Chapter 66 Care of Patients with Problems of the Thyroid and Parathyroid Glands
Safe and Effective Care Environment
1. Adjust the environment for the patient with severe hypothyroidism or thyrotoxicosis.
2. Ensure the availability of suction and emergency intubation equipment for anyone who has thyroid or parathyroid surgery.
3. Prevent injury in the patient who has bone density loss or hypocalcemia.
Health Promotion and Maintenance
4. Teach patients taking thyroid hormone inhibitors the correct timing of therapy, side effects, adverse effects, and when to seek medical assistance.
5. Be accepting of patient behavior and changes in appearance.
6. Inform patients and family members that changes in cognition and behavior resulting from thyroid problems are usually temporary.
7. Compare the clinical manifestations of hyperthyroidism with those of hypothyroidism.
8. Interpret clinical changes and laboratory data to determine the effectiveness of interventions for thyroid problems.
9. Coordinate nursing care for the patient during the first 24 hours after thyroid or parathyroid surgery.
10. Identify teaching priorities for the patient taking thyroid hormone replacement therapy.
11. Compare the clinical manifestations of hyperparathyroidism with those of hypoparathyroidism.
http://evolve.elsevier.com/Iggy/
Answer Key for NCLEX Examination Challenges and Decision-Making Challenges
Review Questions for the NCLEX® Examination
Thyroid Disorders
Hyperthyroidism
Pathophysiology
Hyperthyroidism is excessive thyroid hormone secretion from the thyroid gland. The manifestations of hyperthyroidism are called thyrotoxicosis, regardless of the origin of the thyroid hormones (Davies & Larsen, 2008). (For example, a person who takes a large amount of synthetic thyroid hormones can have thyrotoxicosis but does not have hyperthyroidism.) Thyroid hormones increase metabolism in all body organs, and excesses produce many different manifestations. Hyperthyroidism can be temporary or permanent, depending on the cause.
In hyperthyroidism the excessive thyroid hormones stimulate most body systems, causing hypermetabolism and increased sympathetic nervous system activity. Many of the manifestations are caused by the body’s response to the demands of hypermetabolism (Chart 66-1).
Hyperthyroidism
| Skin Manifestations | Neurologic Manifestations |
Metabolic Manifestations Psychological/Emotional Manifestations Reproductive Manifestations Other Manifestations | |
| Pulmonary Manifestations | |
| Cardiovascular Manifestations | |
| Gastrointestinal Manifestations | |
| Musculoskeletal Manifestations | |
Thyroid hormones stimulate the heart, increasing both heart rate and stroke volume. These responses increase cardiac output, systolic blood pressure, and blood flow (Burton, 2011).
Thyroid hormones are produced in response to the stimulation hormones secreted by the hypothalamus and anterior pituitary glands. Thus oversecretion of thyroid hormones changes the secretion of hormones from the hypothalamus and anterior pituitary gland through negative feedback (see Chapter 64). Thyroid hormones also have some influence over sex hormone production in both men and women. Women have menstrual problems and decreased fertility. Both men and women with hyperthyroidism have an increased libido (sexual urge or interest).
Etiology and Genetic Risk
Genetic/Genomic Considerations
Graves’ disease has a strong association with other autoimmune disorders, such as diabetes mellitus, vitiligo, and rheumatoid arthritis. It often occurs in both members of identical twins, with an inheritance pattern of familial clustering or complex, which suggests a polygenic gene-environmental interaction (Nussbaum et al., 2007).
Incidence/Prevalence
Hyperthyroidism is a common endocrine disorder. Graves’ disease can occur at any age but is diagnosed most often in women between 20 and 40 years of age, affecting women about ten times more often than men (Davies & Larsen, 2008). Toxic multinodular goiter usually occurs after the age of 50 and affects women four times more often than men (McCance et al, 2010).
Patient-Centered Collaborative Care
Assessment
History
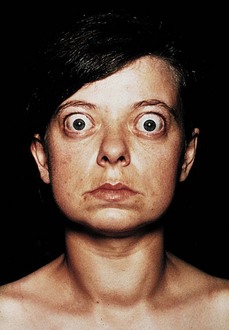
Visual changes may be the earliest problem the patient notices, especially exophthalmos with Graves’ disease (Fig. 66-1). Ask about changes in vision, such as blurring or double vision and tiring of the eyes.
Physical Assessment/Clinical Manifestations
Observe the size and symmetry of the thyroid gland. Palpate the thyroid gland to assess the presence of a mass or general enlargement. In goiter, a generalized thyroid enlargement, the thyroid gland may increase to four times its normal size (Fig. 66-2). Goiters are common in Graves’s disease and are classified by size (Table 66-1). Bruits (turbulence from increased blood flow) may be heard in the neck with a stethoscope. (See Chapter 64 for thyroid palpation and auscultation.)
TABLE 66-1 GOITER CLASSIFICATION
| GOITER GRADE | DESCRIPTION |
|---|---|
| 0 | No palpable or visible goiter. |
| 1 | Mass is not visible with neck in the normal position. Goiter can be palpated and moves up when the patient swallows. |
| 2 | Mass is visible as swelling when the neck is in the normal position. Goiter is easily palpated and is usually asymmetric. |
Laboratory Assessment
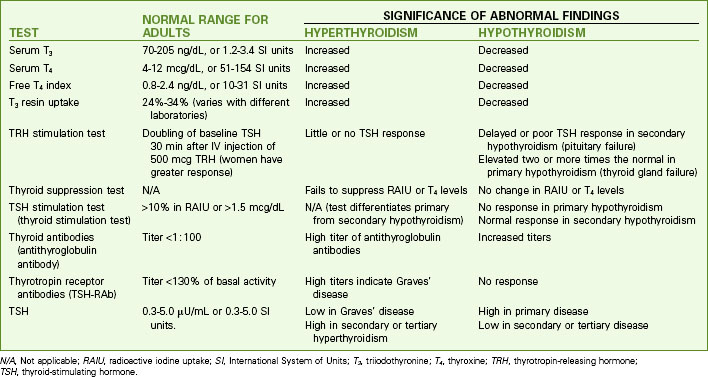
Testing for hyperthyroidism involves measurement of blood values for triiodothyronine (T3), thyroxine (T4), T3 resin uptake (T3RU), and thyroid-stimulating hormone (TSH). Antibodies to TSH (TSH-RAb) are measured to diagnose Graves’ disease. The most common changes in laboratory tests for Graves’ disease and other forms of hyperthyroidism are listed in Chart 66-2.
Other Diagnostic Assessment
Physiological Integrity
Why is a goiter often present in clients who have Graves’ disease?
A. The low circulating levels of thyroid hormones stimulate the feedback system and trigger the anterior pituitary gland to secrete more thyroid-stimulating hormone, which increases the numbers and size of glandular cells in the thyroid gland.
B. The autoantibodies stimulate the inflammatory and immune responses to increase the number of white blood cells circulating in the thyroid gland, which increases tissue size without increasing the number of glandular cells.
C. The excessive autoantibodies bind to the thyroid hormone receptor sites, which increases the number and size of glandular cells in the thyroid gland.
D. The autoantibodies stimulate blood vessel growth and blood storage within the thyroid gland, increasing its overall size.
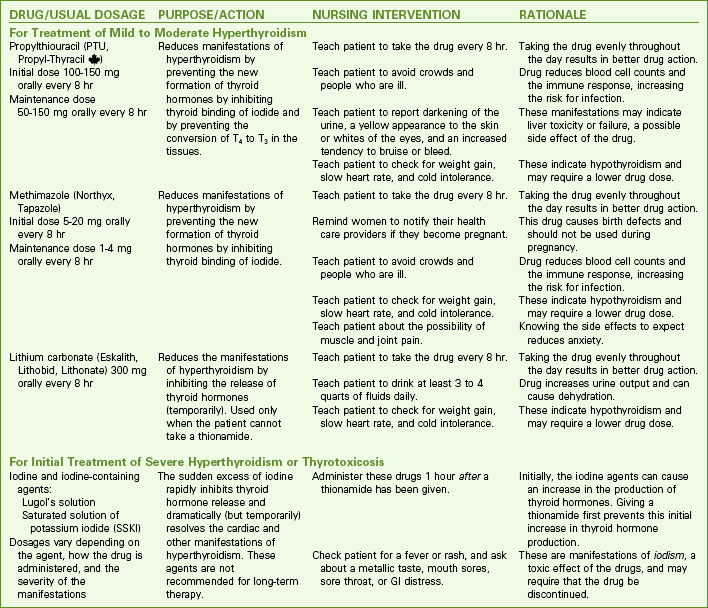
Nonsurgical Management
Drug therapy with antithyroid drugs is the initial treatment of hyperthyroidism. Chart 66-3 lists teaching priorities for the patient receiving drug therapy for hyperthyroidism. The preferred drugs are the thionamides, which include propylthiouracil (PTU) and methimazole (Tapazole). These drugs block thyroid hormone production by preventing iodide binding in the thyroid gland (see Chart 66-3). In addition, PTU also prevents T4 from being converted to the more powerful T3 in the tissues. Methimazole doses are lower than PTU doses. The response to these drugs is delayed because the patient may have large amounts of stored thyroid hormones that continue to be released.
Drug Alert
Both propylthiouracil and methimazole are effective but dangerous drugs. Propylthiouracil now has a black box warning because it is associated with an incidence of serious liver injury and liver failure. Methimazole can cause birth defects. The Food and Drug Administration recommends that unless a patient is pregnant or is allergic to methimazole, propylthiouracil should be avoided. Assess any patient taking propylthiouracil for manifestations of liver problems (e.g., yellowing of the sclera and skin, dark urine, clay-colored stools, elevated liver enzymes) (Aschenbrenner, 2009).
Beta-adrenergic blocking drugs, such as propranolol (Inderal, Detensol ![]() ) may be used as supportive therapy. These drugs relieve diaphoresis, anxiety, tachycardia, and palpitations but do not inhibit thyroid hormone production. See Chapters 36 and 40 for a discussion of the actions and nursing implications of these agents.
) may be used as supportive therapy. These drugs relieve diaphoresis, anxiety, tachycardia, and palpitations but do not inhibit thyroid hormone production. See Chapters 36 and 40 for a discussion of the actions and nursing implications of these agents.
RAI therapy is performed on an outpatient basis. One dose may be sufficient, although some patients need a second or third dose. The radiation dose is low and is usually completely eliminated within a month; however, the source is unsealed, and some radioactivity is present in the patient’s body fluids and stool for a few weeks after therapy (Al-Shakhrah, 2008). Radiation precautions are needed to prevent exposure to family members and other people. Chart 66-4 lists precautions to teach the patient during the first few weeks after receiving 131I.
Patient And Family Education
Preparing For Self-Management: Safety Precautions for the Patient Receiving an Unsealed Radioactive Isotope
• Use a toilet that is not used by others for least 2 weeks after receiving the radioactive iodine.
• Sit to urinate (males and females) to avoid splashing the seat, walls, and floor.
• Flush the toilet three times after each use.
• If urine is spilled on the toilet seat or floor, use paper tissues or towels to clean it up, bag them in sealable plastic bags, and take them to the hospital’s radiation therapy department.
• Men with urinary incontinence should use condom catheters and a drainage bag rather than absorbent gel-filled briefs or pads.
• Women with urinary incontinence should use facial tissue layers in their clothing to catch the urine rather than absorbent gel-filled briefs or pads.
• Using a laxative on the second and third days after receiving the radioactive drug helps you excrete the contaminated stool faster (this also decreases the exposure of your abdominal organs to radiation).
• Wear only machine-washable clothing, and wash these items separate from others in your household.
• After washing your clothing, run the washing machine for a full cycle on empty before it is used to wash the clothing of others.
• Avoid close contact with pregnant women, infants, and young children for the first week after therapy. Remain at least 3 feet (about 1 meter) away from these people, and limit your exposure to them to no more than 1 hour daily.
• Some radioactivity will be in your saliva during the first week after therapy. Precautions to avoid exposing others to this contamination (both household members and trash collectors) include:
Al-Shakhrah, I. (2008). Radioprotection using iodine-131 for thyroid cancer and hyperthyroidism: A review. Clinical Journal of Oncology Nursing, 12(6), 905-912.
Surgical Management
Operative Procedures
A thyroidectomy is performed with the patient under general anesthesia. In the traditional open approach, the patient’s neck is extended and the surgeon makes a “collar” incision just above the clavicle. The surgeon attempts to avoid the parathyroid glands and recurrent laryngeal nerves to reduce the risk for complications and injury. Minimally invasive video-assisted thyroidectomy is being used for some patients (Snissarenko et al., 2009).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree