Chapter 13 Bleeding Disorders
Basic concepts
1 Differentiate between the processes of primary and secondary hemostasis
Primary hemostasis involves the formation of a temporary platelet “plug” following binding of platelets to exposed collagen, platelet secretion of procoagulant substances (e.g., adenosine diphosphate [ADP], Ca2+), and platelet aggregation. This platelet plug is referred to as temporary because it is readily reversible at this stage. Secondary hemostasis involves the covalent cross-linking of fibrin between platelets, resulting in the formation of an irreversible platelet plug. This process is dependent on activation of the coagulation cascade (Table 13-1).
Table 13-1 Primary and Secondary Hemostasis
| Feature | Primary Hemostasis | Secondary Hemostasis |
|---|---|---|
| Definition | Temporary platelet plug | Permanent platelet plug |
| Example disease(s) | Von Willebrand disease | Hemophilia A and B |
| Laboratory testing | Bleeding time, platelet aggregation studies | Prothrombin time (PT), partial thromboplastin time (PTT) |
| Clinical manifestations of disturbed mechanism | Relatively mild (e.g., excessive bleeding after dental work or surgery), mucocutaneous petechiae | Relatively severe (e.g., hemarthrosis) |
3 What constitutes the extrinsic, intrinsic, and common pathways in the coagulation cascade that forms the fibrin clot (secondary hemostasis)?
As mentioned, the common pathway is activated by either the extrinsic pathway or intrinsic pathway, and it eventuates in the formation of a fibrin clot. This pathway includes factors X, V, II, and I (Fig. 13-1).
4 What information can be provided by measuring the prothrombin time and activated partial thromboplastin time?
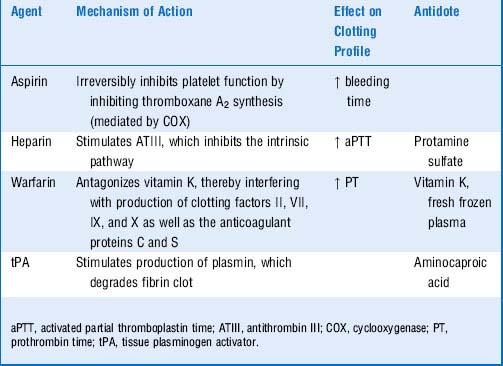
6 What is the mechanism of action of the following drugs? How do they affect the times just discussed?
7 What is the mechanism of action of tissue plasminogen activator?
As its name suggests, tissue plasminogen activator (tPA) is an enzyme that activates the plasma enzyme plasminogen by converting it into its active form, plasmin. Plasmin is an enzyme that proteolytically cleaves fibrin strands, thereby degrading fibrin clots that may obstruct vessels. In addition to tPA, streptokinase and urokinase are sometimes referred to as “clot busters” (Table 13-2).
Summary Box: Hemostasis, Coagulation Cascade, Pharmacotherapy
 Primary hemostasis is the process whereby platelets adhere to the underlying collagen of damaged vascular endothelium and form a temporary platelet “plug.”
Primary hemostasis is the process whereby platelets adhere to the underlying collagen of damaged vascular endothelium and form a temporary platelet “plug.”
 Secondary hemostasis is the process whereby these platelets are covalently cross-linked to form an irreversible platelet plug, a process that requires clotting factors.
Secondary hemostasis is the process whereby these platelets are covalently cross-linked to form an irreversible platelet plug, a process that requires clotting factors.
 Disorders affecting platelet function will impair primary hemostasis. Platelet function can be tested by checking bleeding time (rarely done) or in vitro platelet function tests (more commonly done).
Disorders affecting platelet function will impair primary hemostasis. Platelet function can be tested by checking bleeding time (rarely done) or in vitro platelet function tests (more commonly done).
 Both the extrinsic and intrinsic pathways lead into the common pathway to cause formation of the fibrin clot.
Both the extrinsic and intrinsic pathways lead into the common pathway to cause formation of the fibrin clot.
 The prothrombin time (PT) reflects the time it takes for the extrinsic and common pathways to form a fibrin clot. The PT can be prolonged by clotting factor deficiencies in either pathway.
The prothrombin time (PT) reflects the time it takes for the extrinsic and common pathways to form a fibrin clot. The PT can be prolonged by clotting factor deficiencies in either pathway.
 The activated partial thromboplastin time (aPTT) reflects the time it takes for the intrinsic and common pathways to form a fibrin clot. The aPTT can be prolonged by clotting factor deficiencies in either pathway.
The activated partial thromboplastin time (aPTT) reflects the time it takes for the intrinsic and common pathways to form a fibrin clot. The aPTT can be prolonged by clotting factor deficiencies in either pathway.
 Aspirin irreversibly inhibits platelets by inhibiting cyclooxygenase (COX), preventing the formation of thromboxane A2, which normally promotes platelet aggregation and vasoconstriction in response to endothelial damage. Aspirin therapy results in a prolonged bleeding time.
Aspirin irreversibly inhibits platelets by inhibiting cyclooxygenase (COX), preventing the formation of thromboxane A2, which normally promotes platelet aggregation and vasoconstriction in response to endothelial damage. Aspirin therapy results in a prolonged bleeding time.
 Heparin stimulates antithrombin III activity, thereby inhibiting the intrinsic pathway and prolonging the aPTT. Heparin has no effect on bleeding time because it does not (typically) affect platelet function. Heparin toxicity can be reversed with protamine sulfate.
Heparin stimulates antithrombin III activity, thereby inhibiting the intrinsic pathway and prolonging the aPTT. Heparin has no effect on bleeding time because it does not (typically) affect platelet function. Heparin toxicity can be reversed with protamine sulfate.
 Warfarin (Coumadin) inhibits the synthesis of vitamin K–dependent clotting factors (II, VII, IX, and X) by antagonizing the action of vitamin K. It preferentially prolongs the PT. There is typically a delay of several days before patients achieve a therapeutic international normalized ratio (INR) on warfarin because warfarin inhibits the synthesis of further clotting factors but does not inhibit the activity of existing plasma clotting factors.
Warfarin (Coumadin) inhibits the synthesis of vitamin K–dependent clotting factors (II, VII, IX, and X) by antagonizing the action of vitamin K. It preferentially prolongs the PT. There is typically a delay of several days before patients achieve a therapeutic international normalized ratio (INR) on warfarin because warfarin inhibits the synthesis of further clotting factors but does not inhibit the activity of existing plasma clotting factors.
 Warfarin toxicity can be reversed by administering vitamin K (takes 1-2 days) or fresh frozen plasma (rapid).
Warfarin toxicity can be reversed by administering vitamin K (takes 1-2 days) or fresh frozen plasma (rapid).
 Tissue plasminogen activator (tPA), streptokinase, and urokinase are “clot-busting” drugs that can be used in particular clinical scenarios such as ST-segment elevation myocardial infarction or acute ischemic cerebrovascular accident.
Tissue plasminogen activator (tPA), streptokinase, and urokinase are “clot-busting” drugs that can be used in particular clinical scenarios such as ST-segment elevation myocardial infarction or acute ischemic cerebrovascular accident.
2 What is the cause of this disorder and how is it inherited?
Hemophilia A is caused by a hereditary deficiency of factor VIII and is inherited in an X-linked recessive manner. Females are very rarely affected because the approximate 50% factor levels in most carriers are sufficient to prevent excessive bleeding. In rare circumstances, females may be affected due to unequal inactivation (lyonization) of factor VIII or factor IX alleles (see Chapter 11, Genetic and Metabolic Disease, for more information).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree