Chapter 30 Care of Patients Requiring Oxygen Therapy or Tracheostomy
Safe and Effective Care Environment
1. Act as a patient advocate for patients receiving oxygen or who have tracheostomies.
2. Protect from injury the patient receiving oxygen or who has a tracheostomy.
3. Use medical asepsis when providing tracheostomy care.
4. Verify safe use of appropriate oxygen delivery systems and tracheostomy equipment.
Health Promotion and Maintenance
6. Support the patient and family in coping with changes in breathing status and the need for a tracheostomy.
7. Develop and evaluate an appropriate nonverbal form of communication for a patient with a tracheostomy.
8. Perform a focused respiratory assessment and re-assessment to determine adequacy of oxygenation and tissue perfusion.
9. Administer oxygen therapy by nasal cannula, mask, endotracheal tube, or tracheal tube, and evaluate the patient’s response.
10. Apply knowledge of anatomy to prevent aspiration in a patient with a tracheal tube.
11. Teach the patient and family about home management of oxygen therapy or tracheostomy.
12. Assess for complications of oxygen therapy for those patients whose respiratory efforts are controlled by the hypoxic drive.
13. Use laboratory data and clinical manifestations to determine the presence of hypoxemia or hypercarbia.
http://evolve.elsevier.com/Iggy/
Answer Key for NCLEX Examination Challenges and Decision-Making Challenges
Review Questions for the NCLEX® Examination
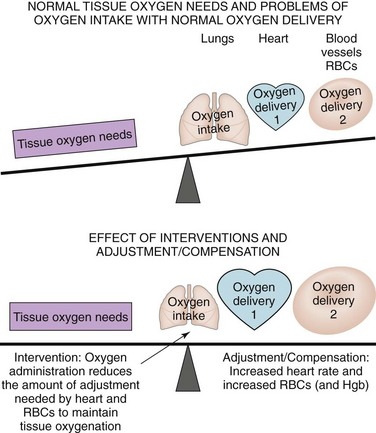
Oxygen is essential for the life and function of all cells and tissues. Three systems—the respiratory system, the cardiovascular system, and the hematologic system—work together to ensure sufficient tissue perfusion with oxygen for cell survival and proper function (see Fig. 29-1). Oxygenation and tissue perfusion needs can be inadequate as a result of many problems with the lungs. When a respiratory problem interferes with adequate oxygenation, both the cardiac system and the hematologic system adjust (compensate) and work harder to restore balance and maintain oxygenation and tissue perfusion (Fig. 30-1). Oxygen therapy and the use of a tracheostomy are interventions that can help improve oxygenation and tissue perfusion and, at the same time, reduce the burden on the cardiovascular and hematologic systems.
Oxygen Therapy
Patient-Centered Collaborative Care
Interventions
Before starting oxygen therapy and while caring for a patient receiving oxygen therapy, you must be knowledgeable about oxygen hazards and complications. Know the rationale and the expected outcome related to oxygen therapy for each patient receiving oxygen. Chart 30-1 lists best practices for patients using oxygen therapy.
Chart 30-1 Best Practice for Patient Safety & Quality Care
Oxygen Therapy
• Check the physician’s prescription with the type of delivery system and liter flow or percentage of oxygen actually in use.
• Obtain a prescription for humidification if oxygen is being delivered at 4 L/min or more.
• Be sure the oxygen and humidification equipment are functioning properly.
• Check the skin around the patient’s ears, back of the neck, and face every 4 to 8 hours for pressure points and signs of irritation.
• Ensure that mouth care is provided every 8 hours and as needed; assess nasal and oral mucous membranes for cracks or other signs of dryness.
• Pad the elastic band and change its position frequently to prevent skin breakdown.
• Pad tubing in areas that put pressure on the skin.
• Cleanse the cannula or mask by rinsing with clear, warm water every 4 to 8 hours or as needed.
• Cleanse skin under the tubing, straps, and mask every 4 to 8 hours or as needed.
• Lubricate the patient’s nostrils, face, and lips with nonpetroleum cream to relieve the drying effects of oxygen.
• Position the tubing so it does not pull on the patient’s face, nose, or artificial airway.
• Ensure that there is no smoking and that no candles or matches are lit in the immediate area.
• Assess and document the patient’s response to oxygen therapy.
• Ensure that the patient has an adequate oxygen source during any periods of transport.
• Provide the patient with ongoing teaching and reassurance to enhance his or her adherence with oxygen therapy.
Hazards and Complications of Oxygen Therapy
Combustion
Oxygen itself does not burn, but it supports and enhances combustion. Therefore a fire burns better in the presence of oxygen. For example, when the oxygen content of the air around a lighted cigarette is nearly 50%, the entire cigarette flames up and can catch items nearby on fire (Edelman et al., 2008). Open fires, even small ones like candles or cigarettes, should not be in the same room during oxygen therapy. Take special precautions during oxygen delivery, including posting a sign on the door of the patient’s room. Smoking is prohibited in the patient’s room, including at home, when oxygen is in use.
Oxygen Toxicity
The causes and manifestations of lung injury from oxygen toxicity are the same as those for acute respiratory distress syndrome (ARDS) (see Chapter 34). Initial symptoms include dyspnea, nonproductive cough, chest pain beneath the sternum, and GI upset. As exposure to high levels of oxygen continues, the symptoms become more severe with decreased vital capacity, decreased compliance, crackles, and hypoxemia. Prolonged exposure to high oxygen levels damages lung tissues. Atelectasis, pulmonary edema, hemorrhage, and hyaline membrane formation result. Surviving this critical condition depends on correcting the underlying disease process and decreasing the oxygen amount delivered.
The toxic effects of oxygen are difficult to treat, making prevention a priority. The lowest level of oxygen needed to maintain oxygenation and prevent oxygen toxicity is prescribed. Closely monitor arterial blood gases (ABGs) during oxygen therapy, and notify the health care provider of PaO2 levels greater than 90 mm Hg. Also monitor the prescribed oxygen level and length of therapy to identify patients at higher risk. High oxygen levels are avoided unless absolutely necessary. The use of continuous positive airway pressure (CPAP) with an oxygen mask, bi-level positive airway pressure (BiPAP), or positive end-expiratory pressure (PEEP) on the mechanical ventilator (see Chapter 34) may reduce the amount of oxygen needed. As soon as the patient’s condition allows, the prescribed amount of oxygen is decreased.
Drying of the Mucous Membranes
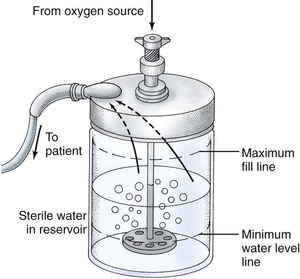
When the prescribed oxygen flow rate is higher than 4 L/min, humidify the delivery system (Fig. 30-2). Ensure that oxygen bubbles through the water in the humidifier.
Infection
Physiological Integrity
Why can oxygen therapy cause hypoventilation in clients who have hypercarbia?
A. Low arterial oxygen levels are the neurologic trigger for these clients to breathe.
B. Excessive carbon dioxide levels reduce the ability of hemoglobin molecules to carry oxygen.
C. High concentrations of oxygen cause sedation, which reduces the strength of respiratory muscle contractions.
D. Unlike people who do not have hypercarbia, these clients are no longer sensitive to changing levels of arterial oxygen.
Oxygen Delivery Systems
The type of delivery system used depends on:
• Oxygen concentration required by the patient
• Oxygen concentration achieved by a delivery system
• Importance of accuracy and control of the oxygen concentration
Low-Flow Oxygen Delivery Systems
Low-flow delivery systems include the nasal cannula, simple facemask, partial rebreather mask, and non-rebreather mask (Table 30-1). These systems are inexpensive, easy to use, and fairly comfortable. A disadvantage is that the actual amount of oxygen delivered varies and depends on the patient’s breathing pattern. The oxygen is diluted with room air (21% oxygen), which lowers the amount of oxygen actually inspired.
TABLE 30-1 COMPARISON OF LOW-FLOW OXYGEN DELIVERY SYSTEMS
| FiO2 DELIVERED | NURSING INTERVENTIONS | RATIONALES |
|---|---|---|
| Nasal Cannula | ||
| Ensure that prongs are in the nares properly. | A poorly fitting nasal cannula leads to hypoxemia and skin breakdown. | |
| Apply water-soluble jelly to nares PRN. | This substance prevents mucosal irritation related to the drying effect of oxygen; promotes comfort. | |
| Assess the patency of the nostrils. | Congestion or a deviated septum prevents effective delivery of oxygen through the nares. | |
| Assess the patient for changes in respiratory rate and depth. | The respiratory pattern affects the amount of oxygen delivered. A different delivery system may be needed. | |
| Simple Facemask | ||
| Be sure mask fits securely over nose and mouth. | A poorly fitting mask reduces the FiO2 delivered. | |
| Assess skin and provide skin care to the area covered by the mask. | Pressure and moisture under the mask may cause skin breakdown. | |
| Monitor the patient closely for risk for aspiration. | The mask limits the patient’s ability to clear the mouth, especially if vomiting occurs. | |
| Provide emotional support to the patient who feels claustrophobic. | Emotional support decreases anxiety, which contributes to a claustrophobic feeling. | |
| Suggest to the health care provider to switch the patient from a mask to the nasal cannula during eating. | Use of the cannula prevents hypoxemia during eating. | |
| Partial Rebreather Mask | ||
| 60%-75% at 6-11 L/min, a liter flow rate high enough to maintain reservoir bag two-thirds full during inspiration and expiration | Make sure that the reservoir does not twist or kink, which results in a deflated bag. | Deflation results in decreased oxygen delivered and rebreathing of exhaled air. |
| Adjust the flow rate to keep the reservoir bag inflated. | The flow rate is adjusted to meet the pattern of the patient. | |
| Non-Rebreather Mask | ||
| 80%-95% FiO2 at a liter flow high enough to maintain reservoir bag two-thirds full | Interventions as for partial rebreather mask; this patient requires close monitoring. | Rationales as for partial rebreather mask. Monitoring ensures proper functioning and prevents harm. |
| Make sure that valves and rubber flaps are patent, functional, and not stuck. Remove mucus or saliva. | Valves should open during expiration and close during inhalation to prevent dramatic decrease in FiO2. Suffocation can occur if the reservoir bag kinks or if the oxygen source disconnects. | |
| Closely assess the patient on increased FiO2 via non-rebreather mask. Intubation is the only way to provide more precise FiO2. | The patient may require intubation. | |
FiO2, Fraction of inspired oxygen.
Nasal Cannula
The nasal cannula, or nasal prongs (Fig. 30-3), is used at flow rates of 1 to 6 L/min. Oxygen concentrations of 24% (at 1 L/min) to 44% (at 6 L/min) can be achieved. Flow rates greater than 6 L/min do not increase oxygenation because the anatomic dead space (places where air flows but the structures are too thick for gas exchange) is full. In addition, high flow rates increase mucosal irritation.
Facemasks
Facemasks for oxygen delivery can deliver a wide range of oxygen flow rates and concentrations.
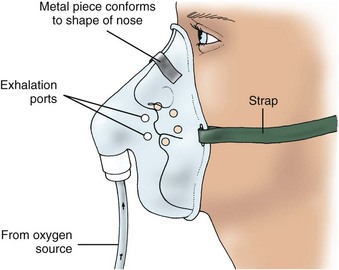
Simple facemasks are used to deliver oxygen concentrations of 40% to 60% for short-term oxygen therapy or in an emergency (Fig. 30-4). A minimum flow rate of 5 L/min is needed to prevent the rebreathing of exhaled air. Ensure the mask fits well to maintain inspired oxygen levels. Care for the skin under the mask and strap to prevent skin breakdown.
Partial rebreather masks provide oxygen concentrations of 60% to 75% with flow rates of 6 to 11 L/min. It is a mask with a reservoir bag but no flaps (Fig. 30-5). With each breath, the patient rebreathes one third of the exhaled tidal volume, which is high in oxygen and provides a higher fraction of inspired oxygen (FiO2). Be sure that the bag remains slightly inflated at the end of inspiration; otherwise, the desired amount of oxygen is not delivered. If needed, call the respiratory therapist for assistance.
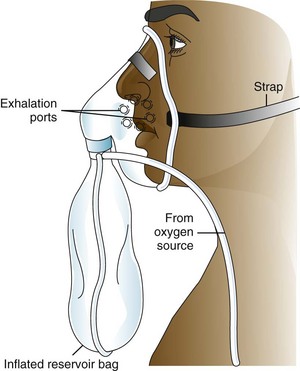
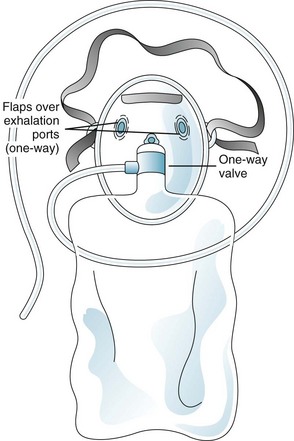
The non-rebreather mask has a one-way valve between the mask and the reservoir and two flaps over the exhalation ports (Fig. 30-6). The valve allows the patient to draw all needed oxygen from the reservoir bag, and the flaps prevent room air from entering through the exhalation ports (room air would dilute the oxygen concentration). During exhalation, air leaves through these exhalation ports while the one-way valve prevents exhaled air from re-entering the reservoir bag. Some models include only one flap on the mask, or one of the exhalation flaps may be removed for safety purposes. The flow rate is kept high (10 to 15 L/min) to keep the bag inflated during inhalation. Assess for this safety feature at least hourly.
High-Flow Oxygen Delivery Systems
High-flow systems (Table 30-2) include the Venturi mask, aerosol mask, face tent, tracheostomy collar, and T-piece. These devices deliver an accurate oxygen level when properly fitted. A high-flow system delivers oxygen concentrations from 24% to 100% at 8 to 15 L/min.
TABLE 30-2 COMPARISON OF HIGH-FLOW OXYGEN DELIVERY SYSTEMS
| FiO2 DELIVERED | NURSING INTERVENTIONS | RATIONALES |
|---|---|---|
| Venturi Mask (Venti Mask) | ||
| 24%-50% FiO2 with flow rates as recommended by the manufacturer, usually 4-10 L/min; provides high humidity | Perform constant surveillance to ensure an accurate flow rate for the specific FiO2. | An accurate flow rate ensures FiO2 delivery. |
| Keep the orifice for the Venturi adaptor open and uncovered. | If the Venturi orifice is covered, the adaptor does not function and oxygen delivery varies. | |
| Provide a mask that fits snugly and tubing that is free of kinks. | FiO2 is altered if kinking occurs or if the mask fits poorly. | |
| Assess the patient for dry mucous membranes. | Comfort measures may be indicated. | |
| Change to a nasal cannula during mealtime. | Oxygen is a drug that needs to be given continuously. | |
| Aerosol Mask, Face Tent, Tracheostomy Collar | ||
| 24%-100% FiO2 with flow rates of at least 10 L/min; provides high humidity | Assess that aerosol mist escapes from the vents of the delivery system during inspiration and expiration. | Humidification should be delivered to the patient. |
| Empty condensation from the tubing. | Emptying prevents the patient from being lavaged with water, promotes an adequate flow rate, and ensures a continued prescribed FiO2. | |
| Change the aerosol water container as needed. | Adequate humidification is ensured only when there is sufficient water in the canister. | |
| T-Piece | ||
| 24%-100% FiO2 with flow rates of at least 10 L/min; provides high humidity | Empty condensation from the tubing. | Condensation interferes with flow rate delivery of FiO2 and may drain into the tracheostomy if not emptied. |
| Keep the exhalation port open and uncovered. | If the port is occluded, the patient can suffocate. | |
| Position the T-piece so that it does not pull on the tracheostomy or endotracheal tube. | The weight of the T-piece pulls on the tracheostomy and causes pain or erosion of skin at the insertion site. | |
| Make sure the humidifier creates enough mist. A mist should be seen during inspiration and expiration. | An adequate flow rate is needed to meet the inspiration effort of the patient. If not, the patient will be “air-hungry.” | |
FiO2, Fraction of inspired oxygen.
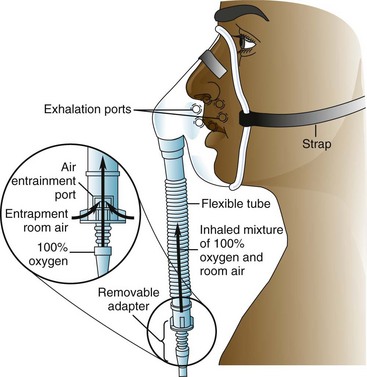
Venturi masks (commonly called Venti masks) deliver the most accurate oxygen concentration without intubation. It works by pulling in a proportional amount of room air for each liter flow of oxygen. An adaptor is located between the bottom of the mask and the oxygen source (Fig. 30-7). Adaptors with holes of different sizes allow specific amounts of air to mix with the oxygen. More precise delivery of oxygen results. Each adaptor uses a different flow rate. For example, to deliver 24% of oxygen, the flow rate must be 4 L/min. Another type of Venturi mask has one adaptor with a dial that is used to select the amount of oxygen desired. Humidification is not needed with the Venturi mask. This system is best for the patient with chronic lung disease because it delivers a more precise oxygen concentration.
< div class='tao-gold-member'>
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree