Chapter 51 Care of Patients with Ear and Hearing Problems
Safe and Effective Care Environment
1. Apply principles of infection control when examining an ear with drainage.
2. Implement precautions to prevent falls in patients experiencing vertigo or dizziness.
Health Promotion and Maintenance
5. Teach patients and family members about what to expect during tests, procedures, and follow-up to manage ear and hearing problems.
6. Provide opportunities for the patient and family to express feelings and concerns about a change in hearing.
7. Refer hearing-impaired patients and families to local and Internet-based support services.
8. Compare the clinical manifestations and interventions for external otitis with those of otitis media.
9. Safely remove impacted cerumen from the ear canal of an older patient.
10. Coordinate the care of the patient with Ménière’s disease.
11. Prioritize nursing care needs for the patient after tympanoplasty.
12. Prioritize educational needs for the patient after stapedectomy.
13. Identify an appropriate method for communicating with a patient who has recently become hearing impaired.
http://evolve.elsevier.com/Iggy/
Answer Key for NCLEX Examination Challenges and Decision-Making Challenges
Review Questions for the NCLEX® Examination
Conditions Affecting the External Ear
External Otitis
Patient-Centered Collaborative Care
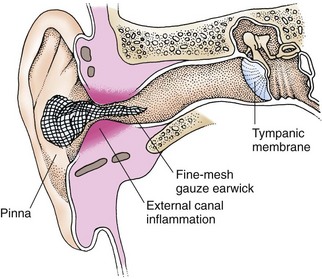
Topical antibiotic and steroid therapies are most effective in decreasing inflammation and pain. Review best practices for instilling eardrops with the patient, as shown in Chart 51-1. Observe the patient self-administer the eardrops to make sure that proper technique is used. If edema obstructs the external canal, an earwick is inserted past the blockage, with drugs applied to the outside end (Fig. 51-1). A long piece of gauze dressing serves as an earwick, which the health care provider inserts using forceps to push carefully through the blocked external auditory canal to the eardrum. The earwick may be removed when eardrops can flow freely into the canal. Use handwashing whenever the infected ear is touched. Oral or IV antibiotics are used in severe cases, especially when infection spreads to surrounding tissue or area lymph nodes are enlarged.
Chart 51-1 Best Practice for Patient Safety & Quality Care
Instillation of Eardrops
• Gather the solutions to be administered.
• Check the labels to ensure correct dosage and time.
• Wear gloves to remove and discard any ear packing.
• Perform a gentle otoscopic examination to determine whether the eardrum is intact.
• Irrigate the ear if the eardrum is intact (see Chart 51-2).
• Place the bottle of eardrops (with the top on tightly) in a bowl of warm water for 5 minutes.
• Tilt the patient’s head in the opposite direction of the affected ear, and place the drops in the ear.
• With his or her head tilted, ask the patient to gently move the head back and forth five times.
• Insert a cotton ball into the opening of the ear canal to act as packing.
Psychosocial Integrity
Cerumen or Foreign Bodies
Pathophysiology
Cerumen (wax) is the most common cause of an impacted canal. A canal can also become impacted as a result of foreign bodies that can enter or be placed in the external ear canal, such as vegetables, beads, pencil erasers, and insects. Although uncomfortable, cerumen or foreign bodies are rarely true emergencies and can be carefully removed by a health care professional. Cerumen impaction in the older adult is common, and removal of the cerumen from older adults often improves hearing (Holcomb, 2009).
Patient-Centered Collaborative Care
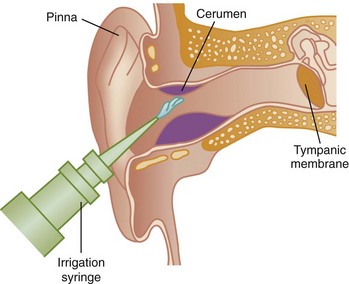
When the occluding material is cerumen, management options include watchful waiting, manual removal, and the use of ceruminolytic agents followed by either manual irrigation or the use of a low-pressure, electronic, oral irrigation device (Holcomb, 2009). The canal can be irrigated with a mixture of water and hydrogen peroxide at body temperature (Fig. 51-2), following best practices for proper irrigation (Chart 51-2). Removal of a cerumen obstruction by irrigation is a slow process and may take more than one sitting. When it is the cause of hearing loss, cerumen removal may improve hearing. Between 50 and 70 ml of solution is the maximum amount that the patient with an impaction usually can tolerate at one sitting.
Chart 51-2 Best Practice For Patient Safety & Quality Care
Ear Irrigation
• Use an otoscope to check the location of the impacted cerumen; ascertain that the eardrum is intact and that the patient does not have otitis media.
• Gather the proper equipment: basin, syringe (without needle), otoscope, towel.
• Warm tap water (or other prescribed solution) to body temperature.
• Fill a syringe with the warmed irrigating solution.
• Place a towel around the patient’s neck.
• Place a basin under the ear to be irrigated.
• Place the tip of the syringe at an angle so that the fluid pushes on one side of and not directly on the impaction (this helps loosen the impaction instead of forcing it further into the canal).
• Apply gentle but firm continuous pressure, allowing the water to flow against the top of the canal.
• Do not use blasts or bursts of sudden pressure.
• If pain occurs, decrease the pressure. If pain persists, stop the irrigation.
• Watch the fluid return for signs of cerumen plug removal.
• Continue to irrigate the ear with about 70 mL of fluid.
• If the cerumen does not drain out, wait 10 minutes and repeat the irrigation procedure.
• Monitor the patient for signs of nausea.
• If the patient becomes nauseated, stop the procedure.
• If the cerumen cannot be removed by irrigation, place (or the patient may place) mineral oil into the ear three times a day for 2 days to soften dry, impacted cerumen, after which irrigation may be repeated.
• After completion of the irrigation, have the patient turn his or her head to the side just irrigated to drain any remaining irrigation fluid.
Action Alert
Discourage the use of cotton swabs and ear candles (hollow tubes coated in wax inserted into the ear and then lighted at the far end) to clean the ears or remove cerumen. Chart 50-3 in Chapter 50 describes steps to teach patients regarding ear hygiene and self–ear irrigation. Refer to Chart 51-3 for nursing care considerations of older adult patients with cerumen impaction.
Chart 51-3 Nursing Focus On The Older Adult
Cerumen Impaction
• Assess the hearing of all older patients using simple voice tests (see Chapter 50).
• Perform a gentle otoscopic inspection of the external canal and eardrum of any older patient who has a problem with hearing acuity, especially the patient who wears a hearing aid.
• Use ear irrigation to remove any impacted cerumen.
• Make certain that the irrigating fluid is about 98.6° F (37° C) to reduce the chance for stimulating the vestibular sense.
• Use no more than 5 to 10 mL of irrigating fluid at a time.
• If nausea, vomiting, or dizziness develops, stop the irrigation immediately.
• Teach the patient how to irrigate his or her own ears.
• Obtain a return demonstration of ear irrigation from the patient, observing for specific areas in which the patient may need assistance.
• Encourage the patient to wash the external ears daily using a soapy, wet washcloth over the index finger (best done in the shower or while washing the hair).
Conditions Affecting the Middle Ear
Otitis Media
Pathophysiology
Acute otitis media and chronic otitis media, also known as suppurant or purulent otitis media, are similar. An infecting agent in the middle ear causes inflammation of the mucosa, leading to swelling and irritation of the small bones (ossicles) within the middle ear, followed by purulent inflammatory exudate. Acute disease has a sudden onset and lasts 3 weeks or less. Chronic otitis media often follows repeated acute episodes, has a longer duration, and causes greater middle ear injury. It may be a result of the continuing presence of a biofilm in the middle ear. A biofilm is a community of bacteria working together to overcome host defense mechanisms to continue to survive and proliferate (Lee et al., 2009). (See Chapter 25 for more information about biofilms.) Therapy for complications associated with chronic otitis media, unlike that of acute otitis media, usually involves surgical intervention.
Patient-Centered Collaborative Care
Assessment
Otoscopic examination findings vary, depending on the stage of the condition. The eardrum is initially retracted, which allows landmarks of the ear to be seen clearly. At this early stage, the patient has only vague ear discomfort. As the condition progresses, the eardrum’s blood vessels dilate and appear red (Fig. 51-3). In the third stage, the eardrum becomes red, thickened, and bulging, with loss of landmarks. Decreased eardrum mobility is evident on inspection with a pneumatic otoscope. Pus may be seen behind the membrane.
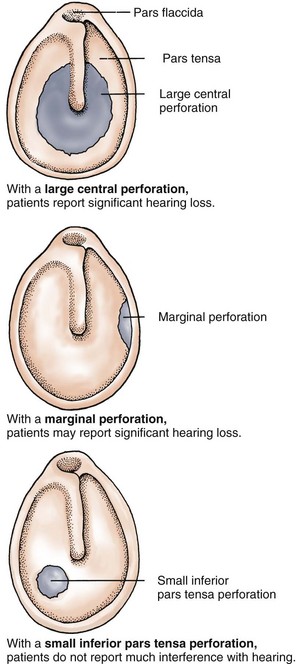
If the condition progresses, the eardrum spontaneously perforates (ruptures) and pus or blood drains from the ear (Fig. 51-4). When the membrane ruptures, the patient notices a marked decrease in pain as the pressure on middle ear structures is relieved (Fig. 51-5). Eardrum perforations from any cause may heal if the underlying problem is controlled. Initially, the eardrum membrane is thinner over the healed perforation. A simple central perforation does not interfere with hearing unless the small bones of the middle ear are damaged or the perforation is large. Repeated perforations with extensive scarring can cause hearing loss.
Interventions
Surgical Management
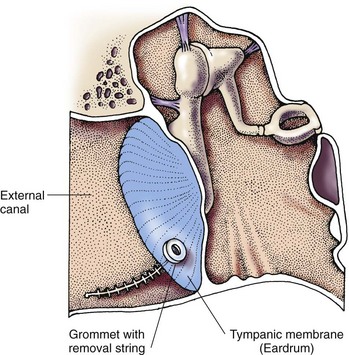
The operative procedure is a small surgical incision often performed in an office or clinic setting and heals rapidly. Another approach is the removal of fluid from the middle ear with a needle. For relief of pressure caused by serous otitis media and for those patients who have repeated episodes of otitis media, a small grommet (polyethylene tube) may be surgically placed through the eardrum to allow continuous drainage of middle ear fluids (Fig. 51-6).
Postoperative care priorities include teaching the patient to keep the external ear and canal free of other substances while the incision is healing. Instruct him or her to keep the head dry by not washing the hair or showering for several days. Other instructions after surgery are listed in Chart 51-4.
Chart 51-4 Patient and Family Education
Preparing for Self-Management: Recovery from Ear Surgery
• Avoid straining when you have a bowel movement.
• Do not drink through a straw for 2 to 3 weeks.
• Avoid air travel for 2 to 3 weeks.
• Avoid excessive coughing for 2 to 3 weeks.
• Stay away from people with respiratory infections.
• If you need to blow your nose, blow gently, without occluding either nostril, with your mouth open.
• Avoid getting your head wet, washing your hair, and showering for 1 week.
• Keep your ear dry for 6 weeks by placing a ball of cotton coated with petroleum jelly (e.g., Vaseline) in your ear. Change the cotton ball daily.
• Avoid rapidly moving the head, bouncing, and bending over for 3 weeks.
• Change your ear dressing every 24 hours or as directed.
Trauma
Patient-Centered Collaborative Care
Nursing care priorities focus on teaching about trauma prevention. Caution patients to avoid inserting objects into the external canal and to follow the steps in Chart 50-3 in Chapter 50 for ear hygiene. Stress the importance of using ear protectors when blunt trauma is likely, especially in sports such as boxing and wrestling.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree