Introduction
An introduction to the systems and processes of clinical governance and their application to maternity care are provided in this chapter. In particular, it focuses on the following key building blocks of clinical governance:
- evidence-based practice
- clinical audit
- professional development
- risk management.
Although these are presented as discrete entities, the clinical governance framework requires the integration of all these systems to achieve quality in clinical care and high standards of midwifery practice.
Included in this chapter are activities designed to help you understand and apply the building blocks of clinical governance. Clinical governance systems have evolved in maternity to enable the provision of high-quality maternity care. Quality maternity care is care focused on meeting the needs of women and their families, hence the chapter commences by exploring current concerns about standards for maternity care.
What is clinical governance?
Clinical governance is an umbrella term for systems and processes in NHS organisations that promote excellence in practice (Currie et al. 2004). The report by the Department of Health (DH), The New NHS: modern, dependable, states that the NHS ‘will have quality at its heart and that every part of the NHS should take responsibility for improving quality’ (DH 1997). Clinical governance was promoted as the framework for NHS organisations to focus on the quality of care provided (DH 1997).
Improving the patient’s experience is at the heart of the clinical governance framework, and successive directions for the modernisation of the NHS and maternity care have been driven by the need to improve the quality of services offered (DH 1997, 1998, 2000a, 2004a, 2007a, b, 2009, 2012). National bodies which support the implementation of clinical governance throughout the health service include the National Institute for Health and Clinical Excellence (NICE), Health Watch England (HWE), the Care Quality Commission (CQC), Monitor, as well as professional bodies such as the Nursing and Midwifery Council (NMC). Statutory supervision of midwives also provides a framework for promoting quality in midwifery practice (NMC 2012) (see Chapter 19) and there are many similarities between the framework for supervision and the framework for clinical governance.
The central focus of both is the promotion of quality in maternity care. In their review of maternity services at the North West London Hospital’s NHS Trust, the NMC concluded that ‘the safety of women would be enhanced by cohesive clinical governance systems along with clear lines of reporting that incorporate statutory supervision of midwives’ (NMC 2006).
Current standards for maternity services
Improving women’s experience and outcomes of maternity care is the guiding principle of clinical governance and NHS policy on maternity services (DH 2004a, 2007a, b, 2009, 2010, 2012). The National Service Framework (NSF) (DH 2004a), which has had a major impact on current standards for maternity care, specified that women should have access to supportive, high-quality maternity services, designed around their individual needs and those of their babies. These recommendations mirror the recommendations made in previous policy documents as well as current NHS policy. Nevertheless, the evidence indicates that quality of maternity care remains a cause for concern (Care Quality Commission 2012, Health Care Commission 2008, NMC 2012). Whilst overall satisfaction with maternity services is high, concern about the quality of maternity care in many NHS trusts demonstrates the need to ensure that robust mechanisms to promote clinical governance are embedded in practice (Care Quality Commission 2012, Health Care Commission 2008, National Perinatal Epidemiology Unit 2007).
Poor standards of clinical care have been cited by successive Confidential Enquiries into Maternal and Infant Deaths as a major contributing factor in the deaths reported. The most recent Centre for Maternal and Child Enquires (CMACE) (formely known as The Confidential Enquiry into Maternal and Child Health (CEMACH)) report, Saving Mothers’ Lives, identified that substandard clinical care was present for 70% of direct deaths and 55% of indirect deaths (CMACE 2011).
The CMACE study on women with type 1 and type 2 diabetes found that the majority were poorly prepared for pregnancy and had poor glycaemic control around the time of conception and in early pregnancy. This study also raised serious concerns about the care of these women during pregnancy and labour as well as the care of the baby (CEMACH 2005). The findings of these reports clearly demonstrate the need to strengthen the frameworks for clinical governance in maternity.
The Care Quality Commission (CQC) is responsible to the DH for assessing standards in health and social care, including standards in maternity care. The CQC (previously the Health Care Commission, HCC) has highlighted a number of concerns related to standards of maternity care in the UK (Care Quality Commission 2012, Health Care Commission 2005, 2006, Kennedy 2005). The HCC identified a number of common themes that undermined the safety of mothers and babies.(Kennedy 2005). These include:
- weak risk management structures
- poor working relationships
- inadequate training and supervision
- poor environment, with services isolated geographically or clinically
- shortages of staff
- poor management of temporary employees.
The following activity provides you with the opportunity to reflect on your perceptions of the standards of maternity care within your maternity unit and identify potential gaps in the quality of care. The recommendations in Table 20.1 are drawn from recommendations made in the NICE Quality Standards for antenatal care (2012), caesarean section (2011) and postnatal care (2006a).
- In relation to local evidence, identify if each of these standards is met.
- Take one recommendation where you consider the standard is not met, and provide a rationale as to why this standard needs to be met.
- List what you feel should be implemented to support the achievement of this recommendation.
Table 20.1 NICE recommendations
Source: compiled from recommendations from NICE 2006b, 2011, 2012.
| Recommendations | Met | Not met |
| 1. Pregnant women are supported to access antenatal care, ideally by 10 weeks 0 days | ||
| 2. Pregnant women are cared for by a named midwife throughout their pregnancy | ||
| 3. Pregnant women with an uncomplicated singleton breech presentation at 36 weeks or later (until labour begins) are offered external cephalic version | ||
| 4. Women should be offered one-to-one care by a midwife in established labour | ||
| 5. Elective caesarean section should be performed at 39 weeks | ||
| 6. A partogram with a 4 hours action line should be used to monitor progress of labour of women in spontaneous labour with an uncomplicated singleton pregnancy at term, because it reduces the likelihood of caesarean section | ||
| 7. All women should have an individualised care plan in the postnatal period |
Developing action plans to facilitate and monitor the implementation of national standards is an important part of the clinical governance agenda in maternity services. Achieving this involves a range of activities including evidence-based practice, risk management, clinical audit and continued professional development, which are key components of clinical governance. Successful implementation of these systems requires strong leadership and the commitment of the entire organisation.
To facilitate the achievement of quality in maternity care, many maternity units have a clinical governance subgroup. This subgroup is accountable to the trust’s clinical governance group for overseeing the promotion of quality in maternity care. Membership of the group includes midwifery and obstetric leads for clinical audit, risk management, evidence-based practice and professional development in addition to a supervisor of midwives. The frequency of meetings is determined by local requirements, but on average the group meets once a month.
- Who are the members of this group?
- Discuss with a member of the group the group’s overall purpose – this is often referred as the group’s terms of reference.
- How does the group relate to the overall clinical governance framework for the trust?
- Identify the key challenges currently facing this group.
- Ask to attend one of their meetings.
You may well discover that the function of the group is to bring together the different components of clinical governance, so that each part is working in harmony with the others to facilitate continuous quality improvement in maternity care. You may also discover that some of the key activities of this group relate to the following:
- evidence-based practice
- clinical audit
- professional development
- risk management.
The following sections will discuss each of these aspects of clinical governance in more depth. However, achieving quality in maternity care requires the integration of all of them.
Evidence-based practice
The development and implementation of evidence-based practice for the care of women throughout their maternity are key components of clinical governance. Evidence-based practice can be defined as ‘the conscientious, explicit and judicious use of current best evidence in making decisions about the care of individual patients, based on skills which allow [the practitioner] to evaluate both personal experience and external evidence in a systematic and objective manner’ (Sackett et al. 1997).
This definition incorporates knowledge and skills gained from personal experience as well as evidence derived from research (see Chapter 18). The value of individual practitioners’ knowledge and skill is also recognised by NICE, which states that although ‘clinical guidelines help health professionals in their work, they do not replace their knowledge and skills’ (NICE 2006b). Clinical guidelines have been developed to assist practitioners to provide care within an evidence-based framework (Field & Lohr 1990). Guidelines for clinical practice can be developed locally or at a national level by NICE.
The National Institute for Health and Clinical Excellence was established because of concern over disparities in clinical practice between regions and hospitals. Part of the remit of NICE is to develop national clinical guidelines ‘on the appropriate treatment and care of people with specific diseases and conditions within the NHS’ (NICE 2006b). The group with responsibility for the development of NICE guidelines is drawn from members of all relevant professions as well as user groups. Guidelines in draft form are available on the NICE website and key stakeholders are invited to submit comments and feedback. This is an important part of the production of the guidelines and it is imperative that midwives and other stakeholders are proactive in ensuring that their voice is heard. The Royal College of Midwives, the Consultant Midwives Group and the Independent Midwives Association, amongst others, are registered stakeholders, and individual midwives can have their views represented through these groups. The NICE website provides information on guidance in development, guidance developed and also guidance to be developed, which affect midwifery practice and the standard of maternity care.
The National Institute for Health and Clinical Excellence also produces implementation advice for all clinical guidelines published after October 2005. This offers suggestions on how to implement specific guidance locally, and key drivers to change, as well as potential barriers and strategies to overcome these. Where NICE guidance exists, local guidelines are required to reflect it.
- List the guidelines that the NICE has produced in relation to maternity care.
- List the guidelines that are in the process of development or review in relation to maternity care.
The aim of national guidelines and standards is to support equality in clinical standards for all women using maternity services as well as the provision of cost-effective care.
In addition to national guidelines and standards for maternity care, there must be clear local arrangements for the development and implementation of best practice guidelines. The process of developing and implementing guidelines differs among NHS trusts, although the principles underpinning the development and implementation of guidelines are similar.
The Clinical Negligence Scheme for Trusts (CNST) requires each maternity provider to have a systematic framework for the development and implementation of guidelines (NHS Litigation Authority 2012). The overall responsibility for this rests with the executive board of each trust, but each trust division has a structurally identified group whose members include midwives, obstetricians, anaesthetists, paediatricians and risk managers as well as user representatives. The responsibility of this group includes some or all of the following:
- Take the lead to promote the development and implementation of evidence-based practice across the maternity services.
- Ensure that clinical guidelines are appropriately ratified according to trust policies.
- Ensure that guidelines are reviewed in light of NICE recommendations, current evidence as well as recommendations of professional bodies such as the Royal College of Midwives and the Royal College of Obstetricians and Gynaecologists.
- Develop a strategy for the dissemination of the guidelines to all members of the multidisciplinary team.
- Ensure that information to be given to women is evidence based.
- Develop an audit strategy to measure compliance with current guidelines.
The group is also responsible for ensuring that guidelines are reviewed in a timely manner.
Individual practitioners have a duty to practise in accordance with the guidelines, taking into consideration the individual needs of women. The Midwives’ Rules and Standards specify that a midwife’s practice must be based on ‘locally agreed evidence-based standards’ (NMC 2012). Reasons for non-compliance must be clearly recorded in the woman’s records.
Guidelines alone are of limited value in promoting best practice. Therefore, there should be a clear strategy to facilitate their implementation. According to the evidence, multifaceted intervention as opposed to one-off intervention is more successful in embedding guidelines in practice (NICE 2002). Strategies used to support local implementation of evidence-based guidelines include:
- mandatory education programmes
- case study review
- reminders in clinical practice
- reminders in maternity records
- discussion at meetings/handovers
- newsletters
- information to women
- reflective practice forums
- feedback from audit.
As part of the implementation process, barriers to the implementation of evidence-based practice need to be identified, and strategies to overcome these barriers identified (NICE 2002).
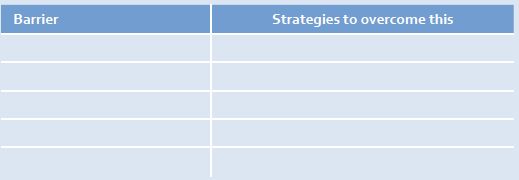
You may have identified that barriers to successful implementation of guidelines lack of knowledge, fear, lack of resources and lack of ownership, and that strong leadership in practice is critical to overcome these. You may also identify that providing clinicians with feedback on whether the guidelines have been fully implemented is important in promoting compliance. Clinical audit is an important part of the clinical governance framework which aims to achieve this.
Clinical audit
Clinical audit provides a framework for measuring quality in midwifery practice through the systematic analysis of standards and the subsequent implementation of any recommendations to improve the quality of care (NICE 2002). Clinical audit comprises a number of different components, including the identification of audit topics, measuring compliance against agreed standards, and identifying and implementing changes in practice as a result of the audit findings. Further audit is then performed to ensure the successful implementation of recommendations and to monitor effectiveness of the implementation strategy. This process is often referred to as the audit cycle (NICE 2002), the overall aim of which is to improve the quality of care.
Clinical audit is concerned not only with reviewing standards but also implementing the necessary changes to practice resulting from the audit findings (NICE 2002). This ensures that the audit process leads to improvements in practice in line with the aims of clinical governance.
How does audit differ from research?
Many midwives are confused about the differences between research and audit. Although midwifery audit and research have many similarities, the purpose is different. Research is concerned with finding out what we should be doing, whereas audit is concerned with what we are doing. For example, whilst a midwife researcher might want to find out best practice in the frequency of antenatal visits for women booked for midwifery-led care, the midwife auditor might want to find out if the frequency of visits accords with local guidelines and NICE recommendations.
The audit process facilities the achievement of quality in maternity care by providing feedback on current standards, and improves practice through the implementation of action plans. Therefore, each maternity service should have a multidisciplinary audit strategy that is reviewed annually and is communicated to all members of the multidisciplinary team. Audit leads should include representatives from midwifery practice, supervision of midwives and obstetrics. The role of the audit leads is to ensure that all members of the multidisciplinary team are involved in the development of the audit strategy as well as the audit process.
In order to co-ordinate and lead the audit process, most NHS trusts have audit departments and audit lead personnel who are part of the overall clinical governance team for the trust. Audit facilitators may also be available to provide support for midwives and other clinicians undertaking audit.



