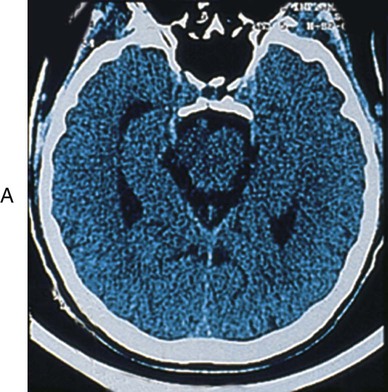
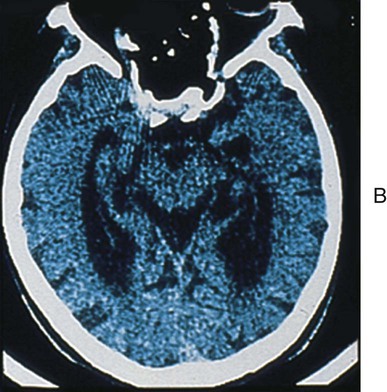
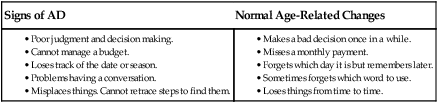
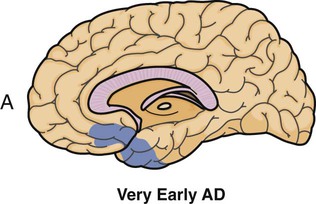
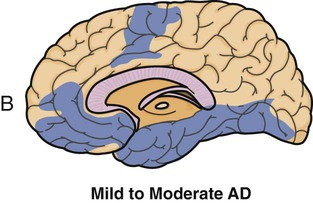
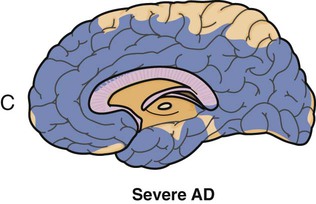
• Define the key terms and key abbreviations listed in this chapter. • Describe confusion and its causes. • List the measures that help confused persons. • Explain the differences between delirium, depression, and dementia. • Describe the signs, symptoms, and behaviors of Alzheimer’s disease (AD). • Explain the care required by persons with AD and other dementias. • Describe the effects of AD on the family. • Explain how to promote PRIDE in the person, the family, and yourself. Changes in the brain and nervous system occur with aging and certain diseases (Box 30-1). Cognitive function may be affected. (Cognitive relates to knowledge.) Quality of life is affected. Cognitive function involves memory, thinking, reasoning, ability to understand, judgment, and behavior. Acute confusion (delirium—p. 468) occurs suddenly. It is usually temporary. Causes include infection, illness, injury, drugs, and surgery. Treatment is aimed at the cause. Confusion from physical changes cannot be cured. Some measures help improve function (Box 30-2). You must meet the person’s basic needs. • Memory loss (losing things, forgetting names) • Problems with common tasks (for example, dressing, cooking, driving) • Problems with language and communication; forgetting simple words • Getting lost in familiar places • Misplacing things and putting things in odd places (for example, putting a watch in the oven) • Personality, mood, and behavior changes • Poor or decreased judgment (for example, going outdoors in the snow without shoes) Permanent dementias result from changes in the brain. The causes in Box 30-3, p. 468 have no cure. Function declines over time. Alzheimer’s disease is the most common type of permanent dementia. Alzheimer’s disease (AD) is a brain disease. Many brain cells are destroyed and die (Fig. 30-2). These functions are affected: According to the Alzheimer’s Association, the most common early symptom of AD is difficulty remembering newly learned information. The classic sign of AD is a gradual loss of short-term memory. At first, the only symptom may be forgetfulness. Box 30-5 lists the warning and other signs of AD. See Box 30-6 for the differences between AD and normal age-related changes. AD changes how a person behaves and acts. Besides the signs and symptoms in Boxes 30-5, 30-7, and 30-8, these changes are common. • Catastrophic reactions (p. 472) • Agitation and aggression (p. 472) • Communication problems (p. 473) • Repetitive behaviors (p. 474) • Changes in intimacy and sexuality (p. 474) • A strange setting. The person does not know the setting well. • Too much noise (TV, radio, music, people talking at once) can cause confusion and frustration. • Not understanding signs. The person may think that a wet floor sign means to urinate on the floor. • Mirrors. The person may think that a mirror image is another person in the room.
Caring for Persons With Confusion and Dementia
Confusion
Dementia
Alzheimer’s Disease
Signs of AD
Behaviors and Problems
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Caring for Persons With Confusion and Dementia
Get Clinical Tree app for offline access