Chapter 38 Care of Patients with Vascular Problems
Safe and Effective Care Environment
1. Collaborate with interdisciplinary health care team members when providing care for patients with vascular problems.
Health Promotion and Maintenance
2. Identify risk factors for vascular problems.
3. Teach patients about lifestyle modifications to prevent vascular problems.
4. Explain the pathophysiology of arteriosclerosis and atherosclerosis.
5. Interpret essential laboratory data related to risk for atherosclerosis.
6. Discuss the role of nutrition therapy in the management of patients with arteriosclerosis.
7. Describe the differences between essential and secondary hypertension.
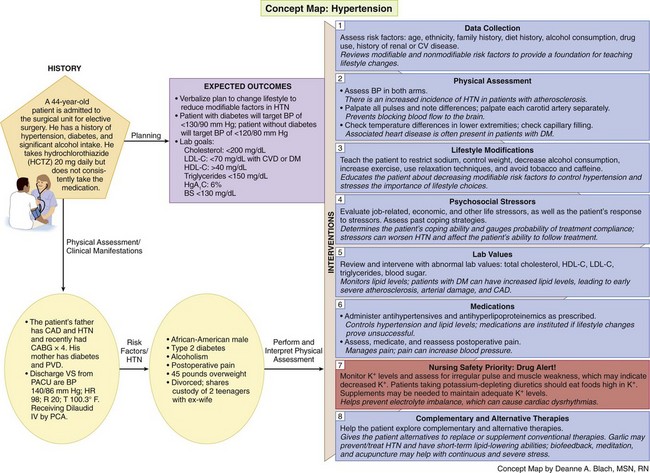
8. Develop a collaborative plan of care for a patient with essential hypertension.
9. Develop a teaching plan for patients on adverse effects of drugs for hypertension and when to notify the health care provider.
10. Compare common assessment findings present in patients with peripheral arterial and peripheral venous disease.
11. Identify when venous thromboembolism (VTE) and complications of VTE occur.
12. Plan nursing interventions to help prevent VTE.
13. Describe the nurse’s role in monitoring patients who are receiving anticoagulants.
14. Monitor for complications of vascular surgery.
15. Perform a focused vascular assessment.
16. Compare assessment findings associated with Raynaud’s phenomenon and Buerger’s disease.
http://evolve.elsevier.com/Iggy/
Animation: Abdominal Aortic Aneurysm
Animation: Physiology of Blood Pressure
Answer Key for NCLEX Examination Challenges and Decision-Making Challenges
Review Questions for the NCLEX® Examination
Arteriosclerosis and Atherosclerosis
Pathophysiology
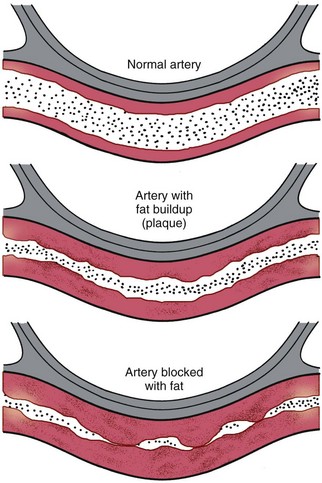
The exact pathophysiology of atherosclerosis is not known, but the condition is thought to occur from blood vessel damage that causes an inflammatory response (see the discussion of inflammation in Chapter 19) (Fig. 38-1). After the vessel becomes inflamed, a fatty streak appears on the intimal surface (inner lining) of the artery. Through the process of cellular proliferation, collagen migrates over the fatty streak, forming a fibrous plaque. The fibrous plaque is often elevated and protrudes into the vessel lumen, partially or completely obstructing blood flow through the artery. Plaques are either stable or unstable. Unstable plaques are prone to rupture and are often clinically silent until they rupture (McCance et al., 2010).
When stable plaque ruptures, thrombosis (blood clot) and constriction obstruct the vessel lumen, causing inadequate perfusion and oxygenation to distal tissues. Unstable plaque rupture causes more severe damage. After the rupture occurs, the exposed underlying tissue causes platelet adhesion and rapid thrombus formation. The thrombus may suddenly block a blood vessel, resulting in ischemia and infarction (e.g., myocardial infarction) (McCance et al., 2010).
Endothelial (intimal) injury of the major arteries of the body can be caused by many factors. Elevated levels of lipids (fats) like low-density lipoprotein cholesterol (LDL-C) and decreased levels of high-density lipoprotein cholesterol (HDL-C) can cause chemical injuries to the vessel wall. (Chapter 35 discusses lipids in detail.) Chemical injury can also be caused by elevated levels of toxins in the bloodstream, which may occur with renal failure or by carbon monoxide circulating in the bloodstream from cigarette smoking. The vessel wall can be weakened by the natural process of aging or by diseases such as hypertension.
Genetic predisposition and diabetes have a major effect on the development of atherosclerosis. Some patients have familial hyperlipidemia, an elevation of serum lipid levels. In these people, the liver makes excessive cholesterol and other fats. However, some people with hereditary atherosclerosis have a normal blood cholesterol level. The reason for the development and progression of plaque in these patients is not understood (McCance et al., 2010).
Other factors are indirectly related to atherosclerosis development. A list of risk factors is found in Table 38-1.
TABLE 38-1 RISK FACTORS FOR ATHEROSCLEROSIS
HDL-C, High-density lipoprotein cholesterol; LDL-C, low-density lipoprotein cholesterol.
Patient-Centered Collaborative Care
Assessment
Laboratory Assessment
Patients with atherosclerosis often have elevated lipids, including cholesterol and triglycerides. Total serum cholesterol levels should be below 200 mg/dL. Elevated cholesterol levels are confirmed by HDL and LDL measurements. Increased low-density lipoprotein cholesterol (LDL-C) (“bad” cholesterol) levels indicate that a person is at an increased risk for atherosclerosis. Low high-density lipoprotein cholesterol (“good” cholesterol) (HDL-C) levels also indicate an increased risk. A desirable LDL-C level is one below 100 mg/dL for healthy people and below 70 mg/dL for those diagnosed with CVD or who are diabetic. A desirable HDL-C level is 40 mg/dL or above (Pagana & Pagana, 2010).
Triglyceride level may also be elevated with atherosclerosis and is an emerging lipid risk factor by the classic Adult Treatment Panel Report No. 3 (ATP III) released by the National Heart, Lung, and Blood Institute (National Cholesterol Education Program, 2002). A level of 150 mg/dL or above indicates hypertriglyceridemia. Women should have a level below 135 mg/dL (Pagana & Pagana, 2010). Elevated triglycerides are considered a marker for other lipoproteins. They also suggest metabolic syndrome, which increases the risk for coronary heart disease (see Table 40-1 and discussion in Chapter 40).
Interventions
• Patients with diabetes but without signs of vascular disease
• Patients with a Framingham Heart Study 10-year absolute risk score of over 20% for coronary heart disease events
Interventions for patients with atherosclerosis or those at high risk for the disease focus on lifestyle changes. Teach patients about the need to make daily changes by avoiding or minimizing modifiable risk factors. Modifiable risk factors are those that can be changed or controlled by the patient, such as smoking, weight management, and exercise. Nutrition is one of the most important parts of the risk-reduction plan. Chapter 40 describes how to manage modifiable risk factors in detail in the Health Promotion and Maintenance section, p. 831. If lipoprotein levels do not improve after lifestyle changes, the health care provider may prescribe drug therapy to lower cholesterol and/or triglycerides.
Nutrition Therapy
The Nutrition Committee of the American Heart Association (AHA) established dietary guidelines to promote healthy dietary habits as a strategy to reduce the risk for cardiovascular disease. The guidelines, revised in 2006, focus on the need to achieve and maintain a healthy weight and make appropriate food choices. Although most research focuses on individual nutrients or foods, the AHA guidelines aim to improve overall diet to ensure nutrient adequacy and energy balance (Lichtenstein et al., 2006). The AHA recommends that people consume a variety of nutritious foods including fruits, vegetables, whole grains, fat-free and low-fat dairy products, and lean meats. Specific AHA guidelines to decrease the risk for cardiovascular disease include minimizing fat and cholesterol intake. Chapter 63 describes the most recent U.S. government dietary guidelines, which include increasing daily vegetables and decreasing dairy food fats.
Drug Therapy
For patients with elevated total and LDL-C levels that do not respond adequately to dietary intervention, the health care provider prescribes one or more lipid-lowering agents (Table 38-2). Drug choice depends on the serum lipid levels. Because most of these drugs can produce major side effects, they are generally given only when nonpharmacologic management has been unsuccessful.
TABLE 38-2 COMMONLY USED DRUGS FOR ATHEROSCLEROSIS
HMG-CoA Reductase Inhibitors (Statins) |
HMG-CoA, 3-hydroxy-3-methylglutaryl coenzyme A.
Drug Alert
Complementary and Alternative Therapy
Lovaza (omega-3 ethyl esters) is approved by the Food and Drug Administration (FDA) as an adjunct to diet to reduce TGs that are greater than 500 mg/dL. This drug also decreases plaque growth and inflammation and reduces clot formation (Harris et al., 2008).
Health Promotion and Maintenance
Hypertension
Pathophysiology
According to the Seventh Joint National Committee (JNC) on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure, hypertension is a systolic blood pressure at or above 140 mm Hg and/or a diastolic blood pressure at or above 90 mm Hg in people who do not have diabetes mellitus. Patients with diabetes and heart disease should have a blood pressure below 130/90 (Joint National Committee, 2003). The Eighth JNC report, due to be released by the U.S. National Institutes of Health in Spring 2012, may likely recommend different values and classifications of patients who are hypertensive.
Mechanisms That Influence Blood Pressure
• The arterial baroreceptor system
• Regulation of body fluid volume
• The renin-angiotensin/aldosterone system
Arterial baroreceptors are found primarily in the carotid sinus, aorta, and wall of the left ventricle. They monitor the level of arterial pressure and counteract a rise in arterial pressure through vagally mediated cardiac slowing and vasodilation with decreased sympathetic tone. Therefore reflex control of circulation elevates the systemic arterial pressure when it falls and lowers it when it rises. Why baroceptor control fails in hypertension is not clear (McCance et al., 2010).
The renin-angiotensin-aldosterone system also regulates blood pressure (see discussion in Chapter 13). The kidney produces renin, an enzyme that acts on angiotensinogen (a plasma protein substrate) to split off angiotensin I, which is converted by an enzyme in the lung to form angiotensin II. Angiotensin II has strong vasoconstrictor action on blood vessels and is the controlling mechanism for aldosterone release. Aldosterone then works on the collecting tubules in the kidneys to reabsorb sodium. Sodium retention inhibits fluid loss, thus increasing blood volume and subsequent blood pressure.
Classifications of Hypertension
In 2003 the JNC made significant changes in classifying blood pressure in adults. The classification for “normal” adult blood pressure is less than 120 mm Hg systolic and less than 80 mm Hg diastolic. Adults with a blood pressure (BP) of 120 to 139 mm Hg systolic or 80 to 89 mm Hg diastolic, considered “normal” under previous guidelines, are classified as prehypertensive. These patients need lifestyle changes to prevent cardiovascular complications (Table 38-3). The relationship between hypertension and cardiovascular events is direct and independent of other risk factors. The higher the patient’s blood pressure is, the greater the chance for coronary, cerebral, renal, and peripheral vascular disease.
TABLE 38-3 BLOOD PRESSURE CLASSIFICATION
| CLASSIFICATION | BLOOD PRESSURE MEASUREMENT | BLOOD PRESSURE READINGS |
|---|---|---|
| Normal | Systolic and diastolic | <120 mm Hg <80 mm Hg |
| Prehypertension | Systolic or diastolic | 120-139 mm Hg 80-89 mm Hg |
| Stage 1: Hypertension | Systolic or diastolic | 140-159 mm Hg 90-99 mm Hg |
| Stage 2: Hypertension | Systolic or diastolic | ≥160 mm Hg ≥100 mm Hg |
From Joint National Committee. (2003). The Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. NIH Publication No. 03-5233. Bethesda, MD: National Heart, Lung, and Blood Institute.
Control of hypertension has resulted in major decreases in cardiovascular morbidity and mortality. The Healthy People 2020 campaign includes a number of objectives related to hypertension to decrease cardiovascular mortality (Table 38-4).
TABLE 38-4 MEETING HEALTHY PEOPLE 2020 OBJECTIVES
Data from www.healthypeople.gov/2020.
Hypertension can be essential (primary) or secondary (Table 38-5). Essential hypertension is the most common classification. Sustained BP elevation in patients with essential hypertension results in damage to vital organs by causing medial hyperplasia (thickening) of the arterioles. As the blood vessels thicken and perfusion decreases, body organs are damaged. These changes can result in myocardial infarctions, strokes, peripheral vascular disease (PVD), or renal failure.
TABLE 38-5 ETIOLOGY OF HYPERTENSION
Isolated systolic hypertension (ISH) is a major health threat, especially for older adults. It is defined as a systolic BP (SBP) reading at or above 140 with a diastolic BP (DBP) below 90. For years, emphasis was placed on the diastolic BP (DBP) reading and attempts were made to lower this number to under 80. However, as people age, the systolic BP (SBP) becomes more significant because it is a better indicator than DBP of risk for heart disease and stroke. Research has shown that DBP rises until age 55 years and then declines, whereas SBP continues to rise. New research demonstrates a significant association between isolated systolic hypertension and peripheral vascular disease (Safar et al., 2009). In older adults, isolated systolic hypertension is the most common form of hypertension.
Etiology and Genetic Risk
Essential hypertension can develop when a patient has any one or more of the risk factors listed in Table 38-5.
Incidence/Prevalence
One in every three American adults has high blood pressure or is being treated for hypertension (AHA, 2010). The disease shortens life expectancy. A higher percentage of men than women have hypertension until age 45 years. From 45 to 54 years, women have a slightly higher percentage of hypertension than men. After age 54 years, women have a much higher percentage of the disease (AHA, 2010). The causes for these differences are not known.
The prevalence of hypertension in African Americans in the United States is among the highest in the world and is constantly increasing. When compared with Euro-Americans, they develop high BP earlier in life, making them much more likely to die from strokes, heart disease, and kidney disease (AHA, 2010). The exact reasons for these differences is not known, but genetics and environmental factors may play a role. Efforts to raise awareness of hypertension within African-American communities, including the importance of receiving treatment and controlling blood pressure, have been somewhat successful. Geographic differences still exist (Lloyd-Jones et al., 2010).
Patient-Centered Collaborative Care
Assessment
Physical Assessment/Clinical Manifestations
When a diagnosis of hypertension is made, most people have no symptoms. However, patients may experience headaches, facial flushing (redness), dizziness, or fainting as a result of the elevated blood pressure. Obtain blood pressure readings in both arms. Two or more readings may be taken at each visit (Fig. 38-2). Some patients have high blood pressure due to anxiety associated with visiting a health care provider. Be sure to take an accurate blood pressure by using an appropriate-size cuff. Anderson et al. (2010) found that forearm blood pressure measurements are as accurate as upper arm blood pressures, especially in patients who are obese. In ambulatory care settings, such as clinics and office practices, wrist blood pressure measurements can be used.
Diagnostic Assessment
Although no laboratory tests are diagnostic of essential hypertension, several laboratory tests can assess possible causes of secondary hypertension. Kidney disease can be diagnosed by the presence of protein, red blood cells, pus cells, and casts in the urine; elevated levels of blood urea nitrogen (BUN); and elevated serum creatinine levels. The creatinine clearance test directly indicates the glomerular filtration ability of the kidneys. The normal value is 107 to 139 mL/min for men and 87 to 107 mL/min for women (Pagana & Pagana, 2010). Decreased levels indicate kidney disease.
An electrocardiogram (ECG) determines the degree of cardiac involvement. Left atrial and ventricular hypertrophy is the first ECG sign of heart disease resulting from hypertension. Left ventricular remodeling can be detected on the 12-lead ECG (see Chapter 40 for discussion of remodeling).
Planning and Implementation
Health Teaching
Interventions.
Lifestyle Changes.
In collaboration with the health care team, teach the patient to:
• Restrict sodium intake in the diet
• Reduce weight, if overweight or obese
• Use relaxation techniques to decrease stress
Strategies to help patients make these changes are discussed in Chapter 40.
Complementary and Alternative Therapies.
Garlic has been used for centuries for a number of health problems, but evidence to support its use to prevent hypertension is controversial. Evidence by consensus and case reports does support garlic’s cholesterol-lowering ability and its ability to decrease blood pressure in patients with hypertension (National Center for Complementary and Alternative Medicine, 2010). Teach patients to check with their health care provider before starting garlic or any herbal therapy because of possible side effects and interactions with other herbs, foods, or drugs. Garlic can affect the liver and cause bleeding in some patients, especially if they have invasive procedures such as surgery.
Drug Therapy.
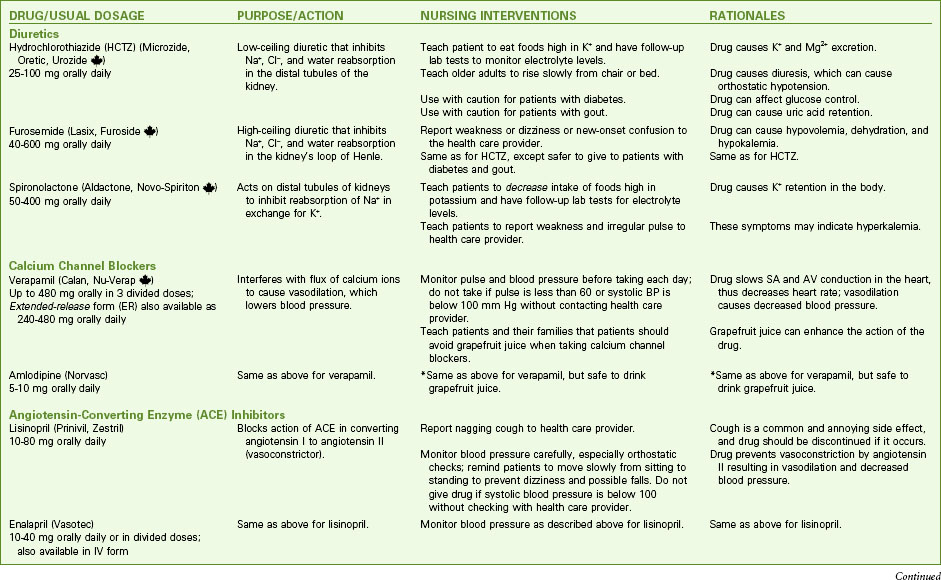
In the largest hypertensive trial done to date, Antihypertensive and Lipid-Lowering Treatment to Prevent Heart Attack Trial (ALLHAT), the use of diuretics has been practically unmatched in preventing the cardiovascular complications of hypertension. Calcium channel blockers, angiotensin-converting enzyme (ACE) inhibitors, angiotensin II receptor antagonists, and aldosterone receptor antagonists may also be given. Examples of commonly used drug classes for hypertension are listed in Chart 38-1.
Diuretics are the first type of drugs for managing hypertension (Cranwell-Bruce, 2008). Three basic types of diuretics are used to decrease blood volume and lower blood pressure in order of how commonly they are prescribed:
• Thiazide (low-ceiling) diuretics, such as hydrochlorothiazide (HydroDIURIL, Microzide, Oretic, Urozide ![]() ), inhibit sodium, chloride, and water reabsorption in the distal tubules while promoting potassium, bicarbonate, and magnesium excretion. However, they decrease calcium excretion, which helps prevent kidney stones and bone loss (Cranwell-Bruce, 2008). Because of the low cost and high effectiveness of thiazide-type diuretics, they are usually the drugs of choice for patients with uncomplicated hypertension. These drugs can be prescribed as a single agent or in combination with other classes of drugs.
), inhibit sodium, chloride, and water reabsorption in the distal tubules while promoting potassium, bicarbonate, and magnesium excretion. However, they decrease calcium excretion, which helps prevent kidney stones and bone loss (Cranwell-Bruce, 2008). Because of the low cost and high effectiveness of thiazide-type diuretics, they are usually the drugs of choice for patients with uncomplicated hypertension. These drugs can be prescribed as a single agent or in combination with other classes of drugs.
Drug Alert
• Loop (high-ceiling) diuretics, such as furosemide (Lasix, Furoside ![]() ) and torsemide (Demadex), inhibit sodium, chloride, and water reabsorption in the ascending loop of Henle and promote potassium excretion.
) and torsemide (Demadex), inhibit sodium, chloride, and water reabsorption in the ascending loop of Henle and promote potassium excretion.
• Potassium-sparing diuretics, such as spironolactone (Aldactone, Novospiroton ![]() ), triamterene (Dyrenium), and amiloride (Midamor), act on the distal renal tubule to inhibit reabsorption of sodium ions in exchange for potassium, thereby retaining potassium in the body. When used, they are typically in combination with another diuretic or antihypertensive drug to conserve potassium.
), triamterene (Dyrenium), and amiloride (Midamor), act on the distal renal tubule to inhibit reabsorption of sodium ions in exchange for potassium, thereby retaining potassium in the body. When used, they are typically in combination with another diuretic or antihypertensive drug to conserve potassium.
Calcium channel blockers such as verapamil hydrochloride (Calan, Nu-Verap ![]() ) and amlodipine (Norvasc) lower blood pressure by interfering with the transmembrane flux of calcium ions. This results in vasodilation, which decreases blood pressure. These drugs also block SA and AV node conduction, resulting in a decreased heart rate. Calcium channel blockers are most effective in older adults and African Americans (Cranwell-Bruce, 2008).
) and amlodipine (Norvasc) lower blood pressure by interfering with the transmembrane flux of calcium ions. This results in vasodilation, which decreases blood pressure. These drugs also block SA and AV node conduction, resulting in a decreased heart rate. Calcium channel blockers are most effective in older adults and African Americans (Cranwell-Bruce, 2008).
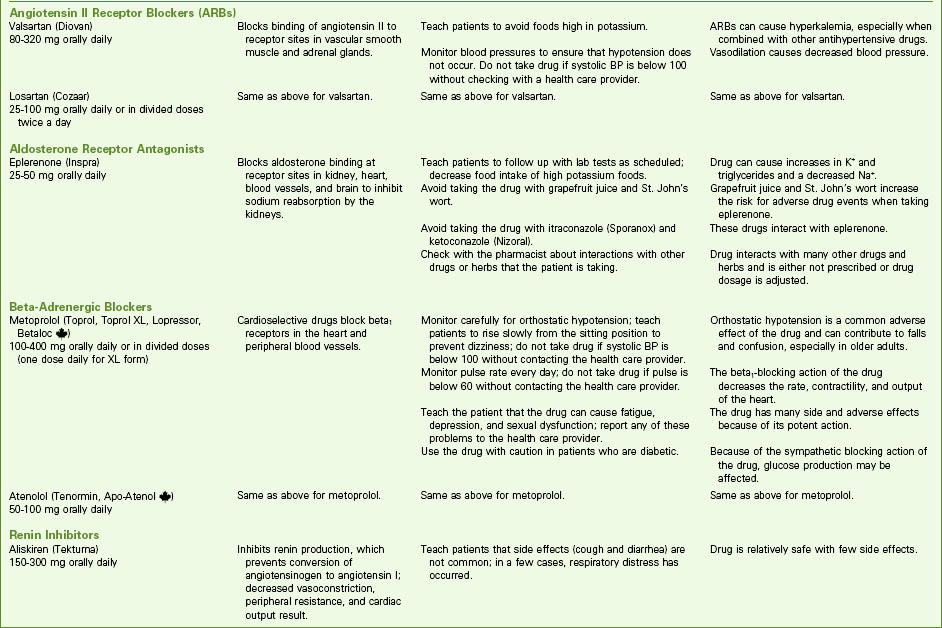
Drug Alert
Angiotensin II receptor antagonists, also called angiotensin II receptor blockers (ARBs) or the -sartan drugs, make up a group of drugs that selectively block the binding of angiotensin II to receptor sites in the vascular smooth muscle and adrenal tissues by competing directly with angiotensin II but not inhibiting ACE (Cranwell-Bruce, 2008). Examples of drugs in this group are candesartan (Atacand), valsartan (Diovan), and losartan (Cozaar). ARBs can be used alone or in combination with other antihypertensive drugs. These drugs are excellent options for patients who report a nagging cough associated with ACE inhibitors. In addition, these drugs do not require initial adjustment of the dose for older adults or for any patient with renal impairment. Like the ACEs, the ARBs are not as effective in African Americans unless these drugs are taken with diuretics or another category such as a beta blocker or calcium channel blocker (AHA, 2010).
Drug Alert
Beta blockers are the drug of choice for hypertensive patients with ischemic heart disease (IHD) because the heart is the most common target of end-organ damage with hypertension. If this drug is not tolerated, a long-acting calcium channel blocker can be used. In patients with unstable angina or myocardial infarction (MI), beta blockers or calcium channel blockers should be used initially in combination with ACE inhibitors or ARBs, with addition of other drugs if needed to control the blood pressure. Best practice for controlling hypertension in post–myocardial infarction (MI) patients includes a combination therapy of beta blockers, ACE inhibitors or ARBs (not as common), and aldosterone antagonists plus intense management of lipids and the use of aspirin. Low-dose aspirin should be considered only once the blood pressure is controlled because of the increased risk for hemorrhagic stroke in patients with uncontrolled hypertension. Patients who are prehypertensive may also benefit from low-dose daily aspirin (Hermida et al., 2009).
Physiological Integrity
Promoting Adherence to the Plan of Care
Interventions.
Patients who do not adhere to antihypertensive treatment are at a high risk for target organ damage and hypertensive urgency or crisis (causes organ damage, such as kidney or heart [target organs]) (Chart 38-2). Patients in hypertensive crisis are admitted to critical care units, where they receive IV antihypertensive therapy such as nitroprusside (Nipride), nicardipine (Cardene IV), fenoldopam (Corlopam), or labetalol (Normodyne). These drugs act quickly as vasodilators to decrease blood pressure (BP). When the patient’s blood pressure stabilizes, oral antihypertensive drugs are given (Horne & Gordon, 2009).
Chart 38-2 Best Practice for Patient Safety & Quality Care
Emergency Care of Patients with Hypertensive Urgency or Crisis
Intervene
• Place patient in a semi-Fowler’s position.
• Start IV of 0.9% normal saline (NS) solution slowly to prevent fluid overload (which would increase blood pressure).
• Administer IV nitroprusside (Nitropress), nicardipine (Cardene IV), or other infusion drug as prescribed (for nitroprusside, cover infusion bag to prevent drug breakdown by light); when stable, switch to oral antihypertensive drug.
• Monitor BP every 5 to 15 minutes until the diastolic pressure is below 90 and not less than 75; then monitor BP every 30 minutes to ensure that BP is not lowered too quickly.
• Observe for neurologic or cardiovascular complications, such as seizures; numbness, weakness, or tingling of extremities; dysrhythmias; or chest pain (possible indicators of target organ damage).
Community-Based Care
Teaching for Self-Management
Schmid et al. (2009) found that patient education is essential to help patients become successful in managing their blood pressure (see the Evidence-Based Practice box on p. 785). Provide oral and written information about the indications, dosage, times for administration, side effects, and drug interactions for antihypertensives. Stress that medication must be taken as prescribed; when all of it has been consumed, the prescription must be renewed on a continual basis. Suddenly stopping drugs such as beta blockers can result in angina (chest pain), myocardial infarction (MI), or rebound hypertension. Urge patients to report unpleasant side effects such as excessive fatigue, cough, or sexual dysfunction. In many instances, an alternative drug can be prescribed to minimize certain side effects.
What Do Patients Need to Be Successful Self-Managers of Blood Pressure?
Teach the patient to obtain an ambulatory blood pressure monitoring (ABPM) device for use at home so that the pressure can be checked. Evaluate the patient’s and family’s ability to use this device. If weight reduction is a desired outcome, suggest having a scale in the home for weight monitoring. For patients who do not want to self-monitor, are not able to self-monitor, or have “white-coat” syndrome when they go to their health care provider (causing elevated BP), continuous ABPM may be used. The monitor is worn for 24 hours or longer while patients perform their normal daily activities. Blood pressure is automatically taken every 15 to 30 minutes and recorded for review later. The advantage of this technique is that the health care provider can view the changes in BP readings throughout the 24-hour period to get a picture of a true BP value. Current evidence strongly supports 24-hour ambulatory blood pressure monitoring as a first-line procedure to determine the need for antihypertensive therapy (Verdecchia et al., 2009).
Health Care Resources
A home care nurse may be needed for follow-up to monitor the blood pressure. Evaluate the patient’s or family’s ability to obtain accurate BP measurements, and assess adherence with treatment. The American Heart Association (www.aha.org), the Red Cross, or a local pharmacy may be used for free blood pressure checks if patients cannot buy equipment to monitor their blood pressure. Health fairs are also available in most locations.
Evaluation: Outcomes
• Verbalize understanding of the plan of care, including drug therapy and any necessary lifestyle changes
• Report adverse drug effects, such as coughing, weakness, or dizziness, to the health care provider immediately
• Consistently adhere to the plan of care, including regular follow-up health care provider visits
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree