Chapter 49 Care of Patients with Eye and Vision Problems
Safe and Effective Care Environment
1. Use aseptic technique when performing an eye examination or instilling drugs into the eye.
2. Apply the principles of infection control when caring for a patient with an eye infection.
3. Orient the patient with reduced vision to his or her immediate environment.
4. Ensure that all members of the health care team are aware of a patient’s visual limitations and need for assistance.
Health Promotion and Maintenance
5. Teach all people, especially those older than 40 years, to have an annual eye examination including measurement of intraocular pressure.
6. Teach patients and family members how to correctly instill ophthalmic drops and ointment into the eye.
7. Teach the patient and family how to alter the home environment for patient safety.
8. Teach patients and family members about what to expect during procedures to correct vision and eye problems.
9. Provide opportunities for the patient and family to express concerns about a change in vision.
10. Refer the patient with reduced vision to local services for the blind.
11. Teach the patient with reduced vision about techniques for performing ADLs and self-care independently.
12. Explain the consequences of increased intraocular pressure (IOP).
13. Identify common actions, conditions, and positions that increase IOP.
14. Prioritize educational needs for the patient after cataract surgery with lens replacement.
15. Prioritize educational needs for patients with primary open-angle glaucoma.
16. Describe the mechanisms of action and nursing implications of drug therapy for glaucoma.
http://evolve.elsevier.com/Iggy/
Answer Key for NCLEX Examination Challenges and Decision-Making Challenges
Review Questions for the NCLEX® Examination
Eyelid Disorders
Entropion and Ectropion
Demonstrate instillation of eyedrops, and evaluate the patient’s ability to instill the drops. Instruct the patient to leave the patch in place until he or she is seen by the ophthalmologist and to report any pain or drainage under the patch. Teach the patient or family member how to clean the suture line with a cotton swab and the prescribed solution. A small amount of antibiotic ointment may be applied (Fig. 49-1). Chart 49-1 describes how to apply ophthalmic ointment. Chart 49-2 lists information on common ophthalmic drugs for eye inflammation and infection.
Chart 49-1 Best Practice For Patient Safety & Quality Care
Instillation of Ophthalmic Ointment
• Check the name, strength, and expiration date of the ointment to be instilled. Be sure it is an ophthalmic (eye) preparation and not a general topical ointment.
• Check to see whether only one eye is to receive the drug or if both eyes are to receive the drug.
• If both eyes are to receive the same drug and one eye is infected, use two separate tubes and carefully label each tube with “right” or “left” for the correct eye.
• Wash your hands and put on gloves.
• Explain the procedure to the patient.
• Have the patient sit in a chair, and you stand behind the patient.
• Ask the patient to tilt the head backward, with the back of the head resting against your body and looking up at the ceiling.
• Gently pull the lower lid down against the patient’s cheek, forming a small pocket.
• Hold the tube (with the cap off) like a pencil, with the tip pointing down.
• Rest the wrist holding the tube against the patient’s cheek.
• Without touching any part of the eye or lid with the tip of the tube, gently squeeze the tube and release about a  – to
– to  -inch thin strip of ointment into the pocket you have made with the patient’s lower lid. Start at the nose side of the pocket, and move toward the outer edge of the pocket.
-inch thin strip of ointment into the pocket you have made with the patient’s lower lid. Start at the nose side of the pocket, and move toward the outer edge of the pocket.
• Gently release the lower lid.
• Tell the patient to close the eye gently (without squeezing the lids tightly).
• With the patient’s eye closed, gently wipe away any excess ointment with a tissue.
• Tell the patient that sight in that eye will be blurred while the ointment is present in the eye and that he or she should not drive or operate heavy machinery until the ointment is removed.
• Remove your gloves, and place the cap back on the tube.
• Ask the patient to keep the eye closed for about 1 minute.
• To remove ointment from the eye, wear gloves if drainage is present.
• Then ask the patient to close the eye; wipe the closed lids with a clean tissue from the corner of the eye nearest the nose outward. If you are wiping the same eye twice, use a different area of the tissue or use a new one.
Chart 49-2 Common Examples of Drug Therapy
Eye Inflammation and Infection
| DRUG | NURSING INTERVENTIONS*† | RATIONALES |
|---|---|---|
| Topical Anesthetics | ||
| Remind the patient not to rub or touch the eye while it is anesthetized. | Touching may injure the eye. | |
| Patch the eye if the patient leaves the facility before the anesthetic wears off. | The use of a patch prevents injury, such as corneal abrasion. | |
| Instruct the patient not to use discolored solution. | Discoloration is a sign of altered drug composition. | |
| Teach the patient to store the bottle tightly closed. | Air may cause drug contamination and oxidation. | |
| Topical Steroids | ||
| Tell the patient to shake the bottle vigorously before use. | Drug is a suspension; shaking is required to distribute the drug evenly in the solution. | |
| Teach the patient to check for corneal ulceration (pain, reduced vision, secretions). | Steroid use predisposes the patient to local infection. | |
| Warn the patient not to share eyedrops with others. | Disease transmission is possible when sharing eyedrops. | |
| Anti-Infective Agents | ||
| Teach the patient the importance of using the drug exactly as prescribed, even if he or she needs to use it hourly. | Bacterial and fungal eye infections worsen rapidly and can lead to blindness if not treated adequately. | |
| Teach the patient how to clean exudate from the eyes before using drops. | Cleansing decreases the risk for contaminating the drug and increases contact of the conjunctiva with the drug. | |
| Reinforce the importance of completing the prescribed drug regimen. | Adherence is critical to maintain a therapeutic level of drug. | |
| Antibiotic-Steroid Combinations | ||
| This is the same as for the general anti-infective agents alone and for the steroids alone. | This is the same as for the general anti-infective agents alone and for the steroids alone. | |
| Topical Antiviral Agents | ||
| Teach the patient to refrigerate the drug and protect it from light. | Drug stability is affected by warm temperatures and light. | |
| Teach the patient to assess for itching lids and burning eyes. | Sensitivity to these drugs is common. | |
| Antifungal Agents | ||
| Teach the patient to assess for itching lids and burning eyes. | Sensitivity to these drugs is common. | |
| Nonsteroidal Anti-Inflammatory Agents | ||
| Teach the patient to check for bleeding in the eye. | These drugs disrupt platelet aggregation. | |
| Teach the patient not to wear soft contact lenses during therapy with these drugs. | These drugs interact with contact lens materials and increase the risk for infection. | |
* When instilling eyedrops, teach patients to use nasal punctal occlusion to reduce the risk for systemic absorption and side effects.
† When more than one topical ophthalmic drug is prescribed, teach patients to separate the instillation of each drug by at least 5 minutes.
Drug Alert
Hordeolum
Nursing interventions include instructing the patient how to apply compresses. Chart 49-3 describes the proper technique for application of an eye compress.
Chart 49-3 Patient and Family Education
Preparing for Self-Management: Application of an Ocular Compress
• Fold a clean washcloth into fourths.
• Soak the washcloth with running tap water that is warm to your inner wrist. (If cool compresses are needed, follow the same steps using cold running tap water.)
• Place the cloth over your closed eye.
• Keep the cloth in place with minimal pressure until the cloth cools (or warms, if cool compresses are prescribed).
• Refold the washcloth so that a different “fourth” will be held against the eye.
• Resoak the cloth with running tap water.
• Repeat applications three times for as many times each day as prescribed by your health care provider.
Chalazion
After surgery, antibiotic ointment is instilled and the eye is covered with a patch. Best practices for application of a nonpressure eye patch are described in Chart 49-4.
Chart 49-4 Best Practice for Patient Safety & Quality Care
Application of an Eye Patch
Nonpressure Eye Patch
2. Explain the procedure to the patient.
4. Apply a skin preparation to the patient’s forehead and cheek.
5. Instruct the patient to close both eyes gently.
6. Place a patch over the closed eyelid.
7. Apply tape from the cheek to the middle of the forehead in a diagonal line.
8. Cover the patch with overlapping pieces of tape.
Keratoconjunctivitis Sicca
Pathophysiology
Keratoconjunctivitis sicca, or dry eye syndrome, results from changes in tear production, tear composition, or tear distribution. Drugs (e.g., antihistamines, beta-adrenergic blocking agents, anticholinergic drugs) also can reduce tear production. Diseases associated with decreased tear production include rheumatoid arthritis, leukemia, sarcoidosis, and Sjögren’s syndrome. Radiation or chemical burns to the eye also decrease tear production. Injury to cranial nerve VII inhibits tears. Eye dryness may follow vision-enhancing surgery. Dry eye syndromes are much more common in women than in men (Pullen & Hall, 2010).
Patient-Centered Collaborative Care
Health Promotion and Maintenance
Conjunctival Disorders
Conjunctivitis
Conjunctivitis is an inflammation or infection of the conjunctiva. Inflammation occurs from exposure to allergens or irritants. Infectious conjunctivitis occurs with bacterial or viral infection and is readily transmitted from person to person (Saligan & Yeh, 2008).
Allergic conjunctivitis manifestations are edema, a sensation of burning, a “bloodshot” eye appearance, excessive tears, and itching. Management includes vasoconstrictor and corticosteroid eyedrops (see Chart 49-2). Teach women to avoid using makeup near the eye until all symptoms have subsided.
Corneal Disorders
Corneal Abrasion, Ulceration, and Infection
Patient-Centered Collaborative Care
Antibiotics, antifungals, and antivirals are prescribed to reduce or eliminate the organisms. Usually, a broad-spectrum antibiotic is prescribed first and may be changed when culture results are known. Steroids may be used with antibiotics to reduce the inflammatory response in the eye. Drugs can be given topically as eyedrops, injected subconjunctivally, or injected IV. Chart 48-4 in Chapter 48 lists best practices for instilling eyedrops. The nursing priorities are to begin the drug therapy, to ensure patient understanding of the drug therapy regimen, and to prevent infection spread.
Often, the anti-infective therapy involves instilling eyedrops every hour for the first 24 hours. Teach the patient how to apply the eyedrops correctly. (See Chart 48-2 in Chapter 48.) Use sterile saline eyedrops to demonstrate the technique, and obtain a return demonstration. If the patient cannot safely self-apply the drugs, teach a family member how to do it.
Keratoconus and Corneal Opacities
Pathophysiology
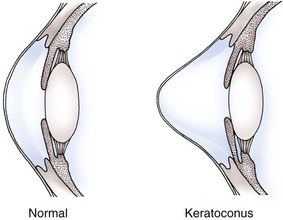
The cornea can permanently lose it shape, become scarred or cloudy, or become thinner. When these conditions occur, refraction is reduced and images are not focused sufficiently for useful vision. Keratoconus, the degeneration of the corneal tissue resulting in abnormal corneal shape, can occur with trauma or may be an inherited disorder (Fig. 49-2). Inadequately treated corneal infections and severe trauma can damage and scar the cornea and lead to severe visual impairment that can be improved only by surgical interventions.
Patient-Centered Collaborative Care
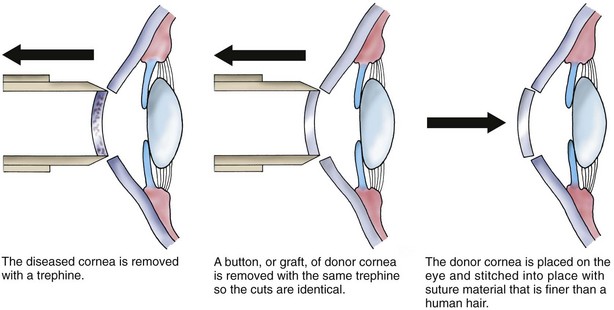
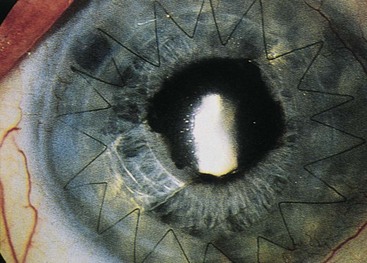
Operative procedures are keratoplasties and are usually performed with local anesthesia in an ambulatory surgical setting. The transplant may involve the entire depth of corneal tissue (penetrating keratoplasty) or only certain layers of the corneal tissue (lamellar keratoplasty). The nerves around and behind the eye are numbed so that the patient cannot move or see out of the eye. The center 7 to 8 mm of the diseased cornea is removed (Fig. 49-3) with an instrument that works like a cookie cutter. The same instrument is used to cut the tissue graft from the donor cornea so that the graft will be a perfect fit. The donor corneal graft is sutured into place on the eye. Fig. 49-4 shows the eye after transplantation. The procedure usually takes about an hour, and the patient is discharged to home 1 to 2 hours after the procedure.
The eye should be protected from any activity that can increase the pressure on, around, or inside the eye. Teach the patient to avoid jogging, running, dancing, and any other activity that promotes rapid or jerky head motions for several weeks after surgery. Other activities that may raise intraocular pressure (IOP) and should be avoided are listed in Table 49-1. Returning to work depends on the type of work. Patients who have sedentary jobs, such as secretaries, may return to work in 1 week, whereas those who perform heavy lifting or manual labor may need to be off work for 6 to 8 weeks.
TABLE 49-1 ACTIVITIES THAT INCREASE INTRAOCULAR PRESSURE
• Raise the head of the bed 30 degrees.
• Instill prescribed antibiotic eyedrops, such as Neosporin or tobramycin.
• Close the eyes, and apply a small ice pack to the closed eyes.
Health Promotion and Maintenance
A. “I have been feeding my cat on the counter so that I don’t have to bend over.”
B. “I have been using an icepack on my eye to reduce the redness and swelling.”
C. “My daughter has been helping me inspect my eye and place the eyedrops.”
D. “Instead of reading a book, I now listen to books on tape.”
Cataract
Pathophysiology
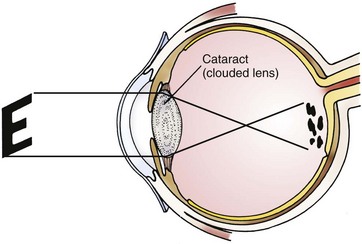
The lens is a transparent, refractive elastic structure suspended behind the iris. A cataract is a lens opacity that distorts the image projected onto the retina (Fig. 49-5). With aging, the lens gradually loses water and increases in density (Touhy & Jett, 2010). This increased density occurs as older lens fibers are compressed and new fibers are produced in the outer layers. Lens proteins dry out and form crystals. As the density of the lens increases, it becomes opaque with a painless loss of transparency. Both eyes may have cataracts; however, the rate of progression in each eye is usually different.
Etiology and Genetic Risk
Cataracts are classified by nature or by onset. They may be present at birth or develop at any time. Cataracts may be age-related or caused by trauma or exposure to toxic agents. They also occur with other diseases and eye disorders (Table 49-2).
TABLE 49-2 COMMON CAUSES OF CATARACTS
| Age-Related Cataracts |
| Traumatic Cataracts |
| Toxic Cataracts |
< div class='tao-gold-member'> Only gold members can continue reading. Log In or Register to continue
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|