Chapter 28 Care of Patients with Burns
Safe and Effective Care Environment
1. Apply the principles of asepsis to protect burn patients with open wounds.
2. Manage the patient’s environment to prevent infection from auto-contamination and cross-contamination in patients with burn injuries.
Health Promotion and Maintenance
3. Teach everyone fire prevention strategies.
4. Instruct everyone on the correct use and placement of smoke detectors and carbon monoxide detectors.
5. Support the patient and family in coping with permanent changes in appearance and function.
6. Encourage the burn patient with wounds and scars to participate in self-care.
7. Assess the patient’s and family’s use of coping strategies related to burn injury, treatment, possible role changes, and possible outcomes.
8. Allow patients who have lost family members, homes, or jobs time to grieve for these losses.
9. Identify burn patients at risk for inhalation injury.
10. Compare the manifestations of superficial, partial-thickness, and full-thickness burn injuries.
11. Explain the expected manifestations of neural and hormonal compensation during the resuscitation phase of burn injury.
12. Prioritize nursing care for the patient during the resuscitation phase of burn injury.
13. Use laboratory data and clinical manifestations to determine the effectiveness of fluid resuscitation during the resuscitation phase of burn injury.
14. Prioritize nursing care for the patient during the acute phase of burn injury.
15. Coordinate with the registered dietitian to meet the nutritional needs for the patient during the acute phase of burn injury.
16. Evaluate the patient’s wound healing during the acute phase of burn injury.
17. Compare pain management strategies for patients in the resuscitation and acute phases of burn injury.
18. Describe the characteristics of infected burn wounds.
19. Use appropriate positioning and range-of-motion interventions for prevention of mobility problems in the patient with burns.
20. Coordinate nursing care for the patient during the rehabilitation phase of burn injury.
http://evolve.elsevier.com/Iggy/
Answer Key for NCLEX Examination Challenges and Decision-Making Challenges
Audio Clip: High- and Low-Pitched Crackles
Audio Clip: High- and Low-Pitched Wheezes
Review Questions for the NCLEX® Examination
Introduction to the Burn Problem
Pathophysiology of Burn Injury
Skin Changes Resulting from Burn Injury
Anatomic Changes
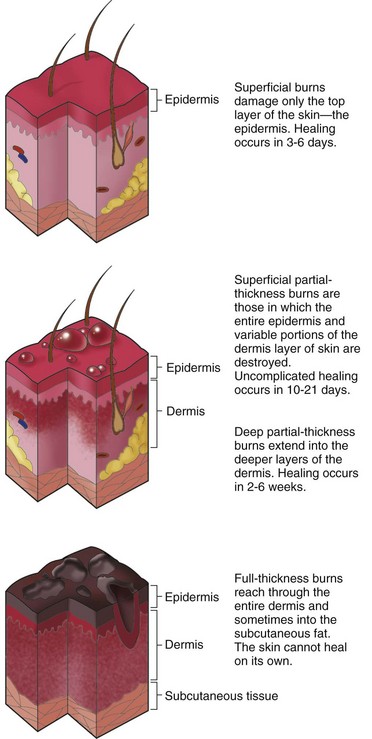
The skin is the largest organ of the body (see Chapter 26). Each of its two major layers, the epidermis and the dermis, has several sublayers. The epidermis, the outer layer of skin, is a layer of stratified epithelial cells about 0.15 mm thick (somewhat thinner in older adults). This layer can grow back after a burn injury because the epidermal cells surrounding sweat and oil glands and hair follicles extend into dermal tissue and regrow to heal partial-thickness wounds. Together, the sweat and oil glands and the hair follicles are the dermal appendages. The depth of the dermal appendages varies in different body areas. The sweat and oil glands in the palm of the hand and the sole of the foot, for example, extend deep into the dermis. This allows for healing of deep burns in these areas. The epidermis has no blood vessels. Nutrients to this layer diffuse from the second layer of skin, the dermis.
Functional Changes
The skin has many functions (see Table 26-1 in Chapter 26). It is a protective barrier against injury and microbial invasion. Burns break this barrier, greatly increasing the risk for infection.
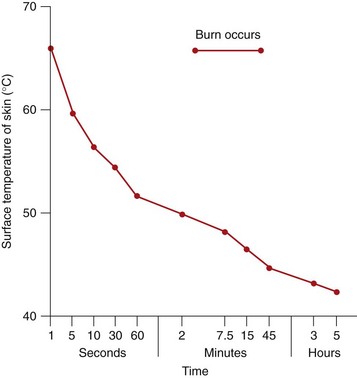
The skin can tolerate temperatures up to 104° F (40° C) without injury. At temperatures of 158° F (70° C) and above, cell destruction is so rapid that even brief exposure damages the skin and tissue below the skin. Fig. 28-1 shows the relationship between temperature and exposure time for burn injury.
Depth of Burn Injury
Differences in skin thickness in various parts of the body also affect burn depth. In areas where the skin is thin (e.g., eyelids, ears, nose, genitalia, tops of the hands and feet, fingers, and toes), a short exposure to high temperatures causes a deep burn injury. The skin is thinner in older adults (Touhy & Jett, 2010), which increases their risk for greater burn severity, even at lower temperatures of shorter duration.
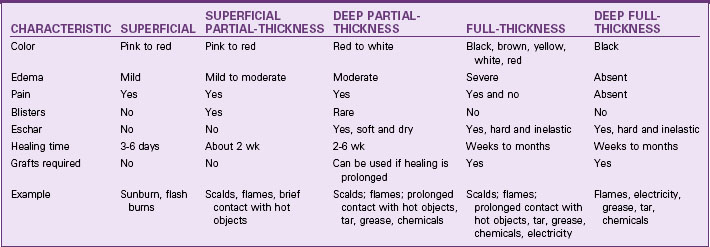
Burn wounds are classified as superficial-thickness wounds, partial-thickness wounds, full-thickness wounds, and deep full-thickness wounds. The partial-thickness wounds are further divided into superficial and deep subgroups (McCance et al, 2010). Table 28-1 lists the clinical differences of these burns.
The American Burn Association (ABA) describes burns as minor, moderate, or major depending on the depth, extent, and location of injury (Table 28-2). Fig. 28-2 shows the tissue layers involved with different depths of injury.
TABLE 28-2 CLASSIFICATION OF BURN INJURY AND BURN CENTER REFERRAL CRITERIA
| CHARACTERISTICS | COMMENTS |
|---|---|
| Minor Burns | |
| Deep partial-thickness burns less than 15% TBSA Full-thickness burns less than 2% TBSA No burns of eyes, ears, face, hands, feet, or perineum No electrical burns No inhalation injury No complicated additional injury Patient is younger than 60 years and has no chronic cardiac, pulmonary, or endocrine disorder | Patients in this category should receive emergency care at the scene and be taken to a hospital emergency department. A special expertise hospital or designated burn center is usually not necessary. |
| Moderate Burns | |
| Deep partial-thickness burns 15%-25% TBSA Full-thickness burns 2%-10% TBSA No burns of eyes, ears, face, hands, feet, or perineum No electrical burns No inhalation injury No complicated additional injury Patient is younger than 60 years and has no chronic cardiac, pulmonary, or endocrine disorder | Patients in this category should receive emergency care at the scene and be transferred either to a special expertise hospital or to a designated burn center. |
| Major Burns | |
| Partial-thickness burns greater than 25% TBSA Full-thickness burns greater than 10% Any burn involving the eyes, ears, face, hands, feet, perineum Electrical injury Inhalation injury Patient is older than 60 years Burn complicated with other injuries (e.g., fractures) Patient has cardiac, pulmonary, or other chronic metabolic disorders | Patients who meet any one of the criteria for a major burn should receive emergency care at the nearest emergency department and then be transferred to a designated burn center as soon as possible. |
TBSA, Total body surface area.
Partial-Thickness Wounds
Superficial partial-thickness wounds are caused by injury to the upper third of the dermis, leaving a good blood supply. These wounds are red and moist and blanch (lighten) when pressure is applied (Fig. 28-3). The small vessels bringing blood to this area are injured, resulting in the leakage of large amounts of plasma, which in turn lifts off the heat-destroyed epidermis, causing blister formation. The blisters continue to increase in size after the burn as cell and protein breakdown occur. Small blisters are often left intact if they are not located over a joint. Large blisters usually are opened and débrided to promote healing.
Deep partial-thickness wounds extend deeper into the skin dermis, and fewer healthy cells remain. Blisters usually do not form because the dead tissue layer is thick, sticks to the underlying dermis, and does not readily lift off the surface. The wound surface is red and dry with white areas in deeper parts (dry because fewer blood vessels are patent). When pressure is applied to the burn, it blanches slowly or not at all (Fig. 28-4). Edema is moderate, and pain is less than with superficial burns because more of the nerve endings have been destroyed.
Full-Thickness Wounds
A full-thickness wound occurs with destruction of the entire epidermis and dermis, leaving no skin cells to repopulate (Fig. 28-5). This wound does not regrow, and areas not closed by wound contraction (see Chapter 27) require grafting.
The full-thickness burn has a hard, dry, leathery eschar that forms from coagulated particles of destroyed dermis. The eschar is dead tissue; it must slough off or be removed from the wound before healing can occur. These thick particles often stick to the lower tissue layer by collagen fibers, which make eschar removal difficult. Edema is severe under the eschar in a full-thickness wound. When the injury is circumferential (completely surrounds an extremity or the chest), blood flow and chest movement for breathing may be reduced by tight eschar. Escharotomies (incisions through the eschar) or fasciotomies (incisions through eschar and fascia) may be needed to relieve pressure and allow normal blood flow and breathing (see p. 527 of the Surgical Management discussion in the Preventing Hypovolemic Shock and Inadequate Oxygenation section).
Deep Full-Thickness Wounds
Deep full-thickness wounds extend beyond the skin into underlying fascia and tissues. These deep injuries damage muscle, bone, and tendons and leave them exposed. These burns occur with flame, electrical, or chemical injuries. The wound is blackened and depressed, and sensation is completely absent (Fig. 28-6). All full-thickness burns need early excision and grafting. Grafting decreases pain and length of stay and hastens recovery. Amputation may be needed when an extremity is involved.
Physiological Integrity
Vascular Changes Resulting from Burn Injury
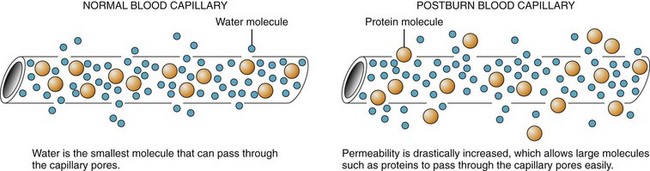
Fluid shift occurs after initial vasoconstriction as a result of blood vessels near the burn dilating and leaking fluid into the interstitial space (Fig. 28-7). This fluid shift, also known as third spacing or capillary leak syndrome, is a continuous leak of plasma from the vascular space into the interstitial space. The loss of plasma fluids and proteins decreases blood volume and blood pressure. Leakage of fluid and electrolytes from the vascular space continues, causing extensive edema, even in areas that were not burned. Fluid shift, with excessive weight gain, occurs in the first 12 hours after the burn and can continue for 24 to 36 hours.
Pulmonary Changes Resulting from Burn Injury
Respiratory damage from an inhalation injury can occur in the upper and major airways and the lung tissue (Cancio et al., 2007). The upper airway is affected when inhaled smoke or irritants cause edema and obstruct the trachea. Irritants coming in contact with the upper airway often cause a reflex closure of the vocal cords. This protective reflex reduces the entry of smoke and toxic gases into the lungs. Heat can reach the upper airway, causing an inflammatory response that leads to edema of the mouth and throat with the potential of airway obstruction.
Gastrointestinal Changes Resulting from Burn Injury
Curling’s ulcer (acute gastroduodenal ulcer that occurs with the stress of severe injury) may develop within 24 hours after a severe burn injury because of reduced GI blood flow and mucosal damage (McCance et al., 2010). The mucus lining the stomach normally is a barrier to the hydrogen ions secreted into the stomach contents. With decreased gastric mucus production, this barrier is disrupted and hydrogen ion production is increased and ulcers may develop as a result. However, this complication is now less common because of the use of H2 histamine blockers, proton pump inhibitors, drugs that protect GI tissues, and early enteral feeding.
Compensatory Responses to Burn Injury
Inflammatory compensation can be helpful by triggering healing in the injured tissues. It also is responsible for some of the serious problems that occur with the fluid shift. Inflammatory compensation causes blood vessels to leak fluid into the interstitial space and white blood cells to release chemicals that trigger local tissue reactions. These responses cause the massive fluid shift, edema, and hypovolemia that are seen in the resuscitation phase (first 24 to 48 hours) after a burn injury. The extent of the inflammatory response depends on the burn severity. Chapter 19 explains the inflammatory responses in detail.
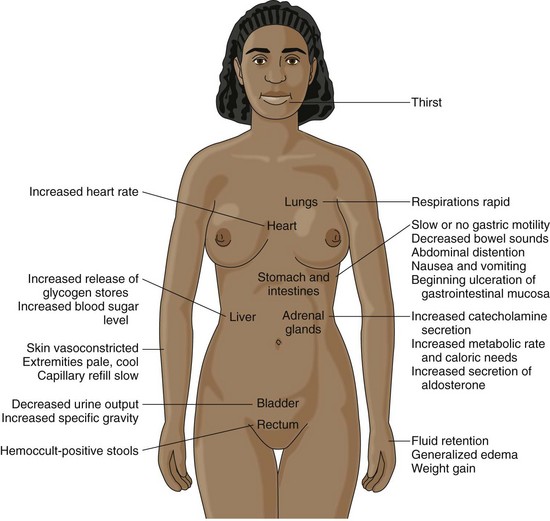
Sympathetic nervous system compensation is the stress response that occurs when any physical or psychological stressors are present. Changes caused by sympathetic compensation are most evident in the cardiovascular, respiratory, and GI systems. Fig. 28-8 shows the results of sympathetic nervous system stimulation.
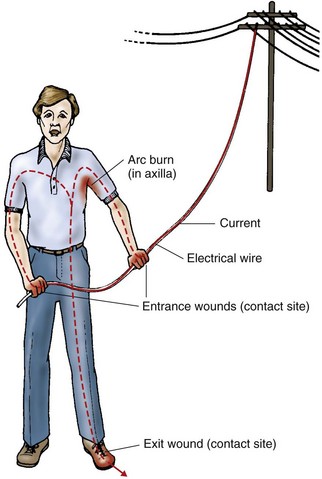
Etiology of Burn Injury
Electrical injuries are burns occurring when an electrical current enters the body (Fig. 28-9). These injuries have been called the “grand masquerader” of burns because the surface injuries may look small but the associated internal injuries can be huge. Tissue injury from electrical trauma results from electrical energy being converted to heat energy. The extent of injury depends on the type of current, the pathway of flow, the local tissue resistance, and the duration of contact. The skin is the most resistant organ; the greatest resistance is in the epidermis of the skin. At high voltages, the difference in tissue resistance is not important. Although various underlying tissues have different resistance to current flow, once skin resistance is overcome, the body acts as a conductor and current flows throughout the involved body part. Bone has a very high resistance because of its density. Current will flow along the surface of the bone, and the heat generated damages the attached muscle. As a result, deep muscle injury may be present even when superficial muscles appear normal or uninjured.
It is difficult to know the exact path a current takes in the body. The course of flow is defined by the locations of the “contact sites,” which are the entrance and exit wounds (Fig. 28-10). At first, the wounds may not be obvious. The path of the injury may involve many internal organs between the two contact sites.
Radiation exposure is more serious in industrial settings where radioactive energy is produced or radioactive isotopes are used. Injury severity depends on the type of radiation, distance from the source, duration of exposure, absorbed dose, and depth of penetration into the body. Chapter 24 discusses potential tissue damage from alpha, beta, and gamma radiation.
Incidence/Prevalence of Burn Injury
Fires and burns are the fifth most common cause of unintentional injury deaths in the United States and the third leading cause of fatal home injuries (American Burn Association, 2010). Although the number of fatalities and injuries caused by residential fires has declined gradually over the past several decades, many residential fire-related deaths remain preventable and continue to pose a significant public health problem.
An estimated 4000 fire and burn deaths occur each year from all sources of burn injury (American Burn Association, 2010). Most deaths occur at the scene of the incident or during transport.
Health Promotion and Maintenance
House fires also are common and lead to severe burns and death. Teach people to reduce the risk for house fires by never smoking in bed, avoiding smoking when drinking alcohol or taking drugs that induce sleep, and keeping matches and lighters out of the reach of children or anyone who is cognitively impaired. If space heaters must be used, stress the importance of keeping clothing, bedding, and other flammable objects away from them. Remind people to keep the screens and doors closed on the fronts of fireplaces and to have chimneys swept each year to prevent creosote buildup. Also remind patients using home oxygen not to smoke or have open flames in a room where oxygen is in use (Edelman et al., 2008).
Resuscitation Phase of Burn Injury
Overview
Events within the first hour after injury can make the difference between life and death for the patient with a burn injury. Immediate care focuses on maintaining an open airway, ensuring adequate breathing and circulation, limiting the extent of injury, and maintaining the function of vital organs. Chart 28-1 outlines the emergency management of a burn injury.
Chart 28-1 Best Practice for Patient Safety & Quality Care
Emergency Management of Burns
General Management for All Types of Burns
Specific Management
Chemical Burns
• If dry chemicals are present on skin or clothing, DO NOT WET THEM.
• Brush off any dry chemicals present on the skin or clothing.
• Remove the patient’s clothing.
• Ascertain the type of chemical causing the burn.
• Do not attempt to neutralize the chemical unless it has been positively identified and the appropriate neutralizing agent is available.
Radiation Burns
• Remove the patient from the radiation source.
• If the patient has been exposed to radiation from an unsealed source, remove his or her clothing (using tongs or lead protective gloves).
• If the patient has radioactive particles on the skin, send him or her to the nearest designated radiation decontamination center.
Patient-Centered Collaborative Care
Assessment
History
Demographic data include age, weight, and height. The rate of serious complications and death from burn injuries is increased among adults older than 50 years. Chart 28-2 lists the age-related differences in older adults’ responses to a burn injury. The patient’s preburn weight is used to calculate fluid rates, energy requirements, and drug doses. This weight is the dry weight, because it represents the patient’s weight before edema begins to form. Calculations based on a weight obtained after fluid replacement is started are not accurate because of water-induced weight gain. Height is important in determining total body surface area (TBSA), which is used to calculate nutritional needs.
Chart 28-2 Nursing Focus On the Older Adult
Age-Related Changes Increasing Complications from Burn Injury
| AGE-RELATED CHANGES | COMPLICATIONS AND NURSING CONSIDERATIONS |
|---|---|
| Thinner skin, sensory impairment, decreased mobility | Sensory impairment and decreased mobility increase the risk for burn injury. Thinner skin increases the depth of injury even when the exposure to the cause of injury is of shorter duration. |
| Slower healing time | Longer time with open areas results in a greater risk for infection and metabolic derangements. |
| More likely to have cardiac impairments | Limits the aggressiveness of fluid resuscitation. Increases the risk for shock and acute kidney injury (AKI). |
| Reduced inflammatory and immune responses | Increases the risk for infection and sepsis. Patient may not have a fever when infection is present. |
| Reduced thoracic and pulmonary compliance | Increased risk for atelectasis, hypoxia, and other pulmonary complications. |
| More likely to have pre-existing medical conditions such as diabetes mellitus, kidney impairment, or pulmonary impairment | Any of these disorders compromise vital organ function and can interfere with fluid resuscitation efforts or other treatments. |
Physical Assessment/Clinical Manifestations
Respiratory Assessment
Patients with major burn injuries and those with inhalation injury are at risk for respiratory problems. Respiratory manifestations common with a burn injury are listed in Table 28-3. Thus continuous airway assessment is a nursing priority (Brown-Guttovz, 2011).
TABLE 28-3 FACTORS DETERMINING INHALATION INJURY OR AIRWAY OBSTRUCTION
Direct Airway Injury
A change in respiratory pattern may indicate a pulmonary injury. The patient may:
• Drool or have difficulty swallowing
• Produce sounds on exhalation that include audible wheezes, crowing, and stridor
Any of these changes may mean the patient is about to lose his or her airway.
Critical Rescue
Carbon Monoxide Poisoning
CO is rapidly transported across the lung membrane and binds tightly to hemoglobin in place of oxygen to form carboxyhemoglobin (CoHb). CO also causes the oxyhemoglobin dissociation curve to shift to the left, which impairs oxygen unloading at the tissue level. This shift results in reduced oxygen delivery because 98% of the oxygen supplied to the tissues comes bound to hemoglobin. Even though the oxygen-carrying capacity of the hemoglobin is reduced, the blood gas value of partial pressure of arterial oxygen (PaO2) is normal (Laing, 2010). The vasodilating action of carbon monoxide causes the “cherry red” color (or at least the absence of cyanosis) in these patients. Manifestations vary with the concentration of CoHb. Table 28-4 lists the effects of carbon monoxide poisoning.
TABLE 28-4 PHYSIOLOGIC EFFECTS OF CARBON MONOXIDE POISONING
| CARBON MONOXIDE LEVEL | PHYSIOLOGIC EFFECTS |
|---|---|
| 1%-10% (normal) | |
| 11%-20% (mild poisoning) | |
| 21%-40% (moderate poisoning) | Decreased blood pressure, increased and irregular heart rate Depressed ST segment on ECG and dysrhythmias Only gold members can continue reading. Log In or Register to continue
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|