Chapter 54 Care of Patients with Musculoskeletal Trauma
Safe and Effective Care Environment
1. Explain the importance of collaborating with the health care team when providing care for patients with fractures and amputations.
2. Apply principles of infection control when caring for a patient with a compound fracture.
Health Promotion and Maintenance
3. Identify community resources about amputations for patients and their families.
4. Recognize the importance of teaching the public about ways to prevent fractures and other musculoskeletal injuries.
5. Plan discharge teaching for patients with fractures or amputations.
6. Plan care that meets the special needs of older adults with hip fractures, including interventions to increase mobility.
7. Describe how to assess the patient’s and family’s reaction to changes in body image resulting from amputation.
8. Explain how to assist patients in coping with loss of a body part.
9. Compare and contrast common types of fractures.
10. Describe the usual healing process for bone.
11. Assess patients with musculoskeletal trauma to prioritize interventions for their care.
12. Explain the typical clinical manifestations that are seen in patients with fractures.
13. Delineate nursing care needed to maintain casts for patients with fractures.
14. Delineate nursing care needed to maintain traction and external fixation for patients with fractures.
15. Plan pain management for patients with musculoskeletal trauma.
16. Identify the risk for complications from fractures, and take measures to help prevent them.
17. Describe how to perform focused musculoskeletal and neurovascular assessment for patients with musculoskeletal trauma.
18. Develop a postoperative plan of care, including health teaching, for a patient after fracture repair.
19. Describe emergency care for people who have a traumatic amputation.
20. Plan postoperative care, including health teaching, after an elective amputation.
21. Identify common causes of amputations.
22. Identify appropriate complementary and alternative therapies for patients with phantom limb pain.
23. Describe the patient-centered collaborative care needed to manage complex regional pain syndrome.
24. Plan care for patients with common types of sports-related injuries.
http://evolve.elsevier.com/Iggy/
Answer Key to NCLEX Examination Challenges and Decision-Making Challenges
Review Questions for the NCLEX® Examination
Fractures
Pathophysiology
Classification of Fractures
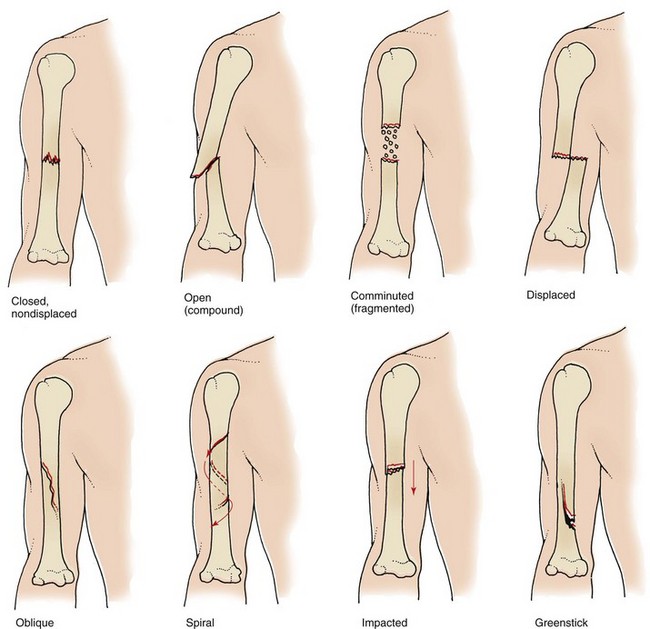
A fracture is classified by the extent of the break:
• Complete fracture. The break is across the entire width of the bone in such a way that the bone is divided into two distinct sections.
• Incomplete fracture. The fracture does not divide the bone into two portions because the break is through only part of the bone.
Fig. 54-1 shows common types of fractures. In addition to being identified by type, fractures are described by their cause. A pathologic (spontaneous) fracture occurs after minimal trauma to a bone that has been weakened by disease. For example, a patient with bone cancer or osteoporosis can easily have a pathologic fracture. A fatigue (stress) fracture results from excessive strain and stress on the bone. This problem is commonly seen in recreational and professional athletes. Compression fractures are produced by a loading force applied to the long axis of cancellous bone. They commonly occur in the vertebrae of older patients with osteoporosis and are extremely painful.
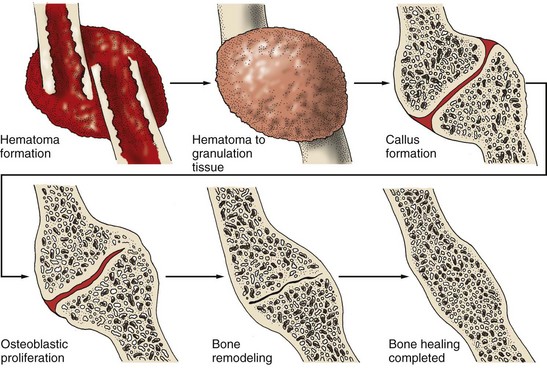
Stages of Bone Healing
When a bone is fractured, the body immediately begins the healing process to repair the injury and restore the body’s equilibrium. Fractures heal in five stages that are a continuous process and not single stages. In stage one, within 24 to 72 hours after the injury, a hematoma forms at the site of the fracture because bone is extremely vascular. Stage two occurs in 3 days to 2 weeks when granulation tissue begins to invade the hematoma. This then prompts the formation of fibrocartilage, providing the foundation for bone healing. Stage three of bone healing occurs as a result of vascular and cellular proliferation. The fracture site is surrounded by new vascular tissue known as a callus (within 3 to 6 weeks). Callus formation is the beginning of a nonbony union. As healing continues in stage four, the callus is gradually resorbed and transformed into bone. This stage usually takes 3 to 8 weeks. During the fifth and final stage of healing, consolidation and remodeling of bone continue to meet mechanical demands. This process may start as early as 4 to 6 weeks after fracture and can continue for up to 1 year, depending on the severity of the injury and the age and health of the patient. Fig. 54-2 summarizes the stages of bone healing.
Considerations for Older Adults
Bone healing is often affected by the aging process. Bone formation and strength rely on adequate nutrition. Calcium, phosphorus, vitamin D, and protein are necessary for the production of new bone (see Chapter 53). For women, the loss of estrogen after menopause decreases the body’s ability to form new bone tissue. Chronic diseases can also affect the rate at which bone heals. For instance, peripheral vascular diseases, such as arteriosclerosis, reduce arterial circulation to bone. Thus the bone receives less oxygen and fewer nutrients, both of which are needed for repair.
Complications of Fractures
Acute Compartment Syndrome
The pathophysiologic changes of increased compartment pressure are sometimes referred to as the ischemia-edema cycle. Capillaries within the muscle dilate, which raises capillary pressure. Capillaries then become more permeable because of the release of histamine by the ischemic muscle tissue. As a result, plasma proteins leak into the interstitial fluid space and edema occurs. Edema increases pressure on nerve endings and causes pain. Blood flow to the area is reduced, and further ischemia results. Sensory deficits or paresthesia generally appears before changes in vascular or motor signs. The color of the tissue pales, and pulses begin to weaken but rarely disappear. The affected area is usually palpably tense, and pain occurs with passive motion of the extremity. If the condition is not treated, cyanosis, tingling, numbness, paresis, necrosis, and severe pain can occur. Chart 54-1 summarizes the sequence of pathophysiologic events in compartment syndrome and the associated clinical assessment findings.
Compartment Syndrome
| Physiologic Change | Clinical Findings |
| Increased compartment pressure | No change |
| Increased capillary permeability | Edema |
| Release of histamine | Increased edema |
| Increased blood flow to area | Pulses present Pink tissue |
| Pressure on nerve endings | Pain |
| Increased tissue pressure | Referred pain to compartment |
| Decreased tissue perfusion | Increased edema |
| Decreased oxygen to tissues | Pallor |
| Increased production of lactic acid | Unequal pulses Flexed posture |
| Anaerobic metabolism | Cyanosis |
| Vasodilation | Increased edema |
| Increased blood flow | Tense muscle swelling |
| Increased tissue pressure | Tingling Numbness |
| Increased edema | Paresthesia |
| Muscle ischemia | Severe pain unrelieved by drugs |
| Tissue necrosis | Paresis/paralysis |
Crush Syndrome
Specific causes of CS include:
• Natural disasters, such as earthquakes
• Work-related injuries, such as being trapped under heavy equipment such as a car
• Drug or alcohol overdose, when one or more limbs may be compressed by body weight for a prolonged time
• Older adults who fall, are unable to get up, and lie for a prolonged time
Regardless of the cause, CS is indicated by:
• Hypovolemia (decreased circulating blood volume)
• Hyperkalemia (increased serum potassium)
• Rhabdomyolysis (myoglobulin release from skeletal muscle into the bloodstream)
• Acute tubular necrosis (ATN) resulting from hypovolemia and rhabdomyolysis
Hypovolemic Shock
Bone is very vascular. Therefore there is a risk for bleeding with bone injury. In addition, trauma can cut nearby arteries and cause hemorrhage, resulting in rapidly developing hypovolemic shock. (The pathophysiology of hypovolemic shock is described in Chapter 39.)
Fat Embolism Syndrome
Abnormal laboratory findings include:
• Increased erythrocyte sedimentation rate (ESR)
• Decreased serum calcium levels
• Decreased red blood cell and platelet counts
These changes in blood values are poorly understood, but they aid in diagnosis of the condition.
FES can result in respiratory failure or death, often from pulmonary edema. When the lungs are affected, the complication may be misdiagnosed as a pulmonary embolism from a blood clot (Chart 54-2).
Pulmonary Emboli: Fat Embolism Versus Blood Clot Embolism
| Fat Embolism | Blood Clot Embolism |
|---|---|
| Definition | |
| Obstruction of the pulmonary vascular bed by fat globules | Obstruction of the pulmonary artery by a blood clot or clots |
| Origin | |
| 95% from fractures of the long bones; occurs usually within 48 hr of injury | 85% from deep vein thrombosis in the legs or pelvis; can occur anytime |
| Assessment Findings | |
| Same as for fat embolism, except no petechiae | |
| Treatment | |
SaO2, Arterial oxygen saturation; SCD, sequential compression device.
Venous Thromboembolism
• Surgical procedure longer than 30 minutes
• Oral contraceptives or hormones
• History of VTE complications
The pathophysiology and management of VTE is described in Chapter 38.
Etiology and Genetic Risk
The primary cause of a fracture is trauma from a motor vehicle crash or fall, especially in older adults. The trauma may be a direct blow to the bone or an indirect force from muscle contractions or pulling forces on the bone. Sports, vigorous exercise, and malnutrition are contributing factors. Bone diseases, such as osteoporosis, increase the risk for a fracture in older adults (see Chapter 53). Genetic factors that increase risk for fracture are discussed with these specific health problems throughout this text.
Health Promotion and Maintenance
• Osteoporosis screening and education
• Home safety assessment and modification, if needed
• Dangers of drinking and driving
• Drug safety (prescribed, over-the-counter, and illicit)
• Helmet use when riding bicycles, motorcycles, all-terrain vehicles (ATVs), and skateboards
These educational interventions are discussed throughout this book and in other texts. Fall prevention is discussed in detail in Chapter 3 as part of care for older adults.
Patient-Centered Collaborative Care
Assessment
Physical Assessment/Clinical Manifestations
Action Alert
Swelling at the fracture site is rapid and can result in marked neurovascular compromise. Gently perform a thorough neurovascular assessment, and compare extremities. Assess skin color and temperature, sensation, mobility, pain, and pulses distal to the fracture site. If the fracture involves an extremity and the patient is not in severe pain, check the nails for capillary refill by applying pressure to the nail and observing for the speed of blood return. If nails are brittle or thick, assess the skin next to the nail. Checking for capillary refill is not as reliable as other indicators of perfusion. Chart 54-3 describes the procedure for a neurovascular assessment, which evaluates circulation, movement, and sensation (CMS function).
Chart 54-3 Best Practice for Patient Safety & Quality Care
Assessment of Neurovascular Status in Patients with Musculoskeletal Injury
| Assessment method | Normal Findings |
|---|---|
| Skin Color | |
| Inspect the area distal to the injury. | No change in pigmentation compared with other parts of the body. |
| Skin Temperature | |
| Palpate the area distal to the injury (the dorsum of the hands is most sensitive to temperature). | The skin is warm. |
| Movement | |
| Ask the patient to move the affected area or the area distal to the injury (active motion). | The patient can move without discomfort. |
| Move the area distal to the injury (passive motion). | No difference in comfort compared with active movement. |
| Sensation | |
| Ask the patient if numbness or tingling is present (paresthesia). | No numbness or tingling. |
| Palpate with a paper clip (especially the web space between the first and second toes or the web space between the thumb and forefinger). | No difference in sensation in the affected and unaffected extremities. (Loss of sensation in these areas indicates peroneal nerve or median nerve damage.) |
| Pulses | |
| Palpate the pulses distal to the injury. | Pulses are strong and easily palpated; no difference in the affected and unaffected extremities. |
| Capillary Refill (Least Reliable) | |
| Press the nail beds distal to the injury until blanching occurs (or the skin near the nail if nails are thick and brittle). | Blood returns (return to usual color) within 3 sec (5 sec for older patients). |
| Pain | |
| Ask the patient about the location, nature, and frequency of the pain. | Pain is usually localized and is often described as stabbing or throbbing. (Pain out of proportion to the injury and unrelieved by analgesics might indicate compartment syndrome.) |
Patient-Centered Care; Evidence-Based Practice
1. What are your priority assessments for the patient when coming into the ED? What sources of evidence would you seek to answer this clinical question?
2. The patient has a dislocated ankle (distal tibia and fibula) and reports that she is still in pain even though the EMT gave her IV fentanyl. How will you respond to this patient, and what action will you take?
3. The patient’s daughter comes to the ED and asks you if her mother’s history of osteopenia may have caused the fracture. How will you answer her?
4. What factors may have contributed to this patient’s “slip and fall?”
Analysis
The most common problems for patients with fractures are:
1. Acute Pain related to one or more fractures, soft-tissue damage, muscle spasm, and edema
2. Potential for neurovascular compromise related to tissue edema and/or bleeding
3. Potential for infection related to a wound caused by an open fracture
4. Impaired Physical Mobility related to acute or chronic pain
Planning and Implementation
Managing Acute Pain
Interventions
For any patient who experiences trauma in the community, first call 911 and assess for airway, breathing, and circulation (ABCs, or primary survey). Then provide lifesaving care if needed before being concerned about the fracture (Chart 54-4). If CPR is needed, ensure circulation first, followed by airway and breathing (see Chapter 36).
Chart 54-4 Best Practice for Patient Safety & Quality Care
Emergency Care of the Patient with an Extremity Fracture
1. Assess the patient’s airway, breathing, and circulation, and perform a quick head-to-toe assessment.
2. Remove the patient’s clothing (cut if necessary) to inspect the affected area while supporting the area above and below the injury. Do not remove shoes because this can cause increased trauma.
3. Remove jewelry on the affected extremity in case of swelling.
4. Apply direct pressure on the area if there is bleeding and pressure over the proximal artery nearest the fracture.
5. Keep the patient warm and in a supine position.
6. Check the neurovascular status of the area distal to the fracture, including temperature, color, sensation, movement, and capillary refill. Compare affected and unaffected limbs.
7. Immobilize the extremity by splinting; include joints above and below the fracture site. Recheck circulation after splinting.
8. Cover any open areas with a dressing (preferably sterile).
For each modality, the primary nursing concern is assessment and prevention of neurovascular dysfunction or compromise. Assess the patient’s neurovascular status every hour for the first 24 hours and every 1 to 4 hours thereafter, depending on the injury (see Chart 54-3). The patient usually reports discomfort that is unrelieved by analgesics if the bandage, splint, or cast is too tight. Elevate the fractured extremity higher than the heart, and apply ice for the first 24 to 48 hours as needed to reduce edema.
Closed Reduction and Immobilization
For certain areas of the body, such as the scapula (shoulder) and clavicle (collarbone), an elastic bandage or commercial immobilizer may be used to keep the bone in place during healing. Because upper extremity bones do not bear weight, splints may be sufficient to keep bone fragments in place for a closed fracture. Fig. 54-3 shows a wrist splint for fracture immobilization. Thermoplastic, a durable, flexible material for splinting, allows custom fitting to the patient’s body part. Splints for lower extremities are also custom-fitted using flexible materials and held in place with elastic bandages (e.g., ace wrap).
Synthetic materials for casts are much more common and include fiberglass and polyester-cotton knit (Fig. 54-4). These materials are lighter than plaster and require minimal drying time. Fiberglass casts are dry in 10 to 15 minutes and can bear weight 30 minutes after application. Polyester-cotton knit casts take 7 minutes to dry and can withstand weight bearing in about 20 minutes. Some health care providers may use synthetic casts for upper extremities and plaster-of-Paris casts for lower extremities because plaster casts can bear more weight for a longer time. However, newer synthetic materials are stronger than earlier ones. Synthetic casts can be bivalved as needed.
Casts can be generally divided into four main groups: arm casts, leg casts, cast braces, and body or spica casts. Table 54-1 describes specific casts that are used for various parts of the body.
TABLE 54-1 TYPES OF CASTS USED FOR MUSCULOSKELETAL TRAUMA
| TYPE AND CHARACTERISTICS OF CAST | USE |
|---|---|
| Upper Extremity Casts | |
| Short-arm cast (SAC) (extends from below the elbow to and including part of the hand) | Stable fractures of the wrist (metacarpals, carpals, or distal radius) |
| Long-arm cast (LAC) (includes the upper arm to and including part of the hand) | Unstable fractures of the wrist, distal humerus, radius, or ulna |
| Hanging-arm cast (same as LAC but heavier, with added loop at the mid-forearm) | Fractures of the humerus that cannot be aligned by LAC (light traction is possible while the patient is in bed or by an attached strap that extends around the neck) |
| Thumb spica (gauntlet) cast (similar to SAC with the thumb casted in abduction) | Fractures of the thumb |
| Shoulder spica cast (the shoulder is casted in abduction with the elbow flexed) | Unstable fractures of the shoulder girdle or humerus; dislocations of the shoulder |
| Lower Extremity Casts | |
| Short-leg cast (SLC) (from below the knee to the base of the toes) | Fractures of the ankle, metatarsals, or foot |
| Long-leg cast (LLC) (from the mid-upper thigh to the base of the toes) | Unstable fractures of the tibia, fibula, or ankle |
| Walking cast (a walking device on the bottom of SLC or LLC) | Same as for SLC or LLC |
| Leg cylinder (similar to SLC, but the ankle and foot are not casted) | Stable fractures of the tibia, fibula, or knee |
| Long-leg cylinder (similar to LLC, but the ankle and foot are not casted) | Stable fractures of the distal femur, proximal tibia, or knee |
| Cast Braces (or Brace Casts) (Not As Common) | |
| Patellar weight-bearing cast (similar to SLC or leg cylinder) | Mid-shaft or distal shaft fractures of the femur |
| External polycentric knee hinge cast (a hinge connects the lower and upper leg and allows 90 degrees of knee flexion) | Same as for the patellar weight-bearing cast |
| Body Casts (Not As Common) | |
Hip spica (extends from below the nipple line down the affected leg [single], down the leg and half of the unaffected leg [ ], or down both legs [double]) ], or down both legs [double]) | Dislocation of the hip; pelvic or hip injuries |
| Risser cast (the body jacket extends from the shoulders to beyond the iliac crests and hips, with a large opening over the anterior chest) | Scoliosis; thoracic spinal fractures |
| Halo cast (the body jacket contains a halo brace) | Fractures of the cervical spine |
Action Alert
Action Alert
Mechanical traction can be either:
• Continuous, as in fracture treatment
• Intermittent, for relief of muscle spasm in other types of musculoskeletal/neurologic trauma, such as cervical nerve root compression
Traction may also be classified as running traction or balanced suspension. In running traction, the pulling force is in one direction and the patient’s body acts as countertraction. Moving the body or bed position can alter the countertraction force. Balanced suspension provides the countertraction so that the pulling force of the traction is not altered when the bed or patient is moved. This allows for increased movement and facilitates care (Table 54-2).
TABLE 54-2 TYPES OF TRACTION USED FOR MUSCULOSKELETAL TRAUMA
| Type and Characteristics of Traction | Use |
|---|---|
| Upper Extremity Traction | |
| Sidearm skin or skeletal traction (the forearm is flexed and extended 90 degrees from the upper part of the body) | Fractures of the humerus with or without involvement of the shoulder and clavicle |
| Overhead or 90-90 traction, skin or skeletal (the elbow is flexed and the arm is at a right angle to the body over the upper chest) | Same as above (depends on the physician’s preference) |
| Plaster traction (pins inserted through the bone are fixed in the cast) | Fractures of the wrist |
| Lower Extremity Traction | |
| Buck’s extension traction (skin) (the affected leg is in extension) | Fractures of the hip or femur preoperatively Prevention of hip flexion contractures Hip dislocation |
| Russell’s traction (similar to Buck’s traction, but a sling under the knee suspends the leg) | Fractures of the hip or distal end of the femur |
| Balanced skin or skeletal traction (the limb is usually elevated in a Thomas splint with Pearson’s attachment, or a Böhler-Braun splint is used) | Fractures of the femur or pelvis (acetabulum) |
| Spinal Column and Pelvic Traction | |
| Cervical halter (a strap under the chin) | Cervical muscle spasms, strain/sprain, or arthritis |
| Cervical skeletal (e.g., halo brace, Crutchfield tongs) | Cervical fractures of the spine; muscle spasms |
| Pelvic belt (a strap around the hips at the iliac crests is attached to weights at the foot of the bed) | Pain, strain, sprain, or muscle spasms in the lower back |
| Pelvic sling (a wide strap around the hips is attached to an overhead bar to keep the pelvis off the bed) | Pelvic fractures; other pelvic injuries |
The two most common types of traction are skin and skeletal traction. Skin traction involves the use of a Velcro boot (Buck’s traction) (Fig. 54-5), belt, or halter, which is usually secured around the affected leg. The primary purpose of skin traction is to decrease painful muscle spasms that accompany hip fractures. The weight is used as a pulling force and is limited to 5 to 10 pounds (2.3 to 4.5 kg) to prevent injury to the skin.

FIG. 54-5 Skin traction with a hook-and-loop fastener (Velcro) boot, commonly used for hip fractures.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree