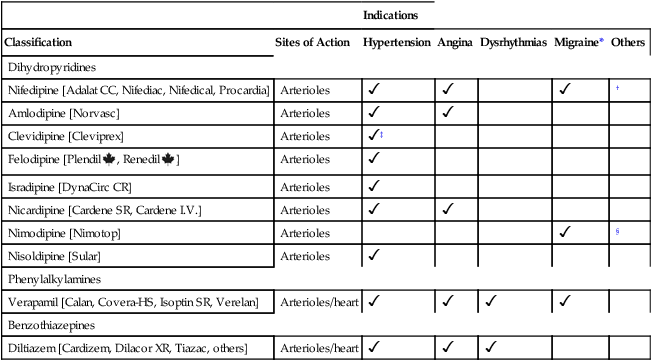
CHAPTER 45 In the heart, calcium channels are coupled to beta1-adrenergic receptors (Fig. 45–1). As a result, when cardiac beta1 receptors are activated, calcium influx is enhanced. Conversely, when beta1 receptors are blocked, calcium influx is suppressed. Because of this relationship, CCBs and beta blockers have identical effects on the heart. That is, they both reduce force of contraction, slow heart rate, and suppress conduction through the AV node. The CCBs used in the United States belong to three chemical families (Table 45–1). The largest family is the dihydropyridines, for which nifedipine is the prototype. This family name is encountered frequently and hence the name is worth remembering. The other two families consist of orphans: verapamil is the only phenylalkylamine, and diltiazem is the only benzothiazepine. The drug names are important; the family names are not. TABLE 45–1 Calcium Channel Blockers: Classification, Sites of Action, and Indications †Suppression of preterm labor (investigational use). ‡Only for IV treatment of severe hypertension. §Prophylaxis of neurologic injury after rupture of an intracranial aneurysm. At therapeutic doses, the dihydropyridines act primarily on arterioles; in contrast, verapamil and diltiazem act on arterioles and the heart (see Table 45–1). However, although dihydropyridines don’t affect the heart at therapeutic doses, toxic doses can produce dangerous cardiac suppression (just like verapamil and diltiazem can). The differences in selectivity among CCBs are based on structural differences among the drugs themselves and structural differences among calcium channels. By blocking calcium channels in the heart and blood vessels, verapamil has five direct effects: • Blockade at peripheral arterioles causes dilation, and thereby reduces arterial pressure. • Blockade at arteries and arterioles of the heart increases coronary perfusion. • Blockade at the SA node reduces heart rate. • Blockade at the AV node decreases AV nodal conduction. • Blockade in the myocardium decreases force of contraction. Of the direct effects on the heart, reduced AV conduction is the most important. Verapamil, administered IV, is used to slow ventricular rate in patients with atrial flutter, atrial fibrillation, and paroxysmal supraventricular tachycardia. Benefits derive from suppressing impulse conduction through the AV node, thereby preventing the atria from driving the ventricles at an excessive rate. Antidysrhythmic applications are discussed in Chapter 49.
Calcium channel blockers
Calcium channels: physiologic functions and consequences of blockade
Heart
Coupling of cardiac calcium channels to beta1-adrenergic receptors.
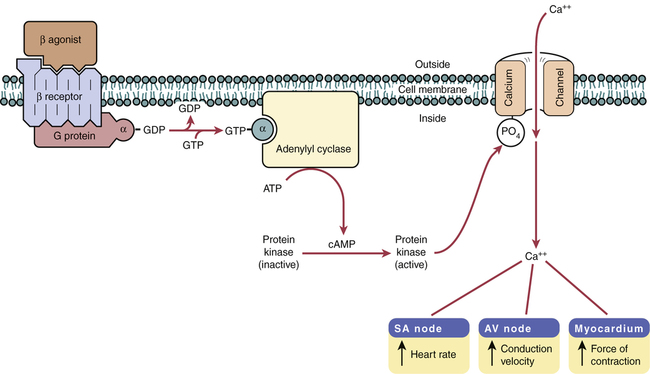
 Coupling of cardiac calcium channels with beta1-adrenergic receptors.
Coupling of cardiac calcium channels with beta1-adrenergic receptors.
In the heart, beta1 receptors are coupled to calcium channels. As a result, when cardiac beta1 receptors are activated, calcium influx is enhanced. The process works as follows. Binding of an agonist (eg, norepinephrine) causes a conformational change in the beta receptor, which in turn causes a change in G protein, converting it from an inactive state (in which GDP is bound to the alpha subunit) to an active state (in which GTP is bound to the alpha subunit). (G protein is so named because it binds guanine nucleotides: GDP and GTP.) Following activation, the alpha subunit dissociates from the rest of G protein and activates adenylyl cyclase, an enzyme that converts ATP to cyclic AMP (cAMP). cAMP then activates protein kinase, an enzyme that phosphorylates proteins—in this case, the calcium channel. Phosphorylation changes the channel such that calcium entry is enhanced when the channel opens. (Opening of the channel is triggered by a change in membrane voltage [ie, by passage of an action potential].)
The effect of calcium entry on cardiac function is determined by the type of cell involved. If the cell is in the SA node, heart rate increases; if the cell is in the AV node, impulse conduction through the node accelerates; and if the cell is part of the myocardium, force of contraction is increased.
Because binding of a single agonist molecule to a single beta receptor stimulates the synthesis of many cAMP molecules, with the subsequent activation of many protein kinase molecules, causing the phosphorylation of many calcium channels, this system can greatly amplify the signal initiated by the agonist.
Calcium channel blockers: classification and sites of action
Classification

Indications
Classification
Sites of Action
Hypertension
Angina
Dysrhythmias
Migraine*
Others
Dihydropyridines
Nifedipine [Adalat CC, Nifediac, Nifedical, Procardia]
Arterioles



†
Amlodipine [Norvasc]
Arterioles


Clevidipine [Cleviprex]
Arterioles
 ‡
‡
Felodipine [Plendil ![]() , Renedil
, Renedil![]() ]
]
Arterioles

Isradipine [DynaCirc CR]
Arterioles

Nicardipine [Cardene SR, Cardene I.V.]
Arterioles


Nimodipine [Nimotop]
Arterioles

§
Nisoldipine [Sular]
Arterioles

Phenylalkylamines
Verapamil [Calan, Covera-HS, Isoptin SR, Verelan]
Arterioles/heart




Benzothiazepines
Diltiazem [Cardizem, Dilacor XR, Tiazac, others]
Arterioles/heart



Sites of action
Verapamil and diltiazem: agents that act on vascular smooth muscle and the heart
Verapamil
Hemodynamic effects
Direct effects.
Therapeutic uses
Cardiac dysrhythmias.



