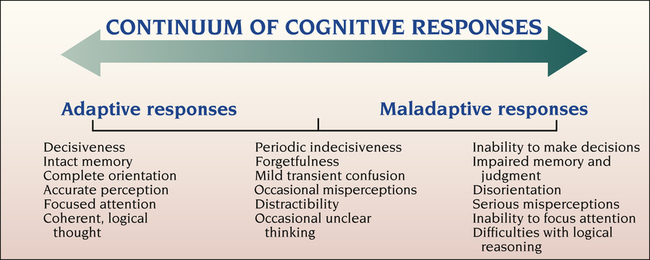
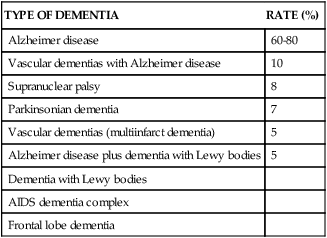
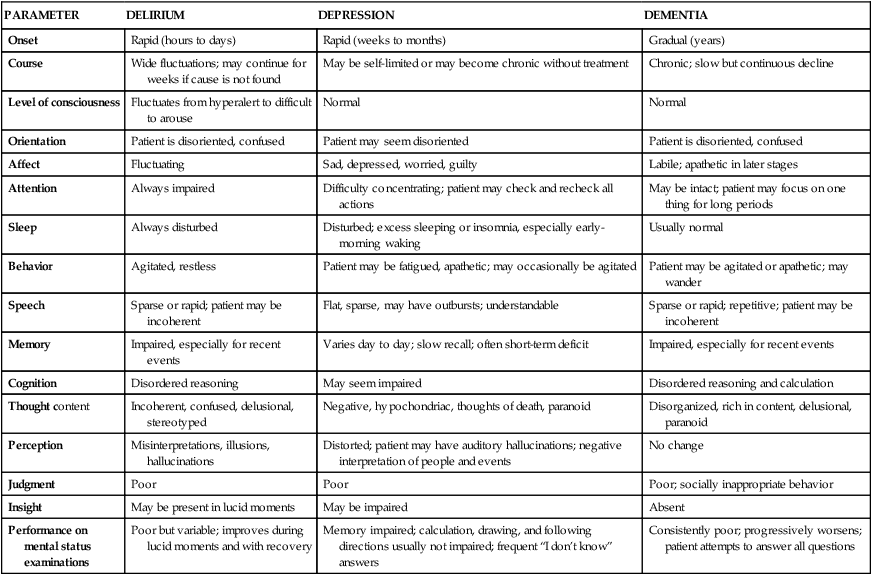
1. Describe the continuum of adaptive and maladaptive cognitive responses. 2. Identify behaviors associated with cognitive responses. 3. Analyze predisposing factors, precipitating stressors, and the appraisal of stressors related to cognitive responses. 4. Describe coping resources and coping mechanisms related to cognitive responses. 5. Formulate nursing diagnoses related to cognitive responses. 6. Examine the relationship between nursing diagnoses and medical diagnoses related to cognitive responses. 7. Identify expected outcomes and short-term nursing goals related to cognitive responses. 8. Develop a family education plan to help caregivers cope with maladaptive cognitive responses. 9. Analyze nursing interventions related to cognitive responses. cognitive responses in the adult. Although maladaptive cognitive responses may occur at any age, they are most common in the elderly. Maladaptive cognitive responses include an inability to make decisions, impaired memory and judgment, disorientation, misperceptions, decreased attention span, and difficulties with logical reasoning. They may be episodic or continuous. Depending on the stressor, the condition may be reversible or it may be a progressive deterioration in functioning. Figure 22-1 presents the continuum of cognitive responses. Maladaptive cognitive responses are seen in people who have the psychiatric diagnoses of delirium, dementia, and amnestic and other cognitive disorders. This chapter focuses primarily on delirium and dementia, because these are the psychiatric categories related to cognitive impairment that nurses encounter most often. Assessment relies heavily on biological findings (see Chapter 5) and on the results of the mental status examination (see Chapter 6). Standardized assessment tools also may be useful. Delirium results in disturbances in the following areas: • Consciousness—reduced clarity or awareness of the environment • Attention—impaired ability to direct and maintain mental focus, resulting in problems with processing stimuli into information • Cognition—recent memory impairment, disorientation to time and person, or language disturbance • Perception—misinterpretations, illusions, or hallucinations The clinical example that follows illustrates the behavior typical of a patient who is delirious. Delirium is commonly found in hospitalized patients, particularly in intensive care units (ICUs), geriatric psychiatry units, emergency departments, alcohol treatment units, and oncology units (Fricchione et al, 2008; Uguz et al, 2010). In addition, a diagnosis of delirium can be missed because the symptoms are assumed to be caused by depression. If adequate intervention does not take place, delirium may become chronic and irreversible. In some cases the process of dementia can be reversed, and the person’s intellectual functioning improves if the underlying stressors are identified and treated. However, in many cases dementia involves a continual and irreversible decline in mental function and behavior. Reversible causes of dementia are listed in Box 22-1. Dementia may occur at any age but most often affects the elderly. This condition results from structural and neurochemical changes in the brain resulting from trauma, infection, cerebrovascular disruptions, substance use, or an unknown cause. The various types of dementia are listed in Table 22-1. TABLE 22-1 TYPES AND OCCURRENCE RATES OF DEMENTIA In the United States, early-onset dementia affects more than one-half million people younger than 65 years of age. In younger adults, early symptoms may be mistaken as stress or depression (Hunt, 2011). Dementia forces individuals to assume dependent roles within their families at a time when they may be primary caretakers themselves. Facts and figures about AD are presented in Box 22-2. The following clinical example demonstrates the behaviors associated with dementia. The behaviors associated with dementia reflect the brain tissue alterations that are taking place (Table 22-2). Behavioral change occurs slowly in the early and late stages of AD and rapidly in the middle stage. The three stages of AD are listed in Box 22-3. TABLE 22-2 ASSOCIATION OF AREAS OF BRAIN PATHOLOGY WITH BEHAVIORAL CHANGES IN DEMENTIA Depression associated with AD is among the most common mood disorders of older adults. Aggression in patients with dementia is strongly linked to the presence of depressive symptoms. Appropriate treatment of the depression may be a way of preventing and managing the physically aggressive behavior. AD behaviors related to delirium, dementia, and depression are compared in Table 22-3. TABLE 22-3 COMPARISON OF DELIRIUM, DEPRESSION, AND DEMENTIA Memory includes several aspects: • Remote memory: recall of events, information, and people from the distant past • Recent memory: recall of events, information, and people from the past week or so • Immediate memory: recall of information or data to which a person was just exposed All of these are evaluated during a mental status examination (see Chapter 6). As AD progresses, patients often develop aphasia, apraxia, agnosia, and amnesia: • Aphasia is difficulty finding the right word. • Apraxia is the inability to perform familiar skilled activities. • Agnosia is difficulty in recognizing well-known objects, including people. • Amnesia is significant memory loss in the absence of clouded consciousness or other cognitive symptoms. The following are precipitating factors related to catastrophic reactions: • A change in cognitive status that results in difficulty organizing and interpreting information, sensory or cognitive overload, or misinterpretation of sensory stimuli • Psychosocial factors that result in increased demands to remember, such as fatigue, changes in routines or caregivers, and disorienting stimuli • Environmental factors, including environmental changes, noise, and decreased light The term confusion is often used when referring to a person with cognitive impairment. Although widely accepted as nursing and medical jargon, this term has not been specifically defined. It is better to use specific terms when describing a patient’s behavior. Five types of disturbing behaviors characteristic of dementia are summarized in Table 22-4. TABLE 22-4 DISTURBING BEHAVIORS CHARACTERISTIC OF DEMENTIA Traumatic brain injury, often referred to as TBI, is a disruption of normal brain function that occurs when the skull is struck, suddenly thrust out of position, or penetrated. Most often it is an acute event similar to other injuries. But it differs in important ways from other injuries. Brain injury can affect all aspects of a person’s life, including personality (U.S. Dept. VA/DoD 2009; SAMHSA, 2010; Reeves and Panguluri, 2011). For service members in Iraq or Afghanistan, the main TBI risk has been from an improvised explosive device (IED) such as a roadside bomb. Helmets and body armor provide some protection against penetrating head injury and, to a lesser extent, against head-impact events. However, the brain remains vulnerable to the effects of blast waves from IEDs. Gunshot wounds as well as combat- or training-related falls and motor vehicle crashes are other causes of service-related TBI (Snell and Halter, 2010). See Chapter 39 for a discussion of the mental health needs of the military and their families. TBI is classified into three categories: mild, moderate and severe. • Mild—A brain injury can be classified as mild if loss of consciousness and/or confusion and disorientation lasts less than 30 minutes. About 75% of all TBIs are mild. Concussion is often used interchangeably with mild TBI. Whereas magnetic resonance imaging (MRI) and computed tomography (CT) scans are often normal, the individual has cognitive problems such as headache, difficulty thinking, memory problems, attention deficits, mood swings, and frustration. These injuries are often overlooked and can be difficult to diagnose. • Moderate—Moderate brain injury is related to loss of consciousness for more than 30 minutes and less than 24 hours. There may be amnesia for 1 to 7 days related to the injury. Brain imaging may or may not reveal abnormalities. • Severe—Severe brain injury is associated with loss of consciousness for longer than 24 hours. There is often objective evidence of brain injury on brain scans and neurological examinations. The deficits range from impairment of higher-level cognitive functions to comatose states. Survivors may have limited function of arms or legs, abnormal speech or language, loss of thinking ability, and emotional problems. The common effects of TBI are listed in Box 22-4. The level and duration of the effects vary from person to person. These effects can be confused with symptoms of other psychiatric disorders. After TBI, a person is at risk for a range of psychiatric disorders, including depression, generalized anxiety disorder, panic disorder, agoraphobia, and posttraumatic stress disorder (Bryant et al, 2010). About half of all people with TBI also experience chronic pain. These comorbid psychiatric illnesses predict poorer health outcomes and poorer quality of life (Bombardier et al, 2010; Reeves and Panguluri, 2011). In 2030, almost one in five U.S. residents, including all of the so-called baby boomers, will be 65 years of age and older. This age group is projected to increase to 88.5 million in 2050, more than doubling the number in 2008. Similarly, the 85 and older population is expected to more than triple, from 5.4 million to 19 million between 2008 and 2050 (U.S. Census Bureau, 2008). AD is the most prevalent cause of maladaptive cognitive responses. Intensive research has focused on identifying its causes, characteristics, and treatment (Holcomb, 2008). Investigators have found that characteristic alterations occur in brain tissue of people with AD: • Neuritic plaques, which consist of amyloid-β (a starchlike protein) and remains of dying nerve cells. Plaques also contain altered glial cells. • Neurofibrillary tangles, which are twisted clumps of protein fibers. Tangles contain a substance called tau protein, which seems to interfere with internal transport in neurons.
Cognitive Responses and Organic Mental Disorders
Continuum of Cognitive Responses
Assessment
Behaviors
Behaviors Associated With Delirium
Behaviors Associated With Dementia
TYPE OF DEMENTIA
RATE (%)
Alzheimer disease
60-80
Vascular dementias with Alzheimer disease
10
Supranuclear palsy
8
Parkinsonian dementia
7
Vascular dementias (multiinfarct dementia)
5
Alzheimer disease plus dementia with Lewy bodies
5
Dementia with Lewy bodies
AIDS dementia complex
Frontal lobe dementia
ANATOMICAL STRUCTURE
FUNCTION
DYSFUNCTION
Occipital lobe
Visual processing
Blindness, loss of depth perception, color agnosia (lack of recognition), persistent after-images
Frontal lobe
Organization of words into fluent speech
Difficulty using “little words” (e.g., in, on, he, she, or); changes in personality, judgment, and behavior
Parietal lobe
Association area for integrating sensory input
Alexia (inability to read), agraphia (inability to write), neglect syndrome, inability to perceive pain, agnosia, apraxia, aphasia, visual-spatial disturbances, loss of executive functions, psychosis
Temporal lobe
Recognition and comprehension of sensory input; hearing; memory consolidation; association of memory, thought, perception, and emotion
Agnosia, apraxia, aphasia, visual-spatial disturbances, loss of executive functions, disorientation in space and time, psychosis, memory loss, misinterpretation of emotional events, misinterpretation of relationships
Limbic system
Emotions, storage of short-term memory, mood
Memory dysfunction, no affective dimension to memory, apathy, unstable affect, personality changes, poor learning ability, memory loss
PARAMETER
DELIRIUM
DEPRESSION
DEMENTIA
Onset
Rapid (hours to days)
Rapid (weeks to months)
Gradual (years)
Course
Wide fluctuations; may continue for weeks if cause is not found
May be self-limited or may become chronic without treatment
Chronic; slow but continuous decline
Level of consciousness
Fluctuates from hyperalert to difficult to arouse
Normal
Normal
Orientation
Patient is disoriented, confused
Patient may seem disoriented
Patient is disoriented, confused
Affect
Fluctuating
Sad, depressed, worried, guilty
Labile; apathetic in later stages
Attention
Always impaired
Difficulty concentrating; patient may check and recheck all actions
May be intact; patient may focus on one thing for long periods
Sleep
Always disturbed
Disturbed; excess sleeping or insomnia, especially early-morning waking
Usually normal
Behavior
Agitated, restless
Patient may be fatigued, apathetic; may occasionally be agitated
Patient may be agitated or apathetic; may wander
Speech
Sparse or rapid; patient may be incoherent
Flat, sparse, may have outbursts; understandable
Sparse or rapid; repetitive; patient may be incoherent
Memory
Impaired, especially for recent events
Varies day to day; slow recall; often short-term deficit
Impaired, especially for recent events
Cognition
Disordered reasoning
May seem impaired
Disordered reasoning and calculation
Thought content
Incoherent, confused, delusional, stereotyped
Negative, hypochondriac, thoughts of death, paranoid
Disorganized, rich in content, delusional, paranoid
Perception
Misinterpretations, illusions, hallucinations
Distorted; patient may have auditory hallucinations; negative interpretation of people and events
No change
Judgment
Poor
Poor
Poor; socially inappropriate behavior
Insight
May be present in lucid moments
May be impaired
Absent
Performance on mental status examinations
Poor but variable; improves during lucid moments and with recovery
Memory impaired; calculation, drawing, and following directions usually not impaired; frequent “I don’t know” answers
Consistently poor; progressively worsens; patient attempts to answer all questions
BEHAVIOR
DESCRIPTION
EXAMPLES
Aggressive psychomotor behavior
An increase in gross motor movement that has the effect of harming or repelling another
Hitting, kicking, pushing, scratching, assaultiveness
Nonaggressive psychomotor behavior
An increase in gross motor movement that does not have an apparent negative effect on others but draws attention because of its repetitive nature
Restlessness, pacing, wandering
Verbally aggressive behavior
Vocalizations that have the effect of repelling others
Demanding, disruptive, manipulative behaviors; screaming; complaining; negativism
Passive behavior
A diminution of behavior—that is, a decrease in gross motor movement accompanied by apathy and a lack of interaction with the environment
Decreased activity, loss of interest, apathy, withdrawal
Functionally impaired behavior
Loss of ability to perform self-care, the expression of which may be aversive and burdensome
Vegetative behaviors, incontinence, poor personal hygiene
Behaviors Associated with Traumatic Brain Injury
Predisposing Factors
Aging
Neurobiological
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Cognitive Responses and Organic Mental Disorders
Get Clinical Tree app for offline access
