M. Linda Workman
Care of Patients with Immune Function Excess
Hypersensitivity (Allergy) and Autoimmunity
Learning Outcomes
Safe and Effective Care Environment
Health Promotion and Maintenance
Physiological Integrity
6 Describe allergy testing techniques.
8 Prioritize care for the patient experiencing anaphylaxis.
9 Explain the rationale for types of drug therapy for autoimmune disorders.
10 Identify the manifestations of hypersensitivity reactions.
11 Prioritize care for the patient experiencing anaphylaxis.

http://evolve.elsevier.com/Iggy/
Animation: Allergy
Answer Key for NCLEX Examination Challenges and Decision-Making Challenges
Audio Clip: High- and Low-Pitched Crackles
Audio Clip: High- and Low-Pitched Wheezes
Audio Glossary
Concept Map Creator
Key Points
Review Questions for the NCLEX® Examination
Most of the time, the inflammatory and immune responses are helpful for protection against infection and cancer development. However, when inflammation or immune responses are prolonged or excessive or occur at an inappropriate time, normal tissues are damaged. These responses are “overreactions” to invaders and foreign antigens and are known as hypersensitivity or allergic responses. When these responses fail to recognize and protect self cells, normal body tissues are attacked and harmed. This type of reaction is known as an autoimmune response. Hypersensitivity and autoimmune responses can severely damage cells, tissues, and organs (Abbas et al., 2010).
Hypersensitivities/Allergies
Hypersensitivity or allergy is an increased or excessive response to the presence of an antigen (foreign protein or allergen) to which the patient usually has been previously exposed. These responses cause problems that range from uncomfortable (e.g., itchy, watery eyes or sneezing) to life threatening (e.g., allergic asthma, anaphylaxis, bronchoconstriction, or circulatory collapse). The terms hypersensitivity and allergy are used interchangeably. Hypersensitivity reactions are classified into five basic types, determined by differences in timing, pathophysiology, and clinical manifestations (Table 22-1). Each type may occur alone or along with one or more other types (McCance et al., 2010).
TABLE 22-1
MECHANISMS AND EXAMPLES OF TYPES OF HYPERSENSITIVITIES
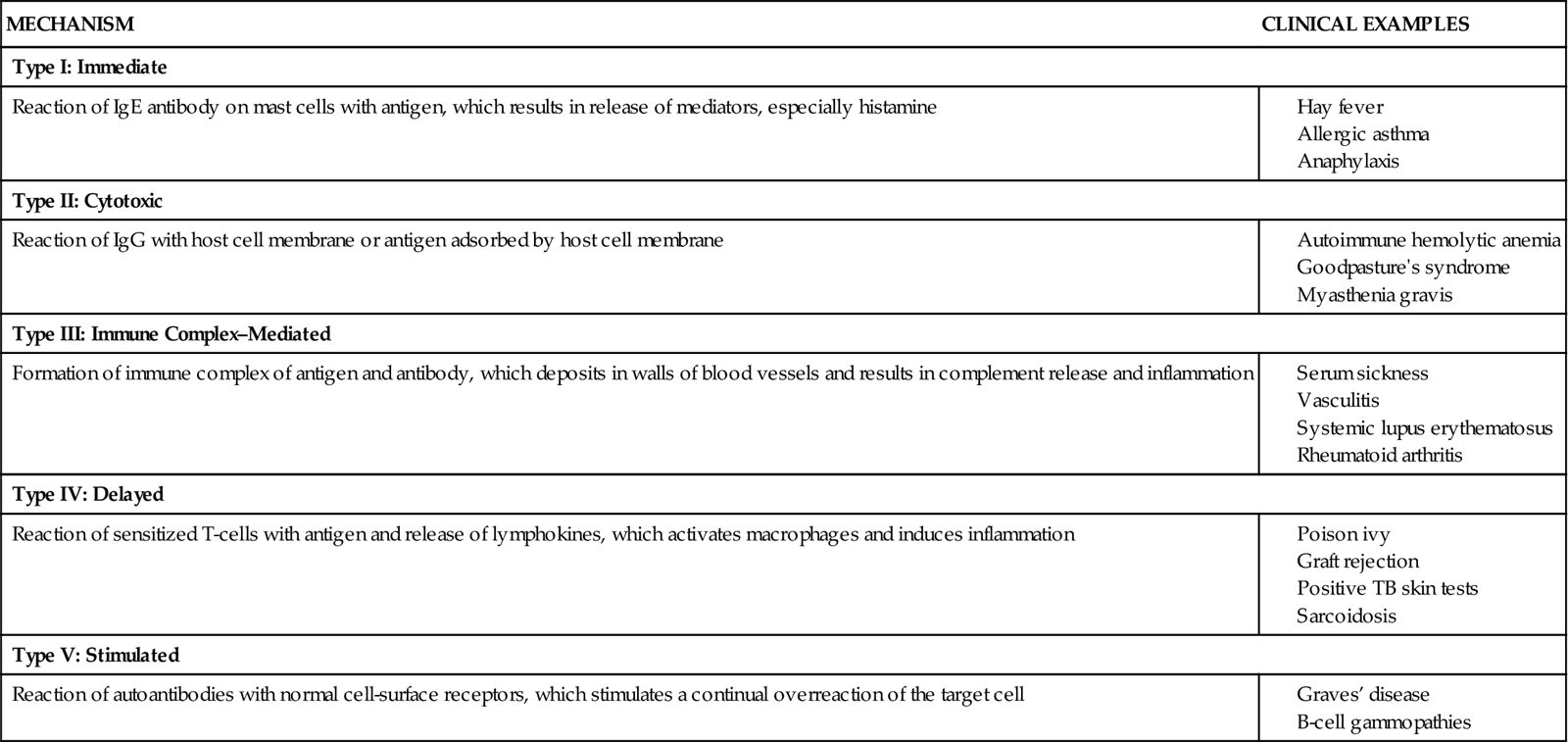
IgE, Immunoglobulin E; IgG, immunoglobulin G; TB, tuberculosis.
Type I: Rapid Hypersensitivity Reactions
Type I, or rapid, hypersensitivity, also called atopic allergy, is the most common type of hypersensitivity. This type results from the increased production of the immunoglobulin E (IgE) antibody class. Acute inflammation occurs when IgE responds to an antigen, such as pollen, and causes the release of histamine and other vasoactive amines from basophils, eosinophils, and mast cells. Examples of type I reactions include anaphylaxis and allergic asthma (discussed in Chapter 32); atopic allergies such as hay fever and allergic rhinitis; and allergies to specific allergens such as latex, bee venom, peanuts, iodine, shellfish, drugs, and thousands of other environmental antigens. Allergens can be contacted in these ways:
• Inhaled (plant pollens, fungal spores, animal dander, house dust, grass, ragweed)
• Ingested (foods, food additives, drugs)
• Injected (bee venom, drugs, biologic substances such as contrast dyes)
Some reactions occur just in the areas exposed to the antigen, such as the mucous membranes of the nose and eyes, causing symptoms of rhinorrhea, sneezing, and itchy, red, watery eyes. Other reactions may involve all blood vessels and bronchiolar smooth muscle causing widespread blood vessel dilation, decreased cardiac output, and bronchoconstriction. This condition is known as anaphylaxis. When symptoms of anaphylaxis occur in a patient who has not been previously exposed to the allergen, the condition is known as an anaphylactoid reaction (Watson, 2010).
Allergic Rhinitis
Pathophysiology
Allergic rhinitis, also called hay fever, is triggered by reactions to airborne allergens, especially plant pollens, molds, dust, animal dander, wool, food, and air pollutants. Some acute episodes are “seasonal,” tending to recur at the same time each year. They often coincide with the timing of large environmental exposure and last only a few weeks. Chronic rhinitis, or perennial rhinitis, tends to occur intermittently (with no predictable seasonal pattern) or continuously when a person is exposed to certain allergens. In “nonallergic rhinitis,” the same manifestations are present although no allergic cause is identified and the immune system does not appear to be involved.
On first exposure to an allergen (an antigen that provokes allergic sensitization), the person responds by making antigen-specific IgE. This antigen-specific IgE binds to the surface of basophils and mast cells (see Fig. 19-9 on p. 311 in Chapter 19). These cells have many granules containing vasoactive amines (including histamine) that are released when stimulated. Once the antigen-specific IgE is formed, the person is sensitized to that allergen.
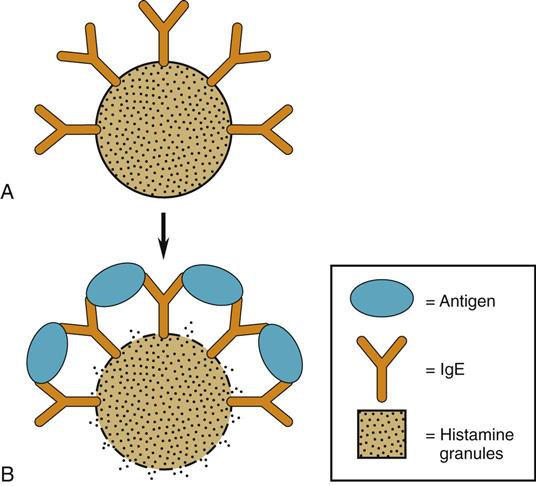
In a type I allergic reaction, the already sensitized person is re-exposed to the provoking allergen. The resulting response has a primary phase and a secondary phase. In the primary phase, the allergen binds to two adjacent IgE molecules on the surface of a basophil or mast cell, which breaks or distorts the cell membrane. These changes cause the cell membrane to open and release the vasoactive amines within the granules into the tissue fluids (Fig. 22-1).
The most common vasoactive amine is histamine, a short-acting biochemical. Histamine causes capillary leak, nasal and conjunctival mucus secretion, and itching (pruritus), often occurring with erythema (redness). These symptoms last for about 10 minutes after histamine is first released. When the allergen is continuously present, mast cells continuously release histamine and other proteins, prolonging the response.
The secondary phase results from the release of other proteins. These other proteins draw more white blood cells to the area and stimulate a more general inflammatory reaction through actions of leukotriene and prostaglandins (other mediators of inflammation; see Chapter 19). This reaction occurs in addition to the allergic reaction stimulated in the primary phase. The resulting inflammation increases the clinical manifestations and is probably responsible for continuing the response.
The tendency to produce IgE in response to antigen exposure is based on genetic inheritance, but no single gene has been found to be responsible. Although allergic tendencies are inherited, specific allergies are not inherited (Nussbaum et al., 2007). For example, a mother who has an allergy to penicillin but not to peanuts may have a child with an allergy to peanuts but not to penicillin. About 50% of patients with allergic rhinitis have one parent with type I allergies. Atopic allergies, including allergic rhinitis, affect about 10% of the population in North America (McCance et al., 2010).
Patient-Centered Collaborative Care
Assessment
History
An accurate and detailed history helps identify possible allergic rhinitis. Ask the patient to describe the onset and duration of problems in relation to possible allergen exposure. Ask about work, school, and home environments and about possible exposures through hobbies, leisure time, or sports activities. Because a tendency toward type I allergic responses can be inherited, ask about the presence of allergies among close relatives.
Physical Assessment/Clinical Manifestations
The patient with allergic rhinitis usually has rhinorrhea (a “runny” nose), a “stuffy” nose, and itchy, watery eyes. He or she may breathe through the mouth, and the voice has a nasal sound. Drainage from the nose is usually clear or white. The nasal mucosa appears swollen and pink. The patient may have a headache or feel pressure over the frontal and maxillary sinuses. Placing a penlight directly on the skin over the sinuses and observing for a glow (transillumination) usually shows reduced glow when rhinitis is present. If nasal secretions drip posteriorly, he or she may have a dry, scratchy throat and pharyngitis. The patient often feels as though he or she has a cold that has lasted longer than a week. Fever is rare unless an infection occurs with the rhinitis.
Laboratory Assessment
A complete blood count (CBC) and differential indicate the presence of an allergic response by an increase in eosinophils. A patient with severe seasonal allergic rhinitis may have an eosinophil count as high as 12% (normal being 1% to 2%). Some patients have an increased total white blood cell (WBC) count, but the percentage of neutrophils remains normal (55% to 70%). If an acute infection occurs with allergic rhinitis, both the total WBC count and the number of neutrophils increase.
Other laboratory tests that indicate the presence of an allergic reaction include serum immunoglobulin E (IgE) levels and the radioallergosorbent test (RAST). A normal level of IgE for adults is about 39 IU/mL (or <100 IU/mL). This level can increase greatly with allergies. The usual IgE test does not indicate the specific allergen—only the tendency to have allergic responses. The radioimmunosorbent test (RIST) shows the blood level of IgE directed against a specific antigen and thus can determine specific allergies. The expense of this study limits its use in allergy testing.
Allergy Testing
Skin testing can show which specific allergens are the cause of most type I reactions. Skin testing can be performed as scratch testing and intradermal testing. Patch testing is often reserved for contact dermatitis and other manifestations of type IV hypersensitivities.
A scratch or prick test can show an immediate hypersensitivity reaction to an allergen. Scratch tests are used in routine allergy testing to determine the cause of allergic rhinitis, asthma, urticaria (hives), or any other type I reactions. Allergens introduced through a scratch or prick cause a localized reaction (wheal) when the test result is positive. Results are usually determined after 15 to 20 minutes.
Patient Preparation.
For best results, systemic glucocorticoids and antihistamines are discontinued for up to 4 weeks before the test to avoid suppressing an allergic response during the test. Nasal sprays to reduce mucous membrane swelling are permitted, except for sprays that contain an antihistamine. Some allergists recommend that aspirin and other NSAIDs also be withheld before allergy testing.
Procedure.
The best site for scratch testing is the inside of the forearm or on the back. Other sites are used if a rash or skin problem is present on the arms or back. Gently clean the skin with soap and water, and remove surface oils with alcohol.
Small drops of sera containing different known allergens are placed on the skin. The skin is scratched or pricked through the drop with a bifurcated skin testing needle. Control drops are also applied to determine how a person reacts to substances that do not normally stimulate a reaction (negative control) and to substances that normally should stimulate a reaction (positive control). Normal saline drops are negative controls, and histamine drops are positive controls. The allergen-tested areas are examined for the presence and size of positive reactions. These areas are then compared with the control areas. Areas showing erythema and wheal formation are considered positive for that antigen. Degree of sensitivity is estimated by the size of the response.
Serious reactions in response to scratch testing are rare. Ensure that emergency equipment, including manual resuscitation bag, oxygen, suction equipment, IV infusion set, and drugs for anaphylaxis (epinephrine and diphenhydramine), is available during a scratch test.
Follow-up Care.
After testing is completed, wash the solution from the skin. Topical steroids and oral antihistamines may be given to reduce itching and increase patient comfort. If an antihistamine that causes sedation is given, another person must drive the patient home.
Repeat open application testing (ROAT) is a form of self-administered patch testing that can help determine which hygiene or beauty products are responsible for a person’s contact dermatitis (Gelpi & Jacob, 2008). (Hygiene, laundry, and beauty products are the most frequent causes of contact dermatitis.) Often, just one application of a suspected allergen does not produce a positive result. With ROAT, the person showers and then draws a 3-cm circle on the inner aspect of the upper arm. The person then selects one product as a suspected allergen and applies it to the circled area. The product is applied to the area twice daily for 7 days. The patient is instructed to protect the area from sunlight and to check it daily for a reaction. A positive reaction may include the presence of increased redness, small bumps, water blisters, or skin scaling. Once a product is identified as an allergen, the patient avoids using it.
Intradermal testing is reserved for substances that are strongly suspected of causing allergy but did not test positive with scratch testing. Intradermal testing increases the risk for an adverse reaction, including anaphylaxis, but it is usually a safe procedure. Ensure that emergency equipment is in the room with the patient. Small amounts of testing sera (0.1 mL) are injected intradermally on the patient’s upper arm and the area is observed for erythema and wheal formation. The degree of allergy is estimated by the size of the response. Patient preparation and follow-up care are the same as for scratch testing.
Oral food challenges are used for patients who have allergic rhinitis when the allergen is eaten and does not come into direct contact with the nasal mucosa. This type of testing is used to identify specific allergens if skin testing is not conclusive and if keeping a food diary has failed to determine the offending food items. The test requires the patient to eliminate suspected foods for 7 to 14 days before testing. After this time, the patient is directed to eat specific suspected food for at least 1 day and to monitor for manifestations of allergy. When many food allergies are present, the patient may have to eat only one food type per day of testing. Oral food challenges are not performed with foods that are known to cause anaphylactic reactions in the patient.
Interventions
Common interventions for allergy management include avoidance therapy, drug therapy, complementary and alternative therapies, and desensitization therapy. Many patients use a combination of these types of therapy for management of allergic rhinitis and other manifestations of type I allergy.
Avoidance Therapy
Avoidance therapy can be successful when specific allergens have been identified. Urge the patient to avoid direct or close contact with these agents. Some allergens, such as certain foods or drugs, may be easy to avoid. Other substances, such as pollen, mold, or dust mites, may require environmental changes.
Teach patients that many airborne allergens can be reduced by air-conditioning and air-cleaning units. In addition, removing cloth drapes, upholstered furniture, and carpeting reduces airborne allergens. Covering mattresses and pillows with plastic or an ultrafine mesh cover also reduces exposure to dust mites and mold, as does laundering bed linens weekly in hot water and detergent.
Pet-induced allergies pose special challenges. Sometimes simple interventions, such as keeping pets out of the bedroom and thorough cleaning of the room to remove animal hair and dander, may reduce symptoms. Frequent bathing of the pet or keeping the pet outdoors can decrease allergen exposure. Depending on the severity of the allergy and how well other methods provide relief, pets with fur, feathers, or dander may need to be removed from the household.
Drug Therapy
Drug therapy for symptom relief may be tried when avoidance therapy is impractical. It can be effective in reducing the allergic response and making the patient more comfortable. Drug therapy involves the use of steroidal and nonsteroidal agents (to reduce inflammation), vasoconstrictors, antihistamines, mast cell stabilizers, and drugs that inhibit the release or action of leukotrienes. Some drugs reduce the response, and other drugs prevent the response.
Decongestants are available as systemic oral drugs or nasal sprays. These drugs do not clear the allergen or prevent the release of mediators such as histamine. They have actions similar to adrenergic drugs and work by causing vasoconstriction in the inflamed tissue, thereby reducing the edema. Decongestants often contain ephedrine, phenylephrine, or pseudoephedrine. Secretions are reduced when vasoconstricting drugs are combined with an anticholinergic drug, such as scopolamine or atropine. Many combination decongestants are available by prescription and as over-the-counter cold and allergy drugs. Side effects include dry mouth, increased blood pressure, and sleep difficulties.
Antihistamines block histamine from binding to the receptor. This action prevents vasodilation and capillary leak. Many antihistamines also decrease secretions. Some antihistamines, such as diphenhydramine (Benadryl, Allerdryl ![]() ) and chlorpheniramine (Allergy, Aller-Chlor, Chlor-Trimeton), often induce sedation. Newer antihistamines, such as desloratadine (Clarinex), cetirizine (Zyrtec), and fexofenadine (Allegra), are less sedating. Not every patient responds to each drug in the same way.
) and chlorpheniramine (Allergy, Aller-Chlor, Chlor-Trimeton), often induce sedation. Newer antihistamines, such as desloratadine (Clarinex), cetirizine (Zyrtec), and fexofenadine (Allegra), are less sedating. Not every patient responds to each drug in the same way.
Corticosteroids decrease inflammatory and immune responses in many ways, one of which is by preventing the synthesis of mediators. Corticosteroid nasal sprays can prevent the symptoms of rhinitis. Systemic corticosteroids can produce severe side effects. These drugs are avoided for rhinitis and are used only on a short-term basis for other problems associated with type I reactions.
Mast cell stabilizing drugs include nasal sprays, such as cromolyn sodium (Nasalcrom), that prevent mast cell membranes from opening when an allergen binds to IgE. Thus these drugs prevent the symptoms of allergic rhinitis but are not useful during an acute episode.
Leukotriene modifiers may be used to treat allergic rhinitis. Zileuton (Zyflo) prevents leukotriene synthesis. (See Chapter 19 for a discussion of the role of leukotriene in inflammatory and allergic responses.) Zafirlukast (Accolate) blocks the leukotriene receptor. Both are oral agents and work best in the prevention of allergic rhinitis.
Complementary and Alternative Therapy
Complementary and alternative therapies have helped some patients with rhinitis obtain relief, especially through the use of aromatherapy. Possible mechanisms of action include competition and desensitization. Some patients with pollen allergies report decreased problems after eating unprocessed honey.
Desensitization Therapy
Desensitization therapy, commonly called “allergy shots,” may be needed when allergens are identified and cannot be avoided easily. It involves subcutaneous injections of small amounts of the allergen. After the allergen has been identified, a very dilute injection solution (1 : 100,000 or 1 : 1,000,000) of the allergen is compounded. A 0.05-mL dose of this solution is injected subcutaneously. Usually an increasing dose is given weekly (or more often) until the patient is receiving a 0.5-mL dose. The patient is then started on the lowest dose of the next higher concentration of allergen solution. The process is repeated with increasing concentrations of allergen solutions until the patient is receiving the maximum dose of the greatest concentration (usually 1 : 100), depending on his or her response. Injections are usually given at weekly intervals during the first year, every other week for the second year, and then every 3 to 4 weeks for the third year. The recommended course of treatment is about 5 years.
Desensitization appears to reduce allergic responses by competition. In theory, the very small amounts of allergen first injected are too low to bind to the IgE already present but are enough to induce immunoglobulin G (IgG) production against that allergen. Because IgG is not associated with either mast cells or basal cells, allergens that bind to IgG do not trigger allergic responses. IgG removes the allergen from the body by precipitation (see Chapter 19). By gradually increasing the allergen injection, large amounts of IgG are produced against the allergen. When the patient is then exposed to the allergen in the environment, the IgG binds to it and clears it from the body before IgE can bind to it and trigger an allergic reaction. Because so much more IgG can be produced compared with IgE, IgG is successful in the competition to bind the allergen.
Anaphylaxis
Pathophysiology
Anaphylaxis, the most dramatic and life-threatening example of a type I hypersensitivity reaction, occurs rapidly and systemically. It affects many organs within seconds to minutes after allergen exposure. Anaphylaxis is not common, although the incidence appears to be rising along with the general increase in the incidence of allergic reactions. The episodes can vary in severity, and it can be fatal. The major factor in fatal outcomes for anaphylaxis is a delay in the administration of epinephrine (Walker et al., 2010; Watson, 2010; White, 2010). Many substances can trigger anaphylaxis in a susceptible person (Table 22-2). Drugs and dyes are more common causes of anaphylaxis in acute care settings; food and insect stings/bites are more common causes of anaphylaxis in community settings.
TABLE 22-2
COMMON AGENTS THAT CAUSE ANAPHYLAXIS