CHAPTER 21
Chronic Venous Disease and Venous Ulcers
Section 1: Carolyn Robinson
Section 2: Monica Melo
OBJECTIVES
1. Define the pathophysiology of chronic venous disease.
2. Describe methods for classification of venous disease.
3. Describe diagnostic testing for venous disease.
4. Describe the most common invasive interventions for venous disease.
5. Identify the nursing implications relevant to chronic venous disease.
6. Describe the common findings associated with venous ulceration.
7. Identify common diagnostic testing associated with venous disease/ulceration.
8. Identify appropriate interventions for venous ulcers.
9. Describe methods of long-term self-care for venous disease/ulceration and prevention of recurrence.
Introduction
Chronic venous disease (CVD) includes a spectrum of clinical presentations ranging from uncomplicated telangiectasias and varicose veins to venous ulceration (Meisner, 2004). Venous disorders can be congenital or acquired. Chronic venous insufficiency (CVI) results from chronic venous hypertension related to dysfunction of the vein walls or valves (Hurie & Wakefield, 2012). Venous hypertension usually is the result of obstruction to venous flow, dysfunction of venous valves, and or failure of the venous pump (Alguire & Mathes, 2013).
Section 1: Chronic Venous Disease
A. Incidence
1. CVD affects approximately 2.5 million people in the United States. Approximately 20% develop leg ulcers.
2. Varicose veins affect up to 40% of adults and are more common in obese people, and in women who have had more than two pregnancies.
3. The prevalence of varicose veins vary widely from 2% to 56% in men and from 1% to 60% in women
B. Epidemiology
1. Older age
2. Family history
3. Female gender: pregnancy, especially multiparity
4. Standing occupation
5. Constipation/low-fiber diet
6. Obesity: BMI >30 kg/m2
7. Smoking
8. Oral contraceptives/HRT
9. Physical activity
10. Injury
11. History of phlebitis/clot (Dean & Spruiell, 2011)
C. Classification
1. Primary: degenerative process in normally formed vessel walls and valves without an identifiable mechanism of venous dysfunction
2. Secondary: result of a precursing event such as deep venous thrombosis (DVT). As the occluded venous segments recanalize after a DVT, chronic luminal changes occur along with partial obstruction and reflux leading to venous hypertension (Davies & Lumsden, 2011)
D. Venous Anatomy
1. The muscular fascia which surrounds the calf and leg muscles is separated into the superficial and deep compartments. The superficial compartment includes all tissues between the skin and muscular fascia. The deep compartment includes the muscles and deep veins which lie beneath the muscular fascia. The veins are divided into three systems: the superficial veins, the deep veins, and the perforating veins (Og˘ uzkurt, 2012).
2. Superficial venous system
a. Drains the skin and subcutaneous tissue
b. The superficial veins lie in the subcutaneous tissue
c. Great saphenous vein
1) Originates along the medial edge of the foot
2) Ascends along the medial leg joining the common femoral vein below the inguinal ligament
3) Communicates with the deep system through perforating veins
d. Small saphenous vein
1) Originates at the lateral edge of the foot
2) Ascends along the posterior calf joining the popliteal vein at or just below the knee (Kaufman, 2004)
3. Deep venous system
a. Contained in the deep muscle compartments
b. Intramuscular (within the muscle)
c. Intermuscular (between the muscle groups)
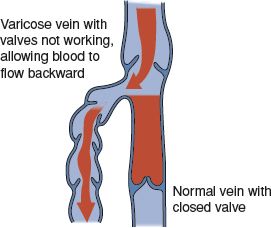
FIGURE 21.1 Normal vein valve closure and varicose vein.
d. Responsible for 90% of venous return through the action of the foot, calf, and thigh muscle pumps (Meisner, 2004)
e. Drain the lower extremity muscles (Meisner, 2005)
4. Perforating veins: connect the superficial with the deep veins and are found in the anterior, lateral, medial, and posterior thigh and calf (Moneta, 2013)
E. Vein Functions
1. Competent vein: blood flow returns normally to the heart
2. Incompetent vein: blood flows in the wrong direction
3. Reflux: blood flows backward in the vein
F. Chronic Vein Abnormalities (Moneta, 2013)
1. Telangiectasias (spider veins) are dilated intradermal venules less than 1 mm in diameter (Dean & Spruiell, 2011).
2. Reticular veins are dilated bluish subdermal veins 1 to 3 mm in diameter.
3. Varicose veins are dilated, elongated, tortuous, subcutaneous veins 3 mm or greater in size (see Fig. 21-1).
 I. Pathophysiology/Etiology
I. Pathophysiology/Etiology
A. Normal Venous Function
1. Calf muscle pump
a. Approximately 90% of the venous return in the legs occurs in the deep veins by the action of the foot, calf, and thigh muscle pumps (Meisner, 2005).
b. Propels blood toward the heart when the legs are moved or the calf muscle is tensed. Does not work when the person stands perfectly still (Hall, 2011).
c. The ejection fraction of the calf pump is approximately 65% as compared to the thigh pump which is 15% (Meisner, 2004) (see Fig. 21-2).
2. Gastrocnemius and soleal muscles
a. Systolic phase: calf muscle contraction closes valves of the perforator veins, propelling blood out of the deep veins toward the heart
b. Diastolic phase: calf muscle relaxes. Pressure in the deep veins and the sinuses decreases and the blood flows via perforators from the superficial system into the deep system (Dean & Spruiell, 2011)
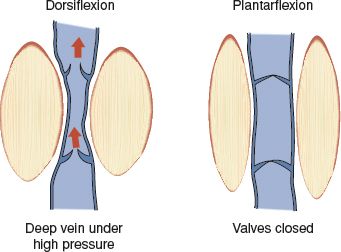
FIGURE 21.2 Calf pump muscle effect on venous valves.
3. Venous valves
a. Usually bicuspid. Direct blood flow from distal to proximal and from the superficial to the deep system
b. Arranged to only allow blood to flow toward the heart (Hall, 2011)
B. Abnormal Venous Function
1. Calf muscle pump (venous pump)
a. Systolic phase: Incompetent perforators allow direct flow of blood from the deep into the superficial veins. Ambulatory venous pressure is increased.
b. Diastolic phase: functions similar to a normal limb.
2. Reflux
a. Pathologic retrograde flow of blood
b. Occurs when the valves are absent or incompetent either by degenerative processes or an episode of DVT
c. Retrograde flow during calf muscle relaxation prevents the usual reduction in pressure (Meisner, 2004)
 II. Assessment
II. Assessment
A. Risk Factors (Hurie & Wakefield, 2012)
1. Congenital: factor VII excess, protein C deficiency, protein S deficiency, factor V Leiden, antithrombin deficiency, prothrombin
2. Acquired: HICV infection, age, immobilization, malignancy, heparin-induced thrombocytopenia, Behcet disease, nephrotic syndrome, antiphospholipid antibodies, myeloproliferative disorders, polycythemia vera, paroxysmal nocturnal hemoglobinuria, inflammatory bowel disease
3. Situational: surgery, trauma, pregnancy, oral contraceptives, hormone replacement therapy
4. Mixed: hyperhomocysteinemia, increased factor VIII levels, increased factor XI levels
B. Patient History
1. Subjective findings: leg aching, heaviness, burning, itching, fatigue, stinging, throbbing, venous claudication, edema, and in serious cases, ulcerations. Symptoms are aggravated by dependency and worse at the end of the day (Dean & Spruiell, 2011; Kachroo et al., 2012).

FIGURE 21.3 Hyperpigmentation changes associated with chronic venous disease.
2. Social: ETOH use, nicotine, and illicit drug use. Employment, daily activities, living situation, support systems.
3. Medications: prescribed and OTC
C. Physical Examination (Dean & Spruiell, 2011)
1. Inspection: Compare legs
a. Edema: initially seen at the ankle progressing to the calf as the disease progresses. May be pitting initially; however, as the disease progresses, the area becomes fibrotic with woody induration.
b. Hyperpigmentation: brownish coloration in the gaiter area (ankle to mid-calf) denoting extravasated intact or fragmented erythrocytes and hemosiderin (see Fig. 21-3).
c. Dermatitis: seen in the posteromedial gaiter area. Generally well demarcated, erythematous, dry and scaly.
d. Lipodermatosclerosis: localized chronic inflammation and fibrosis of the skin and subcutaneous tissue in the lower leg (Moneta, 2012).
e. Atrophie blanche or “white atrophy”: White, macular areas overlying the distal lower extremity as the CVI becomes more advanced.
2. Examination
a. Vital signs including height and weight
b. Pulse examination
c. Measure circumference of both legs just above the ankle, at the widest part of the calf, and the widest part of the thigh
D. Scoring Tools for Classification of Venous Disease
CEAP classification (Eklöf et al., 2004): developed to communicate the results of a comprehensive venous evaluation classifying venous disease by severity, cause, site, and specific abnormality. As the diagnosis and treatment modalities for venous disease changed, the original classification has been modified. Venous disease can be reclassified at any time and should be followed by date. Venous disease is often classified using only the C classification.
Basic CEAP classification
1. Clinical classification
C0: no visible or palpable signs of venous disease
C1: telangiectasias or reticular veins
C2: varicose veins
C3: edema
C4a: skin pigmentation or eczema
C4b: lipodermatosclerosis or atrophie blanche
C5: healed venous ulcer
C6: active venous ulcer
S: symptomatic, including ache, pain, tightness, skin irritation, heaviness and muscle cramps and other complaints attributable to venous dysfunction
A: asymptomatic
2. Etiologic classification
Ec: congenital
Ep: primary
Es: secondary (post-thrombotic)
En: no venous cause identified
3. Anatomic classification
As: superficial veins
Ap: perforator veins
Ad: deep veins
An: no venous location identified
4. Pathophysiological classification
Basic CEAP
Pr: reflux
Po: obstruction
Pr,o: reflux and obstruction
Pn: no venous pathophysiology identified
Advanced CEAP is the same as basic CEAP with the addition of locators for venous pathology
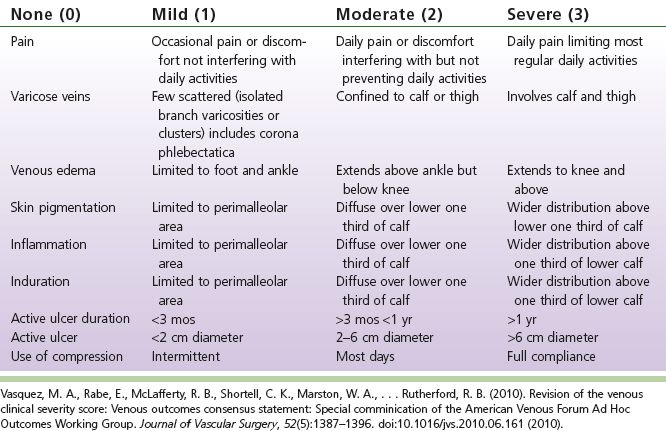
E. Venous Severity Scoring System (VCCS) (see Table 21-1) (Vasquez & Munschauer, 2011; Vasquez et al., 2010)
1. Developed to be more sensitive to changes in patient disease status over time.
2. Scores the venous disease based on categories: pain, varicose veins, venous enema, skin pigmentation, inflammation, induration, active ulcer, ulcer size, ulcer duration, and use of compression.
 III. Diagnostic Testing
III. Diagnostic Testing
A. Noninvasive Testing
1. Duplex ultrasonography
a. Test of choice for diagnosing venous insufficiency (Dean & Spruiell, 2011).
b. Obstruction: seen with loss-of-flow signal; chronic reveals smaller diameter of vein and is partially compressible; acute shows distension of vein and is not compressible. Characteristics of the intraluminal obstruction are different.
Table 21-1 Venous Severity Scoring System (VCCS)
c. Valvular insufficiency: seen when patient performs a Valsalva maneuver or compression of a vein above the probe, as reflux in a vein. Normal reflux is less than 1 second.
2. Magnetic resonance venography (MRV) and Computed Tomographic Venography (CTV)
a. Valuable technique for assessing veins in regions inaccessible or poorly accessible to sonography (Glockner & Lee, 2010).
b. Both allow for large fields of view with cross-sectional images that provide superb soft tissue detail and levels of contrast that permit clear delineation between veins and adjacent structures (Bismuth, Shah, & Karmonik, 2011).
3. Air plethysmography (APG) (Hurie & Wakefield, 2012)
a. Physiologic study used to assure venous reflux, calf muscle pump function, and venous obstruction
b. Measures calf volume change in response to gravity and exercise as a reflection of reflux (Meisner, 2004)
c. Can be useful in determining who will benefit most from surgical therapy
4. Photoplethysmography (PPG) (Meisner, 2004)
a. Simplest noninvasive test. Provides little quantitative information.
b. Based on transmission of infrared light into the skin and measurement of backscattered light by an adjacent photoreceptor.
 IV. Nonsurgical Management (the most common are discussed)
IV. Nonsurgical Management (the most common are discussed)
A. Supportive (Dean & Spruiell, 2011)
1. Leg elevation: when sitting, the legs should be higher than the hips and when lying, the legs should be higher than the heart.
TABLE 21-2 Compression Stocking Classification

2. Calf exercises with flexion and extension movements at the level of the ankle.
3. Meticulous skin care. Regular use of moisturizing lotions, creams. Exfoliating with a urea or alpha-hydroxy acid containing lotion for hyperkeratotic or ichthyotic skin.
4. Periodic use of topical glucocorticoid for eczematous stasis dermatitis.
B. Compression
1. To be effective, stockings must fit firmly with diminishing compression as the garment ascends the leg, avoiding a proximal constricting band.
2. Graduated external compression should provide a counterbalance to the graduated hydrostatic pressure change within the superficial veins.
3. Prescription stockings measured to fit properly are recommended.
4. Prescription garment can be designed to provide compression at the ankle ranging from 20 to 60 mm Hg. 20 to 30 mm Hg is usually sufficient for people with primary varicose veins.
5. Knee length is generally enough.
6. Stockings lose their elasticity with wear and washing. It is important to educate the patient in proper caring of the garment, to replace it every 6 months (see Table 21-2).
C. Pharmacology: The use of medications in the treatment of venous insufficiency has been studied in Europe but not in the United States.
1. Agents that may be useful (Dean & Spruiell, 2011)
a. Phlebotropic agents
1) Horse chestnut seed extract, hydroxyrutosides, micronized flavonoid fraction, maritime oxandrolone and danazol pine bark extract, calcium dobesilate, centella asiatica, aminaftone, and grape seed extract
b. Fibrinolytic agents
1) Stanozolol, oxandrolone, danazol, defibrotide, sulodexide, mesoglycan
c. Hemorheologic agents
1) Pentoxifylline
d. Antiplatelet agents
1) Aspirin
 V. Invasive Management: A complete ultrasound evaluation of the venous system is done prior to intervention to identify reflux.
V. Invasive Management: A complete ultrasound evaluation of the venous system is done prior to intervention to identify reflux.
A. Sclerotherapy (Dean & Spruiell, 2011)
1. Indications
a. Telangiectasias: cosmetic
b. Small superficial varices that do not drain into an incompetent vein
c. Superficial venous malformations
2. Technique
a. Sclerosing agent (e.g., hypertonic saline, sodium tetradecyl [diluted or concentrated]) injected using a fine needle into the vessel
b. Results in inflammatory injury to the endothelium, thrombosis, and obliteration of the vein
c. Compression applied for 3 to 21 days, depending on provider preference
3. Risks
a. Inadvertent intra-arterial injection
b. Unexpected anaphylaxis
4. Complications
a. Hyperpigmentation most common
b. Additional complications have been listed but are rare
B. Radiofrequency Ablation (RFA)
1. Removes refluxing saphenous vein from circulation
2. Indicated for symptomatic GSV or SSV reflux with or without reflux at their corresponding deep system junctions
a. Nontortuous major saphenous tributaries such as the accessory saphenous, anterior thigh circumflex branch, and the vein of Giacomini (Acquista & Diietzek, 2011)
b. Can be performed in a physician’s office
c. Delivers temperature-controlled energy directly to the vein wall immediately contracting the luminal diameter and effects a fibrotic seal of the treated vein
d. Contraindications include nonpalpable pedal pulses, ABI <0.7, active local or systemic infection, aneurysmal segments, and AV malformation of the vein planned for treatment
e. Adverse effects: paresthesia (most common), skin burns, phlebitis, DVT, pulmonary embolism, hematoma, ecchymosis, and hyperpigmentation (Dean & Spruiell, 2011)
f. Post procedure: compression, ace wraps or graduated high thigh compression is recommended to reduce bruising and swelling in the postoperative period. The patient is encouraged to walk immediately after the procedure and 5 to 10 minutes every hour when awake. Prolonged sitting and standing should be avoided and the legs should be elevated above the heart when lying. Bruising is common and may take 6 weeks to resolve. Normal activities can be resumed in 3 to 4 days. A DVT study is recommended in 48 to 72 hours post procedure to assess for DVT (Eidt, 2012)
C. Laser Ablation
1. Minimally invasive procedure performed in a physician’s office or clinic
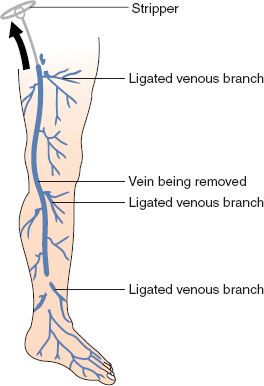
FIGURE 21.4 Vein ligation and stripping.



