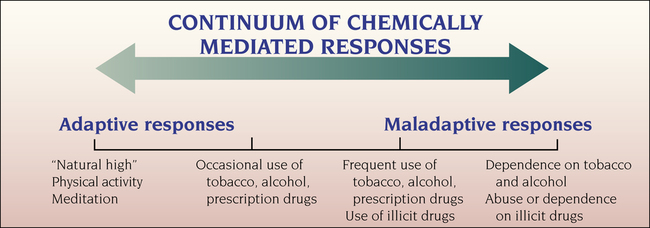
Donald L. Taylor and Gail W. Stuart 1. Describe the continuum of adaptive and maladaptive chemically mediated responses. 2. Identify behaviors associated with chemically mediated responses. 3. Analyze predisposing factors, precipitating stressors, and appraisal of stressors related to chemically mediated responses. 4. Describe coping resources and coping mechanisms related to chemically mediated responses. 5. Formulate nursing diagnoses related to chemically mediated responses. 6. Examine the relationship between nursing diagnoses and medical diagnoses related to chemically mediated responses. 7. Identify expected outcomes and short-term nursing goals related to chemically mediated responses. 8. Develop a patient education plan to promote patients’ adaptive chemically mediated responses. 9. Analyze nursing interventions related to chemically mediated responses. 10. Evaluate nursing care related to chemically mediated responses. A person may achieve a state of relaxation, euphoria, stimulation, or altered awareness in several ways. The range of these chemically mediated responses is shown in Figure 23-1. Although there is a continuum from occasional drug use to frequent drug use to abuse and dependence, not everyone who uses drugs becomes an abuser, nor does every abuser become dependent. • Substance abuse refers to continued use despite related problems. • Substance dependence indicates a severe condition, usually considered a disease. There may be physical problems and serious disruptions in the person’s work, family, and social life. • Addiction refers to the psychosocial behaviors related to substance dependence. The terms dependence and addiction are often used interchangeably. • Dual diagnosis is the co-existence of substance abuse and one or more psychiatric disorders in the same person. • Withdrawal symptoms result from a biological need that develops when the body becomes adapted to having the drug in the system. Characteristic symptoms occur when the level of the substance in the system decreases. • Tolerance means that with continued use, more of the substance is needed to produce the same effect. All nurses need to be educated about the signs of substance use, ways to screen for them, and brief interventions that they can use regardless of clinical setting (Tran et al, 2009; Mollica et al, 2011). Nurses often see substance abusers at their worst, during a medical or psychiatric crisis. They may see these patients returning repeatedly for alcohol- or drug-related health problems. The United States has one of the highest levels of substance use and addiction in the world (Table 23-1). Approximately 30% of people in the United States report having some form of alcohol use disorder at some point in their lives. TABLE 23-1 PROFILING COMMON ADDICTIONS IN THE UNITED STATES Data from Department of Health and Human Services, SAMHSA Office of Applied Studies 2009 National Survey on Drug Use and Health, www.mayoclinic.com/health/caffeine/NU00600; Center for Translational Neuroimaging, http://www.bnl.gov/medical/RCIBI/addiction.asp; Illinois Institute for Addiction Recovery, www.addictionrecov.org; Center for Internet Addiction Recovery, www.netaddiction.com; and MedicineNet.com, www.medicinenet.com/sexual_addiction. All accessed October 2011. Substance use is involved in many medical illnesses, hospitalizations, emergency room visits, and deaths. Substance use is a chronic, relapsing health problem that consumes a significant amount of health care resources. Substance users may be in treatment many times or make repeated attempts to quit before they are successful. Key facts about alcohol use and drug abuse are presented in Box 23-1. According to the National Institute on Drug Abuse, about 71% of high school seniors in the United States have used alcohol sometime in their lives. Among eighth graders, 36% have had at least one drink of alcohol, 5% report having been drunk, 20% have smoked cigarettes, and 17% have used marijuana. Among twelfth graders, 41% had consumed alcohol in the past 30 days; about 23% reported heavy alcohol consumption, called binge drinking (at least five or more drinks on one occasion within the past 2 weeks); and 3% said they consumed alcohol daily (Johnson et al, 2011; NIAAA, 2011). When examined by age groups, in 2009, 10.0% of youths ages 12 to 17 years were current drug users, compared with 9.3% in 2008. Among adults between the ages of 18 and 25 years, current drug use increased from 19.6%in 2008 to 21.2% in 2009. The rate of drug use among adults age 26 years or older increased from 5.9% in 2008 to 6.3% in 2009 (Substance Abuse and Mental Health Services Administration, 2010). Overall use of alcohol and illicit drugs increases with age until the mid-20s, levels off, and then decreases. However at-risk and binge drinking are frequently reported by middle-aged and elderly adults (Blazer and Wu, 2009). If regular use begins before age 17 years, the individual is more likely to have alcohol and illicit drug abuse and dependence problems as an adult. The lifetime prevalence and the intensity of alcohol use are greater among males. Most people with alcohol use disorders do not seek treatment (Substance Abuse and Mental Health Services Administration, 2010). It is estimated that only 11% of people in the United States who need alcohol treatment receive it. The most frequently cited reasons for not seeking alcohol treatment are cost, not wanting to stop using the substance, and not seeing the need for treatment (Edlund et al, 2009; Oleski et al, 2010). Unmet need for treatment is highest among the elderly, persons from racial-ethnic minority groups, those with low income, those without insurance, and those living in rural areas (Grella et al, 2009). • Clinicians’ lack of awareness of the symptoms or the high rates of substance disorders in psychiatric populations • Difficulty in differentiating substance disorders from psychiatric disorders • Patients’ denial, minimization, and reluctance to talk about their substance-related problems • Patients’ cognitive, psychotic, and other impairments related to their psychiatric illness Studies show that despite the high rate of dual disorders in various populations, such as those with severe and persistent mental illness, the chronically homeless, and those incarcerated in prison, the facilities and programs designed to treat both disorders are underused (Brunette et al, 2008). Screening for substance use problems is essential in the primary care setting where most people seek health care (Neushotz and Fitzpatrick, 2008; Savage, 2008; Baird, 2009; Oleski et al, 2010). Screen, Brief Intervention, Refer to Treatment (SBIRT) is a public health approach to delivering early intervention to anyone who uses alcohol or drugs in unhealthy ways (Madras et al, 2009; Robinson, 2010; Kazemi et al, 2011). The goal of SBIRT is to improve early identification of people who are overusing, abusing, or dependent on alcohol or other substances (Table 23-2). Initial screening is completed for all patients annually. When indicated by the initial screening, further evaluation using a standardized instrument such as AUDIT-C or B-DAST is done followed by a brief intervention. TABLE 23-2 SBIRT: SCREEN, BRIEF INTERVENTION, REFER TO TREATMENT Motivational interviewing skills (Chapter 2) are used as the intervention to increase insight about substance use and motivation to change. Referral to an addiction specialist or treatment facility is indicated for patients who are identified as being at risk for dependency or when use places them or others at risk for harm. SBIRT should be an essential practice skill of all nurses. The simplest biological measure to obtain is blood alcohol content (BAC) by use of a Breathalyzer. Alcohol in any amount has an effect on the central nervous system (CNS). The behaviors that can be expected from a nontolerant person at different concentrations of alcohol in the blood are shown in Table 23-3. In the United States, the legal limit as of 2011 is 0.08% blood alcohol content as measured by a breath device, urinalysis, or blood test. TABLE 23-3 COMPARISON OF BLOOD ALCOHOL CONCENTRATIONS WITH BEHAVIORAL MANIFESTATIONS OF INTOXICATION
Chemically Mediated Responses and Substance-Related Disorders
Continuum of Chemically Mediated Responses
Definition of Terms
Attitudes About Substance Abuse
Prevalence
ADDICTION
STATISTIC
Alcohol
About 18.7 million people, or about 7% of the U.S. population, are dependent on or abuse alcohol. Only about 10% of them belong to Alcoholics Anonymous. Every day, 12,500 people try alcohol for the first time.
Caffeine
The most widely used mood-altering drug in the world, caffeine, is regularly ingested by up to 90% of people in the United States. About 100 mg (one cup of coffee) per day can lead to physical dependence and withdrawal symptoms on quitting. Caffeine can alter behavior and affect sleeping habits.
Drugs
It is estimated that 3.6 million people are dependent on drugs, and 700,000 of them are in treatment for their addiction at any one time. Every day, 8000 people try drugs of abuse for the first time. Marijuana, cocaine, and pain relievers are the leading drugs of abuse.
Food addiction
Food addiction affects 4 million adults and a quickly growing number of children; binge eating is the most common eating disorder. An estimated 15% of mildly obese people are compulsive eaters.
Gambling
About 3% of adults experience a serious problem with gambling that results in significant debt, family disruption, job losses, criminal activity, or suicide.
Internet
Between 5% and 10% of the population suffer from Internet addiction, which is defined as any online-related, compulsive behavior that interferes with normal living and causes severe stress on family, friends, loved ones, and the work environment.
Sex
Sex addiction affects more than 16 million people in the United States. Addicts become dependent on the neurological changes in the brain that occur during sex. They are consumed by sexual thoughts, making it difficult to work or engage in healthy personal relationships.
Shopping
At least 1 in 20 people in the United States is a compulsive shopper, with men and women affected equally. Cultural factors, such as those emphasizing happiness associated with purchasing products, are thought to fuel shopping addictions.
Tobacco
In the United States, 69.7 million people use tobacco products. The highest rate of use is among 18 to 25 year olds and among people living in the Midwest. Approximately 25% of men and 21% of women are cigarette smokers.
Dual Diagnosis
Assessment
Screening for Substance Abuse
SBIRT
SCREENING
FOCUS
EXAMPLE
Annual (initial) screen
Screening can quickly assess the presence and severity of substance use and may be completed with an interview and self-report; important to always use supportive and nonjudgmental communication skills
How many times in the last year have you had 5 or more drinks in a day?
Or
How many days per week do you drink alcohol?
When you drink, how many drinks do you have?
Full (secondary) screen
More focused assessment
AUDIT-C, (see Box 23-2) or other screening tool
Brief intervention
Emphasis on increasing awareness of substance use, understanding the impact on health status, and encouraging behavioral change
Motivational Interviewing (see Chapter 2)
What do you enjoy about drinking/using?
What don’t you like when you drink?
From 1 to 10, how ready are you to change your drinking habits?
What change would you be able to make?
Refer to treatment
If the assessment indicates substance use placing the patient or others at risk for harm, a screening score identifying a need for specialist care, or if patient requests, provide a referral to a local treatment center
http://findtreatment.samhsa.gov/
Breathalyzer
BLOOD ALCOHOL LEVEL
BEHAVIORS
0.05-0.14 g/dL
Euphoria, labile mood, cognitive disturbances (decreased concentration, impaired judgment, loss of sexual inhibitions)
0.15-0.19 g/dL
Slurred speech, staggering gait, diplopia, drowsiness, labile mood with outbursts
0.20-0.29 g/dL
Stupor, aggressive behavior, incoherent speech, labored breathing, vomiting
0.30-0.39 g/dL
Coma
0.40-0.50 g/dL
Severe respiratory depression, death ![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Chemically Mediated Responses and Substance-Related Disorders
Get Clinical Tree app for offline access