Comprehensive Pressure Ulcer Prevention Program Improves Outcomes for At-Risk Patients
Michael Kingan MSN, RN, CWOCN1
Kathleen Srsic-Stoehr MSN, MS, RN, NEA-BC2
Anne Marie Foley BSc, RN3
Stefanie Lescallet BSN, RN4
1Clinical Specialist Michael.J.Kingan@MedStar.net
2(Former) Senior Nursing Director, Evidence-Based Practice and Quality
3(Former) Clinical Manager/Interim Nursing Director, 2G MICU
4Nursing Director, 2F Stroke Center Unit
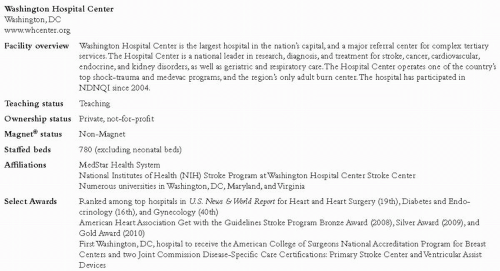
Washington Hospital Center Washington, DC
www.whcenter.org
Case Study Highlights
To reduce pressure ulcers, the Department of Nursing (DON) formed a Pressure Ulcer Performance Improvement (PI) Team, added a certified wound, ostomy, and continence nurse (CWOCN) clinical specialist, and started a Wound Resource Nurse program to increase expertise at the point of care. Individual units improved their staffing profiles, incorporated new evidence-based practices and products, and worked to create a culture that prized hospital-acquired pressure ulcer (HAPU) prevention.
Identification of the Problem
Washington Hospital Center joined NDNQI® in 2004 to benchmark pressure ulcers and other nursing indicators as part of the DON quality and performance improvement plan. (See Figure 1.) In 2005, HAPU rates were above the NDNQI mean. No formalized evidencebased prevention program was in place and compliance with skin care assessment and interventions was inconsistent. This case study chronicles the DON prevention initiatives and spotlights the efforts of one critical care and one acute care medical unit in reducing HAPUs.
Development of the Department of Nursing Initiatives
In early 2006, the new DON Strategic Plan formally addressed pressure ulcer reduction targets and action plans for the first time. The Strategic Plan set three primary objectives for quality and performance improvement:
Establish a leadership structure accountable for a culture of safety;
Adopt evidence-based practices to improve outcomes; and
Achieve national recognition for excellent clinical care.
The Strategic Plan also required establishing an annual target as a part of continued reduction of the HAPU rates. These targets to date are:
FY07 = NDNQI mean or better
FY08 = NDNQI mean or better
FY09 = NDNQI 50th percentile or better
FY10 = NDNQI 25th percentile or better
The DON formed the Pressure Ulcer Performance Improvement Team co-chaired by a clinical specialist and a unit director. Membership evolved to include bedside staff nurses, a physician “champion”, and representatives from the hospital’s Quality Resources, Risk Management, Clinical Nutrition, Physical Medicine and Rehabilitation, Clinical Resource Management, Outcomes Management, and Health Information Management departments. In 2006-2007, the PI team reviewed the literature for evidence-based prevention practices and developed targeted education programs. In addition, MedStar Health System, the parent company of Washington Hospital Center, started a systemwide task force in 2006 to provide an evidence-based practice pressure ulcer prevention and management program. Gap analysis was conducted at each hospital by interprofessional teams. The Hospital Center took the lead for MedStar in developing online prevention education modules for registered nurses (RNs), patient care technicians (PCTs), and all care providers, who completed training in late 2007.
In January 2008, a clinical specialist attended a university-based wound, ostomy, and continence nurse (WOCN) program, became certified, and began leading the WOCN service line. The WOCN consult process was incorporated into the electronic order entry system and new consult criteria were defined. The CWOCN worked with an interprofessional team (including a physical medicine and rehabilitation specialist, a plastic surgeon, a dietician, a resource manager, and a health information management director) to revise the formulary with evidence-based wound prevention and treatment options, improve the “present on admission” identification of pressure ulcers, and conduct weekly bedside rounds.
In March 2009, to further increase expert resources, the DON implemented a unit-based wound resource nurses (WRNs) program. Based on unit size and HAPU rates, at least one bedside RN and PCT from each unit joined the WRN program for a two-year commitment. After completing specialty education, each unit’s WRN team serves as a first-line, unit-based resource to their peers. WRN teams become experts in skin assessment and pressure ulcer prevention measures, including support surface and product usage and incontinence management. WRN PCTs assist in prevalence surveys and educate other PCTs about reporting mobility, nutritional intake, skin health, and incontinence problems to the patient’s RN. WRN RNs assist in developing prevention plans of care, critique new products, help with implementing new policies, and evaluate unit pressure ulcer quality data.
Financial Implications of Department of Nursing Initiatives
Pressure ulcers and other adverse patient outcomes have been identified as a preventable expense for hospitals. The incremental cost of care for a patient who develops a pressure ulcer averages $15,418 and ranges from $3,529 to $59,931 (Virkstis, Matsui, Westheim, Jaggi, & Boston-Fleischhauer, 2009). Training for the clinical specialist who became a CWOCN cost $8,000. The WRN program included a one-time initial cost of $3,760. Salary costs for unit-based staff participation in the WRN training were approximately $590 per nursing unit. Additional costs included targeted education programs, application of appropriate evidence-based prevention and treatment measures, and salary expenses
for WRN teamS’ ongoing work on their units. However, such expenses have enabled a substantial reduction of HAPU rates at the hospital, as exemplified by the critical care unit and acute care unit highlighted in this case study.
for WRN teamS’ ongoing work on their units. However, such expenses have enabled a substantial reduction of HAPU rates at the hospital, as exemplified by the critical care unit and acute care unit highlighted in this case study.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree