (PhD); 56.4 (master’s) • Assistant professors: 51.5 years (PhD); 50.9 years (master’s) The overall numbers of nursing school enrollments is not growing fast enough to meet projected demand (Figure 20-4) for RN and APRN services into the next two decades. Even though the AACN reported a significantly higher percentage of increase (5.1%) in enrollments for entry-level baccalaureate nursing programs in 2011, the increase is not sufficient considering the implementation of the Affordable Care Act of 2010 and the impending increase of more than 32 million Americans accessing heath care services. Clearly there is strong interest among new nursing students and across the RN workforce in advancing education. The question now becomes what is the ability of higher learning institutions to handle the high number of applicants? In the 2010-2011 academic year, the data indicated that only 39.5% of applications were accepted for entry, whereas 75,587 qualified applicants were turned away, primarily because of shortage of faculty and resource constraints. The average eligibility rate for applications submitted into entry-level baccalaureate programs was approximately 50% overall, creating a shortfall on eligible admissions of 10.5%. The top reasons given by nursing schools for not accepting all qualified applicants into entry-level baccalaureate programs include insufficient clinical teaching sites (65.2%), a lack of faculty (62.5%), limited classroom space (46.1%), insufficient preceptors (29.4%), and budget cuts (24.8%). (The graphed data on turn-aways can be found at http://aacn.nche.edu/media-relations/TurnedAway.pdf.) The AACN survey also noted an increase in total enrollments into nursing programs, with an increase of 10% from 2010, across all baccalaureate, masters, and doctoral programs in 733 nursing schools (87.5%) in the United States. AACN reports that 80,767 students graduated from baccalaureate programs last year: “Given the call by the IOM for nurses to increase their education, AACN was pleased to see growth in degree-completion programs for RNs looking to earn their bachelor’s or master’s degree” (AACN, 2012a). For the ninth straight year, enrollment in RN-to-baccalaureate programs increased by 15.8% within a total of 814 advancement degree programs available nationwide. There are also 62 new advancement degree programs in development, marking a 7% increase in available programs. The Bureau of Health Professions (BHPr, 2004) projected that the number of licensed RNs would remain relatively constant (2.7 million) between 2000 and 2020. The number of licensed RNs was projected to increase slightly through 2012, but “today the youngest cohorts of nurses in the workforce are projected to be the largest in history by the time they reach middle-age and will provide 30 percent more FTE RNs than the baby-boomer cohorts who are now nearing retirement” (Auerbach et al., 2011). The current nursing shortage may last longer because of the large number of RNs approaching retirement age and the growth and aging of the U.S. population. For example, the report by the Bureau of Health Professions (BHPr) (2006) titled, The Registered Nurse Population: Findings from the March 2004 National Sample Survey of Registered Nurses, showed that the average age of registered nurses was 46.8 years in 2004 compared with 45.2 years in 2000. According to the BHPr’s (2010) report, The Registered Nurse Population: Initial Findings from the 2008 National Sample Survey of Registered Nurses, the percentage of nurses under age 40 years grew to 29.5% of RNs, increasing their numbers by nearly 18% from the same age group in 2004. This is a very positive finding, although as it was noted by Buerhaus and colleagues (2009a), the same survey sample revealed that most surveyed RNs were white females working in hospitals located in urban and suburban areas where the average nursing age only decreased by 2 years in 2008 compared to 2006. Only 19% of RNs were under age 35 years, and 4 in 10 RNs continued to fall between the ages of 35 to 49 years and 50 years and over (Figure 20-5). • The “graying” factor makes the nursing shortage an even greater issue, as the RN loss is projected to be 128% higher in 2020 than in 2002. The graying of the existing licensed pool is evident in the following data. According to the 2008 National Sample Survey of Registered Nurses released in September 2010 by the federal BHPr, the average age of the RN population in 2008 was 46 years of age, up from 45.2 years in 2000. • With the average age of RNs projected to be at 44.5 years in 2012, nurses in their 50s are expected to become the largest segment of the nursing workforce, accounting for almost one quarter of the RN population (Buerhaus et al., 2009c). • Within the next 8 years, the Bureau of Labor Statistics (BLS) projects the need for 1.2 million additional nurses to fill new positions and replace those retiring from the profession. Historically, when the unemployment rate was high, the RN workforce tended to be larger than predicted, and when unemployment was low, the RN supply decreased more than expected. An increase of 1 percentage point in the unemployment rate was associated with 1.2% increase in the size of the RN workforce (Staiger et al., 2012). RN employment overall has risen from 2 million in 2001 to 2.35 million in 2007 and 2.6 million in 2008, with 63% of this increase occurring in hospitals. There were an estimated 3,063,163 licensed registered nurses living in the United States in March of 2008; this is an estimated increase of 5.3% since 2004. However, nearly all of this employment increase was supplied by older RNs and non-U.S. born nurses, the two most rapidly increasing segments of the nursing workforce today (Buerhaus, 2008). Nurse vacancy and turnover rates are predictors of nursing shortages as well. The average nursing vacancy rate reported in 2008 was 8.1% (American Health Care Association, 2008) which represents a nearly 50% decrease from 16.1% in 2005. The turnover rate is slowly decreasing: 15.5% in 2003, and 13.9% in 2005 (AACN, 2008). However, the turnover rate for first-year nurses remains high; one survey reported 27.1% in 2007 (PricewaterhouseCoopers, 2007); another revealed 13% turnover and also found 37% of first-year nurses reporting that they felt ready to change jobs (Kovner et al., 2007). Several work environment factors have been cited as reasons for increased turnover (Buerhaus et al., 2000; Tri-Council for Nursing, 2004), including workload, autonomy, relations with managers, and compensation. Such factors influence job stress, in turn leading to job satisfaction or dissatisfaction (Hayhurst et al., 2005) and ultimately turnover and intent to stay. Professional autonomy, or control over the practice environment, was identified as the strongest predictor of nurses’ identification with the organization (Apker et al., 2003). Nurses who did not believe their jobs provided sufficient freedom were less likely to experience feelings of affiliation and loyalty toward their employers. The manager’s leadership style was found to be a significant predictor of nurses’ job satisfaction (Duffield et al., 2007; Weberg, 2010) and retention. Duffield and colleagues (2007) found that nursing leadership at the unit level is important for job satisfaction and intention to leave, which in turn has an impact on safety and patient outcomes. Weberg’s (2010) study showed significance between transformational leadership and increases in satisfaction and well-being with decreasing burnout and overall stress in staff nurses. An increase in salary for nurses relative to the salary in other occupations increases the attractiveness of nursing as a profession. An increase in salary now correlates more to the education level, expertise, and/or higher certification of the nurse as an individual. The impact of the recessionary decade increased the supply of nurses through several mechanisms. Part-time RNs were motivated to work more hours or full-time; older RNs delayed retirement or returned to work from retirement. Licensed RNs working in non-nursing jobs returned to nursing, and young people decided to enroll in nursing programs, a demand occupation with future stability (Staiger et al., 2012). The reliance on older RNs and on internationally educated RNs has increased significantly in the past 12 years. Older RNs comprised 44.7% of the total RN population in 2008, compared with 41.1% in 2004 and 33.4% in 2000. The percentage of RNs who were 60 years and older increased from 13.6% in 2004 to 15.5% in 2008, and the average age of the RN population in 2008 was 46 years of age compared to 46.8 in 2004 (BHPr, 2010). Between the years of 2001 and 2008, employment of older nurses in hospital settings fluctuated with the economy from boom to bust and accounted for 59% of the total increase in RN employment. During this same period, the nonhospital employment settings accounted for 18% of RN employment growth as well, but all growth in this period was represented by the older RN group over age 50 years (Buerhaus et al., 2009a). During this same period, the growth of middle-aged nurses (ages 35 to 49 years) was negative, with a substantial loss in nonhospital settings, thus overwhelming the hospital employment segment. Organizations reported that the shortage had a serious impact on nurse staffing, including increased overtime usage, higher stress, restricted expansion, changes in recruiting and hiring practices, decreased quality of care, and increased difficulty in scheduling coordination (May et al., 2006). This shortage is further being fueled by the international demand for nurses. According to Daniel and colleagues (2000), international recruitment of nurses once again surfaced as a way of addressing the nursing shortage, specifically in the United States, United Kingdom, Canada, and Western Europe. The International Council of Nurses (ICN) (2007a) reported worldwide population aging projections in the first quarter of the twenty-first century. The results clearly indicated that an aging population is an issue around the world, with greater than 1 billion people older than 60 years. The distribution of this population includes approximately 700 million in developing countries (which will increase nearly 240% from the 1980 levels). Included in this latter group are five of the ten largest populations in the world—China, India, Indonesia, Brazil, and Pakistan. This projection also indicated that the four countries with the oldest populations (with 31% older than 60 years) in the world—Japan, Italy, Greece, and Switzerland—also would be severely affected. Given the global magnitude of this shortage, few countries have nurses in excess; as a result, recruiting nurses internationally often creates an even more severe shortage in their home country. According to McHugh and colleagues (2008), the U.S. recruits more internationally educated nurses (IEN) than any other country. This is evident in that the number of IENs working in the United States has tripled since the 1990s. In March of 2008, an estimated 170,235 RNs living in the United States received their initial nursing education in another country or U.S. Territory, claiming 5.6% of the total nursing population. Approximately half of the IENs were originally from the Philippines (48.7%), 11.5% from Canada, and 9.3% were from India (BHPr, 2010). In 2008 alone, a record number of 48,000 RN FTEs were filled by foreign-born nurses (Buerhaus et al., 2009a). According to McHugh and colleagues (2008), major barriers to recruitment of IENs have been related to both limited visas and ethical concerns related to depletion of nursing resources in other countries. International recruitment has been of major concern to the International Council of Nurses (ICN) for more than a decade now. In 1999, the ICN released a position statement, Nurse Retention, Transfer and Migration, now updated as Nurse Retention and Migration (ICN, 2007a). In this document, the ICN linked the nursing shortage (inadequate supply of nurses) to lack of quality in health care. The statement addressed the individual nurse’s rights, as well as positive and negative issues related to migration. It also delineated roles that national nurses associations should take to raise nurse awareness of potential constraints and ensure that countries seeking to recruit nurses had policies and practices relative to fair and humane treatment of nurses. The ICN supports the migration of nurses as a short-term strategy for addressing the nursing shortage, viewing nurse migration as a way of increasing the nurse’s career opportunities and personal self-interests. Nurse migration is further viewed by the ICN as a way of increasing multicultural practice and learning opportunities within the nursing profession. This is especially true as nurses have identified two major reasons for leaving their home country—economic security and professional opportunity—although personal safety/security in the workplace and/or country has also been noted. However, concerns related to recruitment practices led the ICN in 2001 to issue a position statement on ethical nurse recruitment, now updated (ICN, 2007b). In 2004, the ICN and its sister organization, the Florence Nightingale International Foundation, investigated global nursing shortage issues related to international recruitment. This global analysis aimed to identify the policy and practice issues and solutions to be considered by governments, international agencies, employers, and professional associations when addressing the supply and use of nurses. To date, this initiative has produced an overview paper and white papers addressing such issues as migration, recruitment and retention, policy and planning, the work environment, and problems specific to Latin America and sub-Saharan Africa. Those papers are available on ICN’s website (www.icn.ch). Principles are relevant because they address changes that need to take place to ensure that nurses are treated fairly and equitably in the international marketplace. Unethical recruitment of nurses in the past has led to nurses being exploited and misled into accepting job responsibilities and work conditions incompatible with their qualifications, skills, and experiences. The ICN condemns the recruitment of nurses into countries where authorities support human rights violations. Sparacio (2005) addressed the complexity of international recruitment and the ethical impact of “brain drain” on the country from which nurses are being recruited. The California Nurses Association (CNA) and National Nurses Organizing Committee put forward a resolution, which was adopted by the CNA’s 2005 House of Delegates, outlining a code of practice for international nurse recruitment (Dumpel, 2005). This code was directed at the concerns and unlawfulness of international recruitment relative to the health care impact. The code specifically targeted human rights issues relative to accessibility and quality of care within the home country. Although international recruitment of nurses has greatly increased in the United States in recent years, few studies have been conducted to examine the adaptation, socialization, and true “lived experience” of the IEN or foreign-born nurse working in the United States. (Jose, 2011). Even though the core values of professional nursing are universally the same, the delivery of quality nursing care is dependent upon contextual factors such as shared common language and understanding among co-workers, patients, and families (Blythe & Baumann, 2009). Recent literature suggests that overall socialization into current American culture can add additional psychological stressors and possible retention issues in the long run for international recruits. Successful adjustment of IENs in the United States is important to ensure quality patient care and financial stability for recruiting health care agencies. Jose (2011) examined the socialization of foreign-born nurses working in the United States for less than 5 years and found six common themes among them: (1) dreams of a better life, (2) a difficult journey, (3) a shocking reality, (4) rising above the challenges, (5) feeling and doing better, and (6) readiness to help others. Considering that the “American way” is most often viewed through the media in other countries, it is often misperceived as a journey to immediate affluence without the struggles. For nurses coming into this country without any prior cultural or workplace socialization, culture shock is detrimental to them and to the recruiting organization. In light of this situation, more health care organizations are using intermediary recruitment agencies to provide preliminary workforce orientation and life skills planning. Kawi and Xu (2009) similarly found that the positive work ethic of IENs and their persistence and willingness to learn and adapt will ultimately prevail in their adjustment to their new U.S. workplace and add value to the nursing workforce. The recent increase in demand for RNs is projected to continue as a result of accelerating demand for health care services. This demand is affected by population growth, a rising proportion of people older than 65 years, with Americans 65 years and older representing nearly 20% of the population by 2030 (IOM, 2011), socioeconomic and cultural shifts, and advances in technology. Population growth and aging baby boomers are the major factors changing the demographic nature of the population, which in turn are affecting the demand for RNs. According to the Bureau of Health Professions (2004), the U.S. population will grow 18% between 2000 and 2020, which equates to an additional 50 million people requiring health care. Increased life expectancy resulting from advances in science and medicine accounts for most of this population growth, as well as the increase in the proportion of the population older than 65 years. A rapid increase in the elderly population began around 2010, when those at the top end of the baby boom generation reached age 65 years (Figure 20-6). The subgroup of people 65 years and older will grow 54% between 2000 and 2020, which equates to an additional 19 million people in this age group. This is equivalent to a tsunami wave that cannot be stopped yet has huge implications for health care delivery financing. In September 2001, the American Nurses Association (ANA)—in conjunction with the American Organization of Nurse Executives (AONE), Sigma Theta Tau International (STTI), 60 other professional nursing organizations, and 19 steering committee organizations—held a summit meeting to begin to analyze the nursing shortage problem and to develop a strategic plan entitled Nursing’s Agenda for the Future: A Call to the Nation (ANA, 2002). The outcome of this meeting was a vision statement and 10 domains for action. The vision statement was as follows (ANA, 2002): The ANA (2002), as part of the Nursing’s Agenda for the Future: A Call to the Nation, developed a “Desired Future Statement (Vision)” for each of the 10 domains. The statement for the domain of “Recruitment and Retention” clearly delineated the comprehensiveness of the undertaking, as follows (ANA, 2002): The vision was derived from the nursing research literature and incorporated the recurring themes related to recruitment and retention. Five strategies were formulated to achieve this vision. The strategies also addressed the two-pronged recruitment issue of the shortage (supply-side economics) and recruitment of (1) students for nursing education programs, and (2) qualified nurses for health care agencies. The strategies also targeted retention issues to be addressed within health care agencies and academic programs focusing on the development of career-based opportunities within health care, development and funding of creative educational initiatives, creation of a desirable and appealing image for nursing as a career choice, formulation and implementation of professional practice models, work environments that ensure career satisfaction, and development of comprehensive recruitment and retention strategies that will appeal to a diverse customer group/population (ANA, 2002). These global strategies were then broken down for the primary strategy in each of the domains, with work on the remaining strategies to be developed. The ANA also identified strategies that could be used to enhance student and faculty recruitment and/or retention (Table 20-1). TABLE 20-1 Student-Related and Faculty-Related Strategies for Recruitment and Retention
Confronting the Nursing Shortage
![]() http://evolve.elsevier.com/Huber/leadership/
http://evolve.elsevier.com/Huber/leadership/
DEFINITIONS
BACKGROUND
The RN Workforce
NURSING SHORTAGE TIME LINE OF EVENTS AND PREDICTIONS
FACTORS CONTRIBUTING TO THE NURSING SHORTAGE
Supply
Nursing Education
Demographic Factors
Aging of the RN Workforce
Work Environment Factors
Autonomy
Relations with Managers
Compensation
Changing Composition of the RN Workforce
International Recruitment
Demand
Changing Demographic Nature of the Population
AMERICAN NURSES ASSOCIATION’S CALL TO ACTION
Recruitment and Retention Strategies
Students
Faculty
Develop professional mentoring models
X
Create a specific curriculum to address diversity
X
X
Obtain funding to support minority enrollment
X
Develop and distribute promotional and recruitment materials to attract individuals from diverse backgrounds into nursing
X
Recruit retired nurses to form professional mentoring corps
X
Provide joint educational and service standardized internships and residencies
X
X
Co-op program/student clinical assistant (SCA) program
X
Negotiate professional paid development opportunities with employers
X
Create a website for leadership development that can be used by education, service, and professional organization members
X
X ![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Nurse Key
Fastest Nurse Insight Engine
Get Clinical Tree app for offline access