Chapter 35. Caring for children with orthopaedic disorders
Brian Silverwood
ABSTRACT
Caring for children with an orthopaedic injury provides the nurse with a challenging and rewarding experience. Unlike most other paediatric specialties, the child admitted to the orthopaedic ward is usually well and active and requires, apart from attention to the bony injury/surgery, planning and interaction to provide him or her with play and distraction to prevent boredom. Many children’s and emergency nurses care daily for children with bony injury and therefore require a sound knowledge base both to deal with the injury and to reassure the anxious child and parent.
LEARNING OUTCOMES
• Describe bone structure, formation and resorption and the core functions of the skeleton, joints and muscles.
• Outline common childhood fractures and methods of management.
• Understand the pathophysiology of common childhood conditions and the medical/surgical treatments available.
• Devise an individualised plan of nursing care for a child who faces a period of immobility.
• Discuss the importance of discharge planning.
Glossary
Abduction
Moving a body part away from the body.
Adduction
Moving a body part towards the body.
Artho
Prefix meaning relating to a joint.
Congenital
Present at birth.
Distal
Situated further away from the area of consideration.
Dorsiflexion
Movement of hand or foot towards the dorsal surface.
Dysplasia
Abnormal development of skin, bone or other tissues.
Entonox
A self-administered inhaled pain relieving agent consisting of 50% nitrous oxide and 50% oxygen.
Equinovarus
The foot points downwards and inwards.
Equinus
The foot points downwards.
Extension
Straightening a joint.
Flexion
Bending a joint.
Hyperextension
Excessive extension.
Intramedullary
Within the medullary (inner) cavity of a long bone.
Inversion
Downwards and inwards movement of the foot.
Lateral
Situated away from the midline of the body.
Macrophage
A large scavenger cell that wanders between cells and removes bacteria and other foreign bodies from blood and tissues.
Medial
Near to the midline of the body.
Proximal
Situated close to the point of origin or attachment.
Osteoblast
A bone-forming cell.
Osteoclast
A large cell that resorbs bone.
Osteocyte
A basic bone cell.
Osteomyelitis
Inflammation of the bone due to infection.
Osteotomy
A surgical cut across the bone.
Rotation
Turning about an axis.
Sclera
Whites of the eyes.
Subluxation
Partial dislocation.
Valgus
A limb deformity in which the extremity is more away from the body’s midline.
Varus
Opposite of valgus.
Bone biology
The function of the skeletal system
The musculoskeletal system consists of 206 bones with their surrounding muscles. The main functions of the bones of the skeleton are to support and give shape to the body, to protect vital organs and to provide a system of levers that enables the body to make movements. In addition, bone serves as storage sites for certain minerals such as calcium and is also responsible for the production of red and white blood cells, a function performed by the red bone marrow. Yellow bone marrow acts as a storage site for lipids.
 Activity
Activity
 Activity
ActivityUsing a suitable anatomy and physiology textbook, or suitable online source, identify and name the different bones of the body. Examine the relative significance of each bone in relation to its main function and location within the human skeleton.
Bone structure
Bones are extremely strong and can withstand considerable forces. Bone is very resilient and can return to its normal shape after the removal of the force that caused it to become misshapen. This tensile strength and resilience is due to the framework of interwoven fibres within bone called collagen, which is a tough, white, slightly flexible material. Bones are made up of two types of tissue (Fig. 35.1):
• Compact or cortical bone: is the dense and hard part of the bone that gives the bone its shape and strength. It is made up of many rods, known as the Haversian system. These have a central canal, which contains blood vessels and nerve fibres, and is surrounded by several sheets of bone tissue called lamellae. The Haversian canals branch and interweave, giving bone great strength along lines of stress.
• Cancellous or spongy bone: is composed of fine bars of bony tissue that interlace with one another to give a honeycomb appearance. These bars of tissue are known as the trabecular bone and are strong, light and provide an excellent structure to absorb stress. The space within the trabeculae is filled by the red blood marrow.
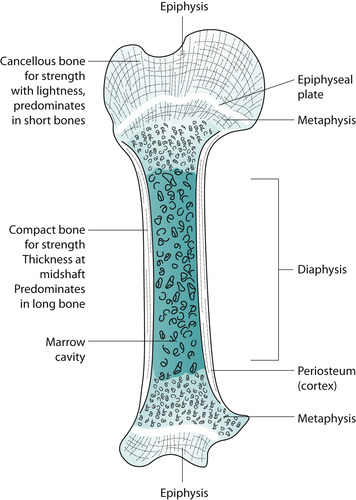 |
| Fig. 35.1 Cross-section of bone. |
All bones are covered by a layer of fibrous tissue called periosteum, which protects the bone and allows the circumference of the bone to grow.
Bone growth, formation and resorption
Bone is constantly remodelling and adapting to the daily stresses placed on our skeleton (Silverwood 2003) (Fig. 35.2). From infancy through to adolescence, bones are actively growing in length, width and density (Table 35.1). Bone remodelling is regulated by several factors including:
• mechanical loads arising from muscle forces regulate the process of bone formation and resorption. For example, a tennis player’s racket arm is typically stronger and wider than a non-player’s arm because the remodelling bone has adapted to the increased daily strain and loading experienced when serving the ball
• calcium: this is the most abundant mineral found within the body. It is arranged around the matrix of collagen, which gives bone its strength and rigidity. Calcium is stored in the bone and released when serum calcium levels are low. A normal serum calcium level is required to allow adequate muscle contraction, transmission of impulses across nerve cells, activities of some enzymes and the building of strong bones
• parathyroid hormone (PTH): controls distribution of calcium. When serum calcium concentrations are low the hormone causes increased calcium absorption from the intestines, calcium reabsorption by the kidneys and increased bone resorption. Parathyroid hormone also regulates the synthesis of the active metabolites of vitamin D, which also enhance absorption of calcium from the intestine.
• sex hormones: oestrogen and testosterone provide a ‘control’ over bone resorption and keeps bone remodelling in homeostasis.
 |
| Fig. 35.2 Bone remodelling (reproduced with permission from Silverwood 2003.) |
| Infancy | Rapid growth in proportion and size as calcium is added to cartilage-like bones |
| Calcium content in relation to body size increases faster than any other stage of life | |
| Childhood | Growth continues |
| Bone density and thickness increase | |
| Bone formation outpaces resorption | |
| Adolescence | Growth accelerates |
| Bone growth peaks around ages 12–17 in boys and ages 11–15 in girls | |
| Bone density and thickness increase | |
| Bone formation outpaces resorption | |
| Age 20 | 90% of peak bone mass achieved |
| Age 35 | Peak bone mass achieved |
| Note: Peak bone mass is about 30% higher in men than women | |
| Age 40 | Bone resorption begins to outpace formation |
| Adult bone loss occurs at a rate of 6–8% per decade |
Fracture repair and bone healing
The fractured ends of the bone bleed and form a clot. The inflammatory healing process commences and the dead tissue and clot is removed by macrophages. The initial strands from the blood clot begin to change into osteoid tissue, which develops and forms callus around the fracture site; osteoclasts remove necrotic bone and osteoblasts develop new bone (Apley & Solomon 2001). Between 6 and 12 weeks, as the callus hardens, the bone regains some mechanical strength. Further callus maturity occurs between 12 and 26 weeks. By 1–2 years bone remodelling has occurred (see Fig. 35.2) and normal bone shape has been restored. Unlike adults, children can restore bony deformity resulting from a significant (up to 30°) malalignment through bone remodelling (Danby & Edwards 2001).
Joints
A joint or articulation is where two or more bones are in close contact with each other. Joints are classified according to their mobility and structure into fibrous, cartilaginous or synovial. Fibrous joints exist between bone and cartilage. The surfaces are simply joined by fibrous tissue and there is little or no movement. Cartilaginous joints allow a small degree of movement and are covered by layers of cartilage linked by a thick pad of tissue, for example, between vertebral bones. Synovial joints, which include all limb joints, permit a great deal of movement and are the most common type of joint. Hyaline cartilage covers the articulating surfaces to prevent friction and a fibrous capsule encloses the joint and helps hold the bones in place. A synovial membrane lines the capsule, which secretes synovial fluid to lubricate the structure.
 Activity
Activity
 Activity
ActivityIdentify the differing types of joint within the human skeleton and justify the joint type in relation to its function and location.
Skeletal muscle
The skeletal muscles are known as voluntary muscles because they produce movement under voluntary control. These muscles are composed of large elongated cells known as muscle fibres, which are bound together by connective tissue into small bundles and are further bound into larger bundles forming the muscle. Each muscle is enveloped in a sheet of fibrous tissue known as the fascia, which is continuous with the tendon. Tendons are composed of bands of fibrous tissue, which attach muscles to bones.
Muscle activity is coordinated and most muscles work in pairs or groups; muscle tissue is capable of contraction and relaxation and may be stimulated by nervous, chemical, electrical or thermal stimulation.
Fractures
A fracture is quite simply a break in the continuity of bone. Most fractures are diagnosed from the description of the injury and the physical appearance of the limb, confirmed by plain X-ray. Physical signs and symptoms of a fracture may include (Danby and Edwards, 2001 and Pagdin, 1996):
• pain, which may be throbbing or localised: the pain is often aggravated by active or passive movement
• impaired, or loss of, function due to pain and the nature of the fracture
• swelling at the fracture site caused by oedema/haematoma formation. Usually increases in the first 12–24 hours following injury
• a deformity may be seen or felt
• abnormal movement in a particular limb due to movement at the fracture site
• tenderness and/or bruising at the fracture site
• crepitus (grating) heard or felt when the ends of the broken bone are un-deliberately rubbed together.
Types of fracture
There are many descriptions of fractures, depending on the nature of the injury and the force that causes the fracture (Fig. 35.3). In children, a fracture through the epiphyseal (growth) plate may result in interference or complete cessation of bone growth of that long bone, which will produce a limb-length discrepancy. These fractures are known as epiphyseal fractures and are classified into five types (Fig. 35.4).
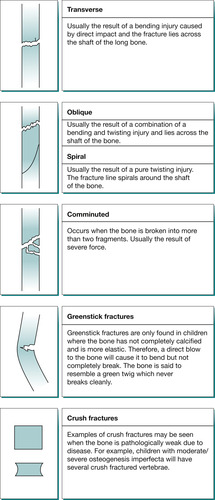 |
| Fig. 35.3 Types of fracture. |
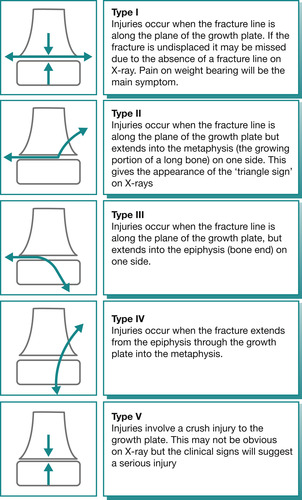 |
| Fig. 35.4 Epiphyseal fractures. |
Other descriptions of fractures
A fracture may be displaced or undisplaced. An undisplaced fracture is one in which the bone ends are lined up, whereas in a displaced fracture the bone ends or fracture fragments are out of alignment and will require correction.
Open (compound) fractures are fractures in which the soft tissue and skin envelope have been disrupted by, for example, the acute angulation of the fracture which breaks through the skin. Such fractures are in immediate danger of infection and risk development of osteomyelitis. Most fractures do not break through the skin and are called closed fractures.
Intra-articular fractures may present where the fracture involves the joint surface. If there is a step or gap in the joint surface this may need surgery to correct it.
Fracture complications
There are many potential associated complications with fractures including the following:
• Infection: in open fractures, a wound infection may spread from the skin and soft tissues and infect the underlying bone. Often, children are at increased risk due to the activity at the time of fracture, which may involve dirt, grit or grass. The child with an open wound should have the wound cleaned and be commenced on systemic antibiotic therapy. If the wound is very dirty it will be left open, dressed appropriately and then closed later on.
• Malunion: this is when the fracture heals in the wrong position/alignment. This may be due to poor reduction or the result of an unstable fracture that slips following reduction. It is important that all children with fractures are seen afterwards as frequently as needed to ensure the bone heals in the right position.
• Delayed union: this complication occurs for a variety of reasons. It may be because the blood supply to the fracture is poor or the fracture is inadequately immobilised. The fracture heals but takes longer than expected.
• Non-union: the fracture fails to heal. This may be due to infection, trapped soft tissues or local bone necrosis.
• Avascular necrosis: the blood supply becomes disturbed to the bone fragments causing failure to heal. It may not present until some time following the injury.
• Damage to structures: in severe fractures other structures may be affected, for example, ischaemia to blood vessels, nerves, organs.
• Compartment syndrome: the fascial compartments within the upper and lower limbs are at risk when bleeding occurs into them from the fracture. The closed non-elastic space fills with blood and increases the pressure on the venous drainage, thereby raising the pressure in the compartment. This starves the muscle cells of oxygen and they die. The circulation can also be disturbed by a bone fragment or very tight plaster cast. The signs and symptoms of compartment syndrome in an upper limb may include:
• painful clawing of the fingers with increasing pain on passive extension of the fingers
• altered sensation, including a burning sensation or patchy loss of sensation
• the pulse is weak, intermittent or absent
• the fingers are cold and bluish
• weak ability to flex the fingers.
Many texts describe these signs of compartment syndrome as the five Ps:
• Pallor
• Paraesthesia
• Paralysis
• Pain
• Pulselessness.
The main symptom to note is pain, which is out of proportion to the injury and which is intractable. This condition needs to be recognised early because it is limb-threatening and prompt surgical attention can save the limb.
Neurovascular observations
When a child enters the hospital with a fracture, the neurovascular status should be assessed initially, then half-hourly for 4 hours, then hourly for 12–24 hours prior to and following repair of the fracture. This involves assessing colour, sensation, temperature, pulse and movement of the limb. Any alteration of these observations should be reported immediately to the orthopaedic team.
 PROFESSIONAL CONVERSATION
PROFESSIONAL CONVERSATION
Rebecca is a newly qualified registered children’s nurse on Part 15 of the NMC register.
 PROFESSIONAL CONVERSATION
PROFESSIONAL CONVERSATIONRebecca is a newly qualified registered children’s nurse on Part 15 of the NMC register.
Yesterday we had a young boy who had a supracondylar fracture to his left elbow. I observed when checking neurovascular observations that his fingers were very dusky and when I tried to extend his fingers he was screaming out in pain. I was very concerned but didn’t really feel very confident so I went to ask the ward manager but she was busy with a parent. I remembered what my preceptor had told me so I contacted the orthopaedic registrar. He came to the ward immediately and within 20 minutes the child was being escorted to theatre for a fasciotomy to release the pressure on his brachial artery. Later the registrar came and thanked me. He said I had probably saved the boy from developing Volkmann’s ischaemia or losing his arm. I am really glad I listened to my preceptor and now really do realise the importance of neurovascular observations. 

Failure to recognise a compartment syndrome of the forearm may result in the child developing Volkmann’s ischaemic contracture caused by progressive muscle necrosis. The muscle is replaced by scar tissue leading to flexion contractures and clawing of the fingers. The result of this condition involves operations to release forearm flexors, muscle slide and tendon lengthening. Prevention through diagnosis would be attained by restoration of blood flow through reduction of compartmental pressure.
Treatment of fractures
The five Rs summarise the five main aims of fracture treatment:
 Activity
Activity
1. Resuscitation: the child with a fracture should rarely require fluid resuscitation, but the nurse should be aware of the signs and treatment necessary for shock. In fractures, shock may be related to pain and blood loss.
2. Reduction: describes the realignment of the fractured bone ends. The best reduction will take place under general anaesthesia where the surgeon can manipulate the bone and observe the correction using an image intensifier. This is especially relevant to children in whom it would not be acceptable to attempt reduction using sedation in the casualty department. Alignment may be acceptable in children with greenstick fractures.
3. Restriction: after the fracture has been manipulated into a good position it needs to be held until bony union occurs (usually 6 weeks in children). The methods used to hold the fracture will depend on the bone affected and the nature of the injury and will include one of:
• plaster cast
• traction
• internal or external fixation.
The aim of restriction is to prevent any deformity and allow bone growth to proceed normally.
4. Restoration: when a limb is immobilised there is a risk that the muscles and joints will stiffen and lose some function. Therefore it is important that the child is encouraged to exercise all joints and muscles except those affected by the injury. For example, a child with a fractured distal radius who has an above-elbow cast can be encouraged to exercise all digits, which keeps the fingers nimble, encourages the muscle to move within the cast and promotes venous return.
 Activity
ActivityA child presents with head injury and an open fractured femur following a road traffic accident.
• What immediate nursing and medical approach should be taken to resuscitate this 7-year-old child who has deteriorating consciousness and in hypovolaemic shock?
• Prioritise and analyse each intervention in relation to how it will stabilise the child’s condition.
Methods of holding fractures
Plaster casts
Plaster casts hold a number of advantages for the child with a fracture, including:
• allowing the child to mobilise and perform most activities of daily living
• low cost and readily available
• light and porous, which allows the skin to breathe
• relatively easy to use and apply
• strong, providing protection
• permeable to X-rays.
Disadvantages include:
 Reflect on your practice
Reflect on your practice
• it may cause discomfort including itching and feel heavy and warm and a child will be tempted to push toys and small objects down the cast leading to pressure sores
• it may hide developing problems:
• a poorly applied cast may cause pressure on the skin and encourage the development of a pressure ulcer
• a surgical wound following an open reduction may develop sepsis
• it is not waterproof.
 Reflect on your practice
Reflect on your practiceConsider what education and skills you need to be competent in the application of a plaster cast.
In what way does this relate to your professional accountability and the recommendations of the British Orthopaedic Association (BOA)?
Plaster casts – nursing care
Prior & Miles (1999) considered the following when caring for an inpatient with a plaster cast:
• Care should be taken not to apply pressure to the cast during the drying period to avoid causing dents in the cast (plaster of Paris takes 24–48 hours to dry; synthetic, fibreglass casts take around 30–60 minutes). The limb should be supported on a pillow to provide even pressure along the cast which prevents undue pressure on bony prominences.
• Elevation of the limb may be necessary to help reduce the amount of swelling which, within a cast, may cause constriction and neurovascular impairment.
Plaster casts – observations
• The cast should be observed regularly for cracking, softening or breakdown.
• If a child has had an open reduction, the cast should be observed for blood loss, which will stain the cast. A line drawn around the cast illustrates any further blood loss.
• Neurovascular observations should be performed, see p 530.
• When the child has recovered and appears stable the cast may need trimming to improve comfort. Hip spica casts will need protection around the edges to prevent contamination by urine and faeces.
Before a child is discharged home, the parent and child should receive advice regarding care of the plaster (sample discharge advice in companion PowerPoint presentation). See p 538-9 for nursing and discharge care for a hip spica cast.
Get Clinical Tree app for offline access




