Donna D. Ignatavicius
Care of Patients with Infection
Learning Outcomes
Safe and Effective Care Environment
Health Promotion and Maintenance
Psychosocial Integrity
Physiological Integrity
6 Identify patients most at risk for infection, including older adults.
7 Provide information to patient and family about drug therapy for infections.
8 Identify common clinical manifestations of infectious diseases.
9 Interpret laboratory test findings related to infections and infectious diseases.
10 Evaluate nursing interventions for management of the patient with an infection.
11 Explain why multidrug-resistant organisms are increasing.
12 Identify common emerging diseases and their basic clinical management.

http://evolve.elsevier.com/Iggy/
Answer Key for NCLEX Examination Challenges and Decision-Making Challenges
Audio Glossary
Concept Map Creator
Key Points
Review Questions for the NCLEX® Examination
The human body has many protective systems that promote homeostasis. Physiologic mechanisms are the structural and functional defenses that protect people from stressors such as infection. When these mechanisms fail to work properly or are overcome with microbes, infection can result.
Infections and infectious diseases have been the major cause of millions of deaths worldwide for centuries. Today, threats of bioterrorism have been added to the concerns about multidrug-resistant and emerging infections. Global travel and migration have increased exposure to a wider variety of infectious agents than in the past. For example, severe acute respiratory syndrome (SARS), monkeypox, and Avian influenza (“bird flu”) have appeared for the first time in the United States during the past decade. However, humans have not gotten any of these diseases yet.
Advancing technology and invasive procedures also introduce microorganisms into the body, often resulting in infection, even though in other environments these microorganisms are harmless. This chapter provides an overview of infection and general principles for prevention and management. Specific infections and their management are described elsewhere in this text.
Overview of the Infectious Process
A pathogen is any microorganism (also called an agent) capable of producing disease. Infections can be communicable (transmitted from person to person [e.g., influenza]) or not communicable (e.g., peritonitis). Microorganisms with differing levels of pathogenicity (ability to cause disease) surround everyone. Virulence is a term for pathogenicity. However, virulence is related more to the frequency with which a pathogen causes disease (degree of communicability) and its ability to invade and damage a host. It can also indicate the severity of the disease.
Many microorganisms live in or on the human host without causing disease. Some microbes are beneficial. Each body location harbors its own characteristic bacteria, or normal flora. Normal flora often functions to compete with and prevent infection from unfamiliar agents attempting to invade a body site. In some instances, microorganisms that are often pathogenic may be present in the tissues of the host and yet not cause symptomatic disease because of normal flora; this process is called colonization.
In the United States, the Centers for Disease Control and Prevention (CDC) collects information about the occurrence and nature of infections and infectious diseases. It then recommends guidelines to health care agencies for infection control and prevention. Certain diseases, such as tuberculosis, must be reported to health departments and the CDC. The infection control practitioner (ICP) for each health care agency is responsible for tracking infections (surveillance) and ensuring compliance with federal and local requirements.
Transmission of Infectious Agents
Transmission of infection in health care requires three factors:
Reservoirs (sources of infectious agents) are numerous. Animate reservoirs include people, animals, and insects. Inanimate reservoirs include soil, water, other environmental sources, and medical equipment (e.g., IV solutions, urine collection devices). The host’s body can be a reservoir; pathogens colonize skin and body substances (e.g., feces, sputum, saliva, wound drainage). A person with an active infection or an asymptomatic carrier (one who harbors an infectious agent without active disease) is a reservoir. Examples of community reservoirs include sewage, stagnant or contaminated water, and improperly handled foods.
Bacteria like Neisseria meningitidis can exist in the respiratory tract while causing no illness. If the bacteria invade the bloodstream or cerebrospinal fluid, they become extremely pathogenic. Another example is Enterococcus, which lives as normal flora in the GI system, where it is nonpathogenic and assists in the digestive process. If it enters the bloodstream, Enterococcus can cause disease.
Continued multiplication of a pathogen is sometimes accompanied by toxin production. Toxins are protein molecules released by bacteria to affect host cells at a distant site. Exotoxins are produced and released by certain bacteria into the surrounding environment. Botulism, tetanus, diphtheria, and Escherichia coli 0157:H7–related systemic diseases are attributed to exotoxins. Endotoxins are produced in the cell walls of certain bacteria and released only with cell lysis. For example, typhoid and meningococcal diseases are caused by endotoxins.
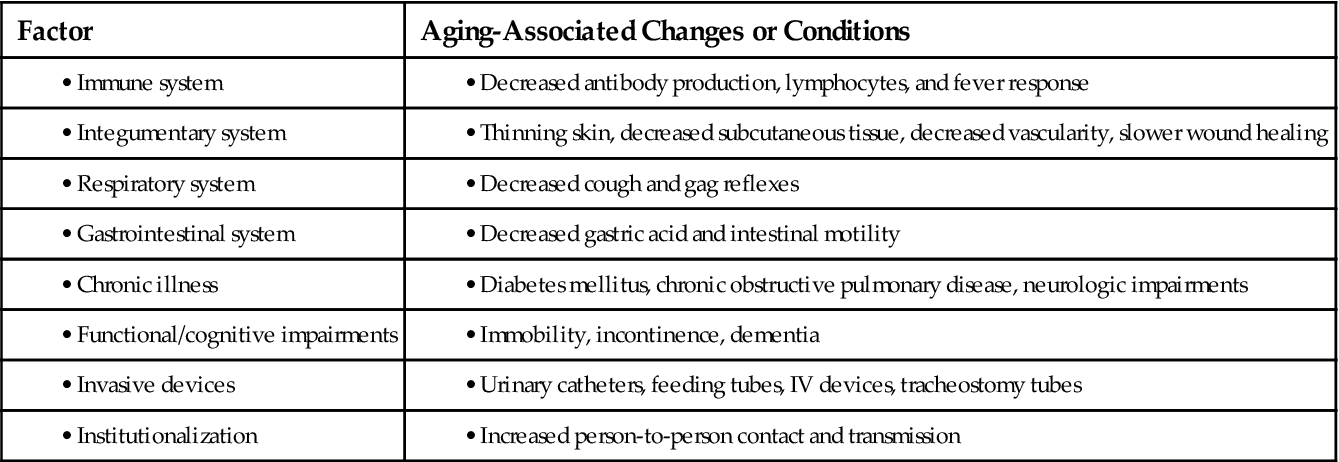
Host factors influence the development of infection (Table 25-1). Host defenses provide the body with an efficient system for protection against pathogens. Breakdown of these defense mechanisms may increase the susceptibility (risk) of the host for infection.
TABLE 25-1
HOST FACTORS THAT INFLUENCE THE DEVELOPMENT OF INFECTION
| HOST FACTOR | INCREASED RISK FOR INFECTION |
| Natural immunity | Congenital or acquired immune deficiencies |
| Normal flora | Alteration of normal flora by antibiotic therapy |
| Age | Infants and older adults |
| Hormonal factors | Diabetes mellitus, corticosteroid therapy, and adrenal insufficiency |
| Phagocytosis | Defective phagocytic function, circulatory disturbances, and neutropenia |
| Skin/mucous membranes/normal excretory secretions | Break in skin or mucous membrane integrity; interference with flow of urine, tears, or saliva; interference with cough reflex or ciliary action; changes in gastric secretions |
| Nutrition | Malnutrition or dehydration |
| Environmental factors | Tobacco and alcohol consumption and inhalation of toxic chemicals |
| Medical interventions | Invasive therapy, chemotherapy, radiation therapy, and steroid therapy; surgery |
The patient’s immune status plays a large role in determining risk for infection. Congenital abnormalities, as well as acquired health problems (e.g., renal failure, steroid dependence, cancer, acquired immune deficiency syndrome [AIDS]), can result in numerous immunologic deficiencies. Depression of the immune system may make the host more susceptible to infection or cripple the ability to combat organisms that have gained entry.
Immunity is resistance to infection; it is usually associated with the presence of antibodies or cells that act on specific microorganisms. Passive immunity is of short duration (days or months) and either natural by transplacental transfer from the mother or artificial by injection of antibodies (e.g., immunoglobulin). Active immunity lasts for years and is natural by infection or artificial by stimulation of the body’s immune defenses (e.g., vaccination). Chapter 19 discusses the immune system and immunity in detail.
Environmental factors can also influence patients’ immune status and thus their susceptibility to or ability to fight infection. Examples include alcohol consumption, nicotine use, inhalation of bone marrow–suppressing toxic chemicals, and certain vitamin deficiencies. Malnutrition, especially protein-calorie malnutrition, places patients at increased risk for infection. Diseases such as diabetes mellitus also predispose a patient to infection. Older adults have decreased immune systems, as well as other physiologic changes that make them very susceptible to infection (Chart 25-1).
Medical and surgical interventions may impair normal immune response. Steroid therapy, chemotherapy, and anti-rejection drugs increase the risk for infection. Medical devices (e.g., intravascular or urinary catheters, endotracheal tubes, synthetic implants) may also interfere with normal host defense mechanisms. Surgery, trauma, radiation therapy, and burns result in nonintact skin. The body’s skin is one of the best barriers or defenses against infection. When this barrier is broken, infection often results.
Microorganisms may enter the body in a variety of ways, including the respiratory tract, GI tract, genitourinary tract, skin and mucous membranes, and bloodstream.
Pathogens may enter the body through the respiratory tract. Microbes in droplets are sprayed into the air when people with infected oral or nasal tissues talk, cough, or sneeze. A susceptible host then inhales droplets, and pathogens localize in the lungs or are distributed via the lymphatic system or bloodstream to other areas of the body. Microorganisms that enter the body by the respiratory tract and produce distant infection include influenza virus, Mycobacterium tuberculosis, and Streptococcus pneumoniae.
Other pathogens enter the body through the GI tract. Some stay there and produce disease (e.g., Shigella causing self-limited disease). Others invade the GI tract to produce local and distant infection (e.g., Salmonella enteritidis). Some produce limited GI symptoms, causing systemic infection (e.g., Salmonella typhi) or profound involvement of other organs (e.g., hepatitis A virus). Millions of foodborne illness cases occur each year in the United States. This type of illness results in many hospitalizations and deaths.
Microorganisms also enter through the genitourinary tract. Urinary tract infection (UTI) is one of the most common health care–associated infections (HAIs). More than half of patients in adult intensive care units (ICUs) have urinary catheters in place. Indwelling urinary catheters are a primary cause of UTIs. The use of invasive catheters has decreased in long-term care settings because older adults are very susceptible to infections.
Although intact skin is the best barrier to prevent most infections, some pathogens such as Treponema pallidum can enter the body through intact skin or mucous membranes. Most enter through breaks in these normally effective surface barriers. Sometimes a medical procedure creates a break in cutaneous or mucocutaneous barriers, as in catheter-acquired bacteremia (bacteria in the bloodstream) and surgical-site infections (SSIs). Fragile skin of older patients and of those receiving prolonged steroid therapy increases infection risk.
Microorganisms can gain direct access to the bloodstream, especially when invasive devices or tubes are used. The incidence of bloodstream infections (BSIs) continues to increase in hospitals throughout the United States. Central venous catheters (CVCs) are a primary cause of these infections (see Chapter 15 for more discussion of CVC-related BSIs). In the community setting, biting insects can inject organisms into the bloodstream, causing infection (e.g., Lyme disease, West Nile viral encephalitis).
For infection to be transmitted from an infected source to a susceptible host, a transport mechanism is required. Microorganisms are transmitted by several routes:
Contact transmission is the usual mode of transmission of most infections. Many infections are spread by direct or indirect contact. With direct contact, the source and host have physical contact. Microorganisms are transferred directly from skin to skin or from mucous membrane to mucous membrane. Often called person-to-person transmission, direct contact is best illustrated by the spread of the “common cold.”
Indirect contact transmission involves the transfer of microorganisms from a source to a host by passive transfer from a contaminated object. Contaminated articles or hands may be sources of infection. For example, patient-care devices like glucometers and electronic thermometers may transmit pathogens if they are contaminated with blood or body fluids. Uniforms, laboratory coats, and isolation gowns used as part of personal protective equipment may be contaminated as well.
Indirect transmission may involve contact with infected secretions or droplets. Droplets are produced when a person talks or sneezes; the droplets travel short distances. Susceptible hosts may acquire infection by contact with droplets deposited on the nasal, oral, or conjunctival membranes. Therefore the CDC recommends that staff stay at least 3 feet (1 m) away from a patient with droplet infection (Siegel et al., 2007). An example of droplet-spread infection is influenza. Unlike airborne droplet nuclei, discussed later, droplets do not stay suspended in the air.
Airborne transmission occurs when small airborne particles containing pathogens leave the infected source and enter a susceptible host. These pathogens can be suspended in the air for a prolonged time. The particles carrying pathogens are usually contained in droplet nuclei or dust; they are usually propelled from the respiratory tract by coughing or sneezing. A susceptible person then inhales the particles directly into the respiratory tract. For example, tuberculosis is spread via airborne transmission.
Preventing the spread of microbes that are transmitted by the airborne route requires the use of special air handling and ventilation systems in an airborne infection isolation room (AIIR). M. tuberculosis and the varicella-zoster virus (chickenpox) are examples of airborne agents that require one of these systems. In addition to the AIIR, respiratory protection using certified N95 or higher level respirator masks is recommended for health care personnel entering the patient’s room (Siegel et al., 2007). The N95 rating means that at least 95% of the inhaled air is filtered.
Other sources of infectious agents include the environment, such as contaminated food, water, or vectors. Vectors are insects that carry pathogens between two or more hosts, such as the deer tick that causes Lyme disease.
The portal of exit completes the chain of infection. Exit of the microbe from the host often occurs through the portal of entry. An organism, such as M. tuberculosis, enters the respiratory tract and then exits the same tract as the infected host coughs. Some organisms can exit from the infected host by several routes. For example, varicella-zoster virus can spread through direct contact with infective fluid in vesicles and by airborne transmission.
Physiologic Defenses for Infection
Strong and intact host defenses can prevent microbes from entering the body or can destroy a pathogen that has entered. Impaired host defenses may be unable to defend against microbial invasion, allowing entry of organisms that can destroy cells and cause infection. Common defense mechanisms include:
Intact skin forms the first and most important physical barrier to the entry of microorganisms. In addition to providing a mechanical barrier, the skin’s slightly acidic pH (resulting from breakdown of lipids into fatty acids), together with normal skin flora, creates an unfriendly environment for many bacteria.
Mucous membranes’ mucociliary action provides some mechanical protection against pathogenic invasion. More important, however, mucous membranes are bathed in secretions that inactivate many microorganisms. Lysozymes, which dissolve the cell walls of some bacteria, are present in large quantities in many body secretions, particularly in tears and nasal mucus.
Other body systems provide natural barriers to infection. For instance, the healthy respiratory tract clears about 90% of all inhaled material by upper airway filtration, humidification, mucociliary transport, and coughing. Peristaltic action mechanically empties the GI tract of pathogenic organisms. Stomach acid, intestinal secretions, pancreatic enzymes, and bile, together with the competition from normal bowel flora, provide an environment that protects the GI tract from invasion by harmful organisms. In the genitourinary tract, the flushing action of urine eliminates pathogenic organisms. The low pH of urine also maintains a sterile environment, although some microorganisms, such as E. coli, thrive in an acid medium.
Phagocytosis occurs when a foreign substance evades the first-line mechanical barriers and enters the body. Various leukocyte types function differently in the immune reaction, but neutrophils bear primary responsibility for phagocytosis. This process of engulfing, ingesting, killing, and disposing of an invading organism is an essential mechanism in host defense. Phagocytic dysfunction dramatically increases a patient’s risk for infection.
Inflammation is another important nonspecific defense mechanism for preventing the spread of infection. It occurs when tissue becomes damaged. Damaged cells release enzymes, and polymorphonuclear (PMN) leukocytes (neutrophils) are attracted to the infected site from the bloodstream. One important substance, histamine, increases the permeability of the capillaries in inflamed tissues, thus allowing fluid, proteins, and white blood cells to enter an inflamed area. Other enzymes activate fibrinogen, which causes leaked fluid to clot and prevents its flow away from the damaged site into unaffected tissue, essentially “walling off” the inflamed tissue. The process of phagocytosis disposes of the invading microorganism and often dead tissue. If inflammation is caused by infection, the end products of inflammation form pus, which is then absorbed or exits the body through a break in the skin. Chapter 19 discusses the process of inflammation in more detail.
Specific defense responses to specific microorganisms are provided by the antibody- and cell-mediated immune systems. The antibody-mediated immune system produces antibodies directed against certain pathogens. These antibodies inactivate or destroy invading microorganisms as well as protect against future infection from that microorganism. Resistance to other microorganisms is mediated by the action of specifically sensitized T-lymphocytes and is called cell-mediated immunity. The components of the immune system work both independently and together to protect against infection. Chapter 19 describes the function of the immune system in detail.
Health Promotion and Maintenance
Infection Control in Inpatient Health Care Agencies
Infections occur most often in high-risk patients, such as older adults and those who have inadequate immune systems (immunocompromised). Implement interventions to prevent infection and detect signs and symptoms as early as possible. Chart 25-2 summarizes nursing interventions for infection prevention and control.
Infection acquired in the inpatient health care setting (not present or incubating at admission) is termed a health care–associated infection (HAI). When occurring in a hospital setting, they are sometimes referred to as hospital-acquired infections, but the former term is more accurate. HAIs can be endogenous (from a patient’s flora) or exogenous (from outside the patient, often from the hands of health care workers, tubes, or implants). Therefore use of the less popular term nosocomial infection does not imply that an infection was caused by health care (or poor health care delivery) but only that it occurred while receiving health care. HAIs, including surgical-site infections (SSIs), occur in 1 in 20 inpatients yearly, causing increased health care costs and many deaths (see discussion of SSIs in Chapter 18). These infections tend to occur most often because health care workers do not follow basic infection control principles, especially aseptic technique and injection practices (Siegel et al., 2007).
Infection control within a health care facility is designed to reduce the risk for HAIs and thus reduce morbidity and mortality, as recommended in The Joint Commission’s National Patient Safety Goals (NPSGs). This expected outcome is consistent with the desire for health care facilities to create a culture of safety within their environments (see Chapter 1). Infection control and prevention is a collaborative effort and includes:
• Facility- and department-specific infection control policies and procedures
• Community and interdisciplinary collaboration
• Product evaluation with an emphasis on quality and cost savings
• Bioengineering for designing health care facilities that help control the spread of infections
The infection control program of a hospital is usually coordinated and implemented by a health care professional certified in infection control (CIC) who has clinical and administrative experience. The Centers for Disease Control and Prevention (CDC) recommends one person with CIC credentials for every 100 occupied acute care beds. Long-term care facilities may not have a practitioner who is dedicated to infection control. However, every facility must designate a health care professional to be responsible for coordinating and implementing an infection prevention and control program.
Long-term care facilities are unique in that they have a large group of older adults who are together in one setting for weeks to years. Nursing homes, in particular, are required to provide a homelike environment in which residents can move and interact freely. Therefore infection control in these settings can be challenging. As a result, many infectious outbreaks have occurred, such as pneumonia, Clostridium difficile, and multidrug-resistant organisms (discussed in the Multidrug-Resistant Organism Infections and Colonizations section on pp. 440-443).
Infection Control in Community-Based Settings
Ambulatory and home health care are the fastest growing segments of the health care system. Infection remains the most common cause of death for dialysis patients. Data on infections in other ambulatory settings are lacking because the CDC has only recently recommended surveillance systems and prevention guidelines. Little information is available about acquired infections in home health settings because data are not systematically collected, surveillance programs are not established, and best practices for infection prevention and control do not exist.
Methods of Infection Control
All health care workers who come in contact with patients or care areas are involved in some aspect of the infection control program of the agency. According to the CDC, infections can be prevented or controlled in at least five major ways:
Health care workers’ hands are the primary way in which infection is transmitted from patient to patient or staff to patient. Hand hygiene refers to both handwashing and alcohol-based hand rubs (ABHRs) (“hand sanitizers”). There is a lack of rigorous evidence linking which specific hand hygiene recommendations best prevent health care–associated infections (HAIs) (Backman et al., 2008).
In 2002, the CDC released a document entitled “CDC Hand Hygiene Recommendations.” These recommendations are summarized in Chart 25-3. Handwashing is still an important part of hand hygiene, but it is recognized that in some health care settings, sinks may not be readily available. Despite years of education, health care workers often find it difficult to leave the patient care setting to wash their hands and do not perform hand hygiene on a consistent basis.
Effective handwashing includes wetting, soaping, lathering, applying friction under running water for at least 15 seconds, rinsing, and adequate drying. Friction is essential to remove skin oils and to disperse transient bacteria and soil from hand surfaces. Performing adequate handwashing takes time that health care workers (HCWs) may not feel they have. Handwashing can also cause dry skin, and therefore hand moisturizers are essential to maintain good hand health and hygiene.
Alcohol-based hand rubs (ABHRs) allow care providers to spend less time seeking out sinks and more time delivering care. However, these hand rubs have their limitations.
The CDC recommends using antiseptic solutions such as chlorhexidine, povidone-iodine, or parachlorometaxylenol (PCMX) for handwashing in caring for patients who are at high risk for infection (e.g., those who are immunocompromised). The use of these solutions is also recommended after caring for patients who are infected with multidrug-resistant or other virulent organisms.
The CDC guidelines (Centers for Disease Control and Prevention [CDC], 2002) also address the issue of artificial fingernails, which have been linked to a number of outbreaks due to poor fingernail health and hygiene. The guidelines recommend that artificial fingernails and extenders not be worn while caring for patients at high risk for infections, such as those in ICUs or operating suites. Most health care agencies have banned artificial nails for all health care workers providing direct patient care and require that natural nails be short and without nail polish.
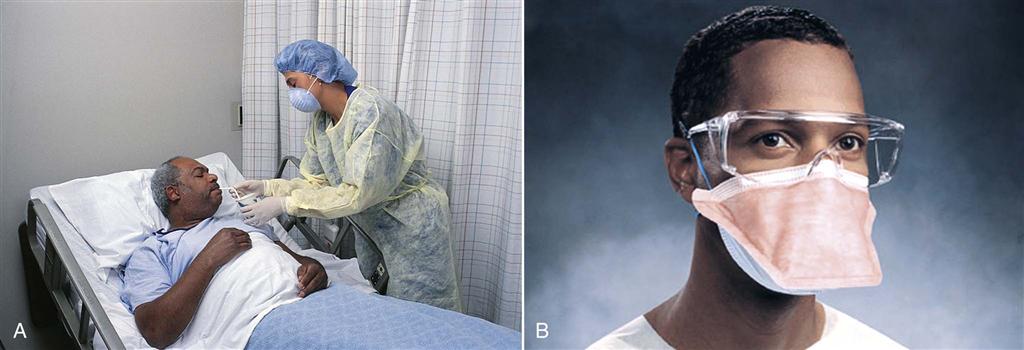
Personal protective equipment (PPE) refers to the use of gloves, isolation gowns, face protection (masks, goggles, face shields), and respirators with N95 or higher filtration (Fig. 25-1).
Most health care settings in the United States and Canada have switched from latex to non-latex gloves. The U.S. National Institute for Occupational Safety and Health (NIOSH) issued a public warning about potential allergic reactions to those exposed to latex in gloves and other medical products. Reactions include rashes, nasal or eye symptoms, asthma, and (rarely) shock. People with latex allergy usually have an allergy to foods such as bananas, kiwis, and avocados. Health care workers (HCWs) have not been as strict with wearing gloves as they should because of poor fit or skin dryness, irritation, and dermatitis. One possible solution to dry skin is the use of aloe vera–coated gloves or moisturizers such as Eucerin or AmLactin products.
Adequate staffing of nurses is an essential method for preventing infection (Stone et al., 2008). In addition to a ratio of one infection control practitioner (ICP) to 100 occupied acute care beds, nurse staffing is critical. The CDC recommends that two methods to ensure adequate infection control (IC) be implemented (Siegel et al., 2007). First, an infection control nurse liaison should be designated on every unit of an inpatient facility. This nurse is responsible for implementing new IC policies, increasing staff IC compliance through education, and collaborating with the facility’s ICP to monitor for infections. Second, bedside nurse staffing should consists of full-time nurses assigned regularly to the unit rather than float, pool, or agency nurses. Studies have found that infection rates increase when float, pool, or agency nurses are substituted for full-time, regular staff (Siegel et al., 2007).
Sterilization and disinfection have helped invasive procedures become much more common and safe. Sterilization means destroying all living organisms and bacterial spores. All items that invade human tissue where bacteria are not commonly found should be sterilized. Disinfection does not kill spores and only ensures a reduction in the level of disease-causing organisms. High-level disinfection is adequate when an item is going inside the body where the patient has resident bacteria or normal flora (e.g., GI and respiratory tracts). As with sterilization, no high-level disinfection can occur without first cleaning the item. This can be especially difficult with items that have narrow lumens in which organic debris can become trapped and is not easily visible. For example, endoscopes have been especially challenging to clean and have been linked to a number of infectious outbreaks.
Patient placement has been used as a way to reduce the spread of infection. Some studies have suggested that private patient rooms help decrease infections. However, the CDC has not mandated that all patients, even those with infections, have a private room. The CDC does recommend that private rooms always be used for patients on Airborne Precautions and those in a protective environment (PE). A PE is architecturally designed and structured to prevent infection from occurring in patients who are at extremely high risk, such as those having stem cell therapy. The CDC also prefers private rooms for patients who are on Contact and Droplet Precautions (Siegel et al., 2007). Many hospitals are increasing their number of private rooms, and some are becoming totally private-room facilities. Large health care systems often have biomedical engineers to assist in designing the best environment to reduce the spread of infection, including ventilation systems and physical layout.
Cohorting is another method of patient placement. Cohorting is the practice of grouping patients who are colonized or infected with the same pathogen. This method has been used the most with patients who have an outbreak of a multidrug-resistant organism like methicillin-resistant Staphylococcus aureus (MRSA). It is particularly effective in long-term care settings.
Infection control principles for patient transport include limiting movement to other areas of the facility, using appropriate barriers like covering infected wounds, and notifying other departments or agencies who are receiving the patient about the necessary precautions (Siegel et al., 2007). Complete and accurate hand-off communication between agencies is also very important to prevent the spread of infection, according to The Joint Commission’s NPSGs.