CHAPTER 19 Communicable and Infectious Disease Emergencies
I. GENERAL STRATEGY
A. Assessment
1. Primary and secondary assessment/resuscitation (see Chapter 1)
B. Analysis: Differential Nursing Diagnoses/Collaborative Problems
C. Planning and Implementation/Interventions
F. Age-Related Considerations
II. SPECIFIC COMMUNICABLE AND INFECTIOUS DISEASE EMERGENCIES
A. Human Immunodeficiency Virus/Acquired Immunodeficiency Syndrome
2. Analysis: differential nursing diagnoses/collaborative problems
3. Planning and implementation/interventions
4. Evaluation and ongoing monitoring (see Appendix B)
B. Diphtheria
2. Analysis: differential nursing diagnosis/collaborative problems
3. Planning and implementation/interventions
4. Evaluation and ongoing monitoring (see Appendix B)
C. Encephalitis
Encephalitis is a viral infection of the brain that causes an inflammatory response of brain tissue. It often coexists with meningitis and has a broad range of signs and symptoms, ranging from unrecognized mild cases to profound neurologic involvement. Most cases in North America are caused by arboviruses, herpes simplex virus (HSV) type 1, varicella-zoster virus (VZV), Epstein-Barr virus (EBV), and rabies. Transmission may be by animal bites (rabies) or may occur seasonally from vectors (e.g., mosquitoes, ticks, and midges carry arboviruses, Lyme disease, Rocky Mountain spotted fever, and so on). The more common human viruses are airborne and are transmitted via droplet or lesion exudate to the person, in whom replication takes place. The virus then enters the nervous system through the blood. In the brain, the virus enters the neuron, where it causes inflammation, neurologic dysfunction, and damage. Encephalitis occurs in all age groups, and mortality ranges from 5% to 10% from arbovirus infection to nearly 100% for rabies.
2. Analysis: differential nursing diagnoses/collaborative problems
3. Planning and implementation/interventions
4. Evaluation and ongoing monitoring (see Appendix B)
D. Hepatitis
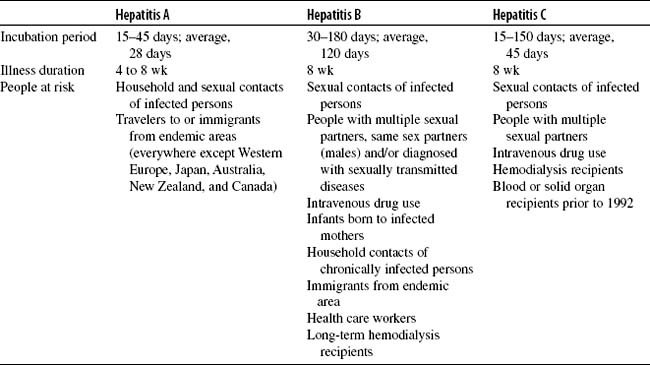
Hepatitis is a viral syndrome involving the hepatic triad (bile duct, hepatic venule, and arteriole) and the central vein area. Cellular inflammation leads to disruption of the hepatic architecture. Types of hepatitis viruses are identified by letters and vary in incubation and duration periods. Hepatitis A virus (Table 19-1) is transmitted primarily through the fecal-oral route. It is found in serum and stool and is infectious 2 weeks before and 1 to 2 weeks after the appearance of jaundice. Hepatitis B virus (HBV) (see Table 19-1) is transmitted most commonly by IV drug use, sexual contact, and less frequently through blood transfusions since testing of the blood supply began. Hepatitis B surface antigen (HBsAg) appears early in the disease process. Hepatitis B e antigen (HBeAg), thought to be a degradation product of the hepatitis B core antigen (HBcAg), also appears about the same time. Antibodies are produced for each antigen. Persistence of core antibodies indicates chronic infection. Persistence of surface antibodies indicates immunity to reinfection. HBsAg in the serum without symptoms is indicative of a carrier state. Hepatitis C virus (see Table 19-1) is transmitted mostly through IV drug use and blood transfusions and is identified by the presence of antihepatitis C virus antibodies. As many as 50% of hepatitis C infections become chronic, and there is no immunity. Hepatitis C causes approximately 60% of hepatitis cases transmitted by blood transfusion. Hepatitis D is found only in patients with acute or chronic HBV infection and is transmitted most commonly by IV drug use and sexual contact. Hepatitis E is an endemic, enterically transmitted infection caused by eating or drinking contaminated food or water and is similar to hepatitis A. Patients with all forms of hepatitis present with the same clinical features; laboratory testing determines the specific origin. Hepatitis A usually resolves in 4 to 8 weeks and hepatitis E in 6 to 9 months. The remaining types can all continue in a chronic state, which may result in cirrhosis and liver cancer. At this time, there is no cure; however, treatments using interferons and ribavirin are showing success in management of the diseases.