Chapter 65 Care of Patients with Pituitary and Adrenal Gland Problems
Safe and Effective Care Environment
1. Protect the patient with antidiuretic hormone (ADH) deficiency from dehydration.
2. Use appropriate interventions to prevent injury in the patient who has hypercortisolism.
3. Modify the environment to reduce stimulation for the patient with pheochromocytoma.
Health Promotion and Maintenance
4. Teach patients how to avoid increasing intracranial pressure after pituitary surgery.
5. Identify the teaching priorities for the patient taking hormone replacement therapy for pituitary or adrenal hypofunction.
6. Teach patients how to monitor therapy effectiveness for diabetes insipidus or syndrome of inappropriate ADH (SIADH).
7. Be accepting of patient behavior.
8. Encourage the patient and family to express concerns about a change in endocrine health.
9. Explain all disease management–related procedures to the patient and family.
10. Compare the common clinical manifestations associated with pituitary hypofunction and pituitary hyperfunction.
11. Coordinate nursing care for the patient immediately after a transsphenoidal hypophysectomy.
12. Interpret clinical changes and laboratory data to determine the effectiveness of therapy for diabetes insipidus and for SIADH.
13. Compare the clinical manifestations of hypercortisolism and adrenal insufficiency.
14. Prioritize nursing care for the patient with acute adrenal insufficiency.
15. Coordinate nursing care for the patient with Cushing’s disease or syndrome.
http://evolve.elsevier.com/Iggy/
Answer Key for NCLEX Examination Challenges and Decision-Making Challenges
Review Questions for the NCLEX® Examination
Disorders of the Anterior Pituitary Gland
• Growth hormone (GH; somatotropin)
• Thyrotropin (thyroid-stimulating hormone [TSH])
• Corticotropin (adrenocorticotropic hormone [ACTH])
• Follicle-stimulating hormone (FSH)
• Melanocyte-stimulating hormone (MSH)
Hypopituitarism
Pathophysiology
More commonly, there is a decrease in the secretion of one hormone and a lesser decrease in the secretion of other hormones. Deficiencies of adrenocorticotropic hormone (ACTH) and thyroid-stimulating hormone (TSH) are the most life threatening because they cause a decrease in the secretion of vital hormones from the adrenal and thyroid glands. Adrenal gland hypofunction is discussed on pp. 1381-1384; hypothyroidism is discussed in Chapter 66.
The cause of hypopituitarism varies. Benign or malignant pituitary tumors can compress and destroy pituitary tissue. Pituitary function can be impaired by severe malnutrition or rapid loss of body fat, such as in people with anorexia nervosa (a disorder in which people see themselves as overweight and eat so little that starvation results). Shock or severe hypotension reduces blood flow to the pituitary gland, leading to hypoxia and infarction. Other causes of hypopituitarism include head trauma, brain tumors or infection, radiation or surgery of the head and brain, and acquired immune deficiency syndrome (AIDS) (Melmed & Kleinberg, 2008). Idiopathic hypopituitarism is an isolated hormone deficiency with an unknown cause.
Patient-Centered Collaborative Care
Assessment
Changes in physical appearance and target organ function occur with deficiencies of specific pituitary hormones (Chart 65-1). Gonadotropin (LH and FSH) deficiency results in the loss of or change in secondary sex characteristics in men and women. While assessing the male patient, look for facial and body hair loss. Ask about episodes of impotence and decreased libido (sex drive). Women may report amenorrhea (absence of menstrual periods), dyspareunia (painful intercourse), infertility, and decreased libido. While examining the female patient, check for dry skin, breast atrophy, and a decreased amount or absence of axillary and pubic hair.
Pituitary Hypofunction
| DEFICIENT HORMONE | CLINICAL MANIFESTATIONS |
|---|---|
| Anterior Pituitary Hormones | |
| Growth hormone (GH) | |
| Gonadotropins (luteinizing hormone, follicle-stimulating hormone [FSH]) | |
| Thyroid-stimulating hormone (thyrotropin) (TSH) | |
| Adrenocorticotropic hormone (ACTH) | |
| Posterior Pituitary Hormones | |
Hyperpituitarism
Pathophysiology
Genetic/Genomic Considerations
An uncommon cause of hyperpituitarism is multiple endocrine neoplasia, type 1 (MEN1), in which there is inactivation of the suppressor gene MENIN (Melmed & Kleinberg, 2008). This problem has an autosomal dominant inheritance pattern and is usually expressed as a benign tumor that affects the pituitary, parathyroid glands, and pancreas. In pituitary function, MEN1 leads to excessive production of growth hormone and acromegaly. Ask a patient suspected of having acromegaly whether either parent also has this problem or has had a tumor of the pancreas or parathyroid glands.
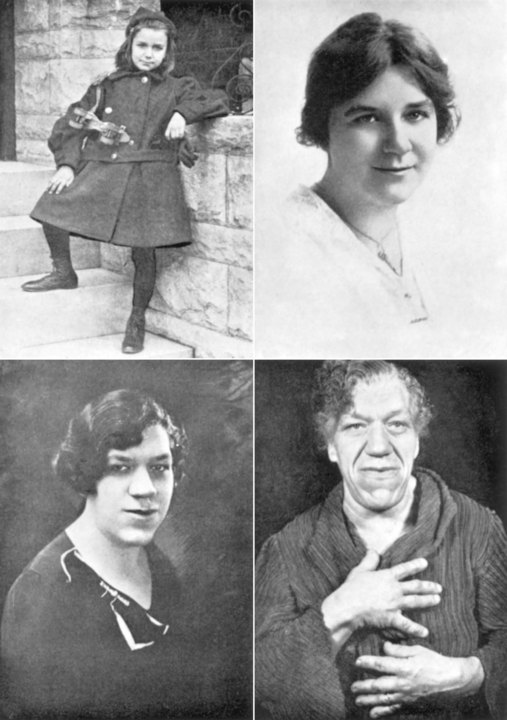
Overproduction of GH in adults results in acromegaly (Fig. 65-1). The onset may be gradual with slow progression, and changes may remain unnoticed for years before diagnosis of the disorder. Early detection and treatment are essential to prevent irreversible changes in the soft tissues, such as those of the face, hands, feet, and skin. Other changes include increased skeletal thickness, hypertrophy of the skin, and enlargement of many organs, such as the liver and heart. Some changes may be reversible after treatment, but skeletal changes are permanent.
Patient-Centered Collaborative Care
Assessment
Changes in appearance and target organ function occur with excesses of specific anterior pituitary hormones (Chart 65-2). Initial manifestations of GH excess are increases in lip and nose sizes, a prominent brow ridge, and increases in head, hand, and foot sizes. The patient with hyperpituitarism often seeks health care because of dramatic changes in appearance. Assess the impact of these changes on self-image and personal relationships.
Anterior Pituitary Hyperfunction
Prolactin (PRL) | Adrenocorticotropic Hormone (ACTH) |
| Cushing’s Disease (Pituitary) | |
| Growth Hormone (GH) | |
| Acromegaly | |
| Thyrotropin (Thyroid-Stimulating Hormone [TSH]) | |
| Gonadotropins (Luteinizing Hormone [LH], Follicle-Stimulating Hormone [FSH]) | |
| Men: | |
| Women: | |
Nonsurgical Management
Drug therapy may be used alone or in combination with surgery and/or radiation. The most common drugs used are dopamine agonists, including bromocriptine mesylate (Parlodel), cabergoline (Dostinex), and pergolide (Permax) (Melmed & Kleinberg, 2008). These drugs stimulate dopamine receptors in the brain and inhibit the release of GH and PRL. In most cases, small tumors decrease until the pituitary gland is of normal size. Large pituitary tumors usually decrease to some extent. In patients with acromegaly, bromocriptine reduces GH levels and decreases tumor size, especially when GH levels remain high after surgery or before the full effect of radiation therapy has occurred.
Drug Alert
Surgical Management
Preoperative Care
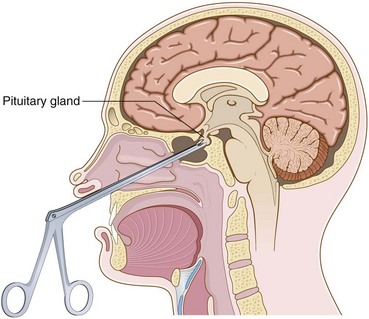
Depending on tumor size and other patient factors, a minimally invasive endoscopic transnasal approach may be used instead of the more traditional transsphenoidal approach (Fig. 65-2). Although both procedures are less invasive than a craniotomy, the endoscopic approach uses smaller diameter instruments and results in less damage to nasal structures (Graham et al., 2009). Both procedures are performed with the patient in a semi-sitting position. For the transsphenoidal approach, the surgeon makes an incision just above the upper lip and reaches the pituitary gland through the sphenoid sinus. After the gland is removed, a muscle graft is taken, often from the thigh, to support the area and prevent leakage of cerebrospinal fluid (CSF). Nasal packing is inserted after the incision is closed, and a mustache dressing is applied. If the tumor cannot be reached by either the endoscopic transnasal approach or the transsphenoidal approach, a craniotomy may be indicated (see Chapter 47).
If the entire pituitary gland has been removed, replacement of thyroid hormones and glucocorticoids is lifelong. Best practices for care after surgery are listed in Chart 65-3.
Chart 65-3 Best Practice For Patient Safety & Quality Care
The Patient After Hypophysectomy
• Monitor the patient’s neurologic status hourly for the first 24 hours and then every 4 hours.
• Monitor fluid balance, especially for output greater than intake, because transient diabetes insipidus can occur.
• Encourage the patient to maintain pulmonary hygiene through deep-breathing exercises.
• Instruct the patient to not cough, blow the nose, or sneeze.
• Instruct the patient to use dental floss and oral mouth rinses, because brushing the teeth is not permitted until the incision heals sufficiently.
• Instruct the patient to avoid bending at the waist for any reason, because this position increases intracranial pressure.
• Monitor the nasal drip pad for the type and amount of drainage. The presence of the halo sign may indicate a CSF leak.
• Monitor bowel movements to prevent constipation and subsequent “straining.”
• Teach the patient self-administration of the prescribed hormones.
After surgery, the patient needs daily self-management regimens and frequent checkups. He or she may need strategies to reduce stress. The home care nurse performs a focused assessment during any home visit to a patient who has undergone a hypophysectomy (Chart 65-4). Review drug regimens and manifestations of infection and cerebral edema with the family.
Chart 65-4 Home Care Assessment
The Patient Who Has Undergone Transsphenoidal or Endoscopic Nasal Hypophysectomy for Hyperpituitarism
Safe and Effective Care Environment