7 Assessment of vital signs and changes in health status
• To help the student understand how to assess vital signs and recognise the changes within a patient’s physical and mental health status
• To help the student to recognise and respond to the deteriorating patient on a medical placement
• To explore why a patient’s health status may change and how this can affect their decision making
Introduction
As students from all fields of nursing, you will have been exposed to simulated practice within the university. However, when you are undertaking observations of patients’ vital signs during your medical placement, you may not find them as easy to perform as you did within simulated practice. Patients vary, and it can be daunting at first as patients are sick and your competence is also being assessed. Remember that your mentor is there to help, guide and supervise you and that you should not undertake any clinical skills alone until your mentor has assessed your competence. This assessment of competence should not be carried out on just one patient but with a variety of patients with differing health problems. Always ask for a rationale. As you progress towards your third year of training you will already be competent in the Essential Skills for years one and two (Nursing and Midwifery Council (NMC) 2010). However, your learning outcomes will be expecting you to demonstrate assessment skills, prioritisation and clinical decision making for a group of patients. Some students find this easier than others to achieve, however, good communication with your mentor regarding your learning needs can really help you to develop in this area.
Observations of vital signs and recognition of changes in your patients’ health status will be an essential clinical skill within your learning outcomes regardless of your chosen field of nursing. Undertaking observations of vital signs and recognising changes in patients’ health status will incorporate all of the NMC (2010) Standard Competencies – professional values, communication and interpersonal skills, clinical decision making, and leadership, management and team working. For example, within decision making, part of the standard competency states that: ‘decision making must be person-focused, and through a process of critical analysis learning to a range of technical and nursing interventions from basic to the highly complex’.
For communication, the NMC Competency states that nurses ‘must communicate safely and effectively with individuals and groups of all ages’ (NMC 2010) and you may find that your record of achievement/practice curriculum documentation has mapped the Essential Skills Clusters for care, compassion and communication with the specific competencies within the domains.
When you are undertaking your observations of vital signs, you will behave with professional values, communicate with your patients, make clinical decisions and often need to liaise with multidisciplinary teams (Box 7.1). You will also meet some of the Essential Skills Clusters while undertaking observations of vital signs, for example some of the organisational aspects of care, compassion and communication skills (NMC 2010).
Box 7.1 Some of the specific competencies that you might meet while undertaking observation of vital signs
Field Standard for Competence: Communication and Interpersonal Skills Domain
All nurses must use a range of communication skills and technologies to support person-centred care and enhance the quality and safety of health care. They must make sure that people receive all the information about their care in a language and manner that is right for them, and that allows them to make informed choices and consent to treatment.
Field Standard for Competence: Nursing Practice and Decision-Making Domain
Adult nurses must be able to carry out accurate health, clinical and nursing assessments across all ages and show the right diagnostic and decision-making skills. They must have the confidence to provide effective adult nursing care in the home, community and in the hospital settings.
Adult nurses must recognise early signs of acute illness in young people, adults and older people and accurately assess and start appropriate and timely management of those at risk of clinical deterioration, who are acutely ill or who need emergency care.
Demonstrating competence
Within your first year
Your mentor will expect to see you do the following in your first year:
• Display the professional behaviour and conduct expected of a nurse, for example gaining agreement from the patient first and explaining what needs to be done.
• Report abnormalities – you may not understand why a patient has abnormal vital signs but you would be expected to report it.
• To use the early warning score.
Within your final year
Your mentor will expect to see you do the following in your final year:
• Demonstrate a patient-centred focus.
• Use the early warning score accurately.
• Detect changes and report, recheck, seek guidance.
• Clearly integrate theory and practice.
• Follow policy and role model professional practice behaviour.
• Be able to relate the patient’s health problem to the patient, context and specialty, discuss care and articulate the rationale to the mentor.
• Initiate actions and interventions.
• Initiate, evaluate and reassess the plan of care using a structured approach.
• Be confident in communication with the multidisciplinary team.
Quiz
Temperature
Also see this resource for a demonstration of taking a temperature:
http://www.cetl.org.uk/learning/temperature-a/player.html (accessed July 2011).
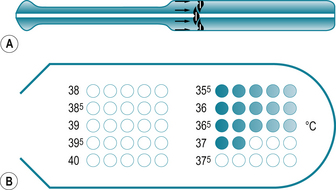
Fig 7.1 (A) Disposable chemical dot thermometer. (B) Recording area of a disposable thermometer
(Holland et al 2008, with permission)
Blood pressure
Also see these resources for a demonstration of taking BP:
http://www.cetl.org.uk/learning/bpm/player.html (accessed July 2011)
http://www.cetl.org.uk/learning/BP_Korotkoff_sounds/player.html
7.17. You are undertaking your placement on medical day care and are caring for Mustafa who has just had a gastroscopy. When you take his observations of pulse and BP, you find that he is tachycardic at 110 beats per minute and his BP has decreased to 90/60 mmHg. What are your thoughts? What could be happening to Mustafa? What nursing actions do you need to take to help Mustafa?
Respiration
7.19. What is the difference between type 1 and type 2 respiratory failure?
7.22. What is a normal respiratory rate?
7.23. How do you assess a patient’s respiratory function?
7.24. What does an abnormal respiratory rate mean?
7.25. Your patient, Henry, is a patient on the virtual ward. He has a long-term health problem of chronic obstructive pulmonary disease (COPD) and when you visit him you notice that he has difficulty speaking in full sentences, has an elevated respiratory rate of 32 breaths per minute and is anxious. What nursing actions could you undertake to help Henry’s breathing? Who else might you need to inform?
Peak expiratory flow rate
7.32. What is peak expiratory flow rate?
7.33. Why and how do we check it?
7.34. What is the normal peak flow reading (predicted or expected)?
7.35. Imran is a 28-year-old man admitted to the acute medical admissions ward with an acute asthma attack. His morning peak flow is 200 L/min, respiratory rate 28/min and saturations 92%. What would your nursing actions be at this point?
Also see this resource for a demonstration of peak flow monitoring:
http://www.youtube.com/watch?v=oHRTiytvuow(accessed July 2011).
Neurological status of your patient
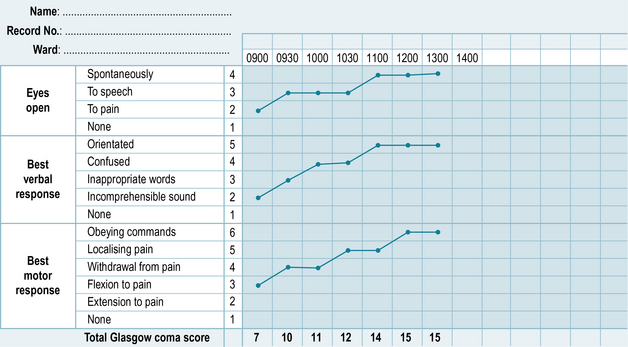
Sometimes you may look after a patient for more than one shift and you may find that you notice a change in how alert they are – sometimes this can be quite a subtle change where your patient seems drowsy or there might be a very sudden change to unresponsive. Another tool that is commonly used is the Glasgow Coma Scale (Fig. 7.5), which comprises of scores for three different measurements – best verbal response, best eye response and best motor response (Brooker & Waugh 2007). The Glasgow Coma Scale takes a lot of practice and it will be helpful for you and your mentor to discuss this in detail when you are caring for a patient who requires this observation, for example a patient who has suddenly become unresponsive or has suffered a cerebral vascular accident.
Delirium
Delirium can be characterised by ‘disturbed consciousness, cognitive function or perception, which has an acute onset and fluctuating course’ (National Institute for Health and Clinical Excellence (NICE) 2010).
• People with dementia or other cognitive impairments.
• People with sensory impairments – poor eyesight, poor hearing.
• Those who are immobile/physically frail.
• Patients with dehydration/infection.
This Website offers excellent explanations about this problem and links to other resources:http://www.nmhdu.org.uk/our-work/mhep/later-life/lets-respect/ (accessed July 2011).
It is important to be able to determine the difference between a chronic cognitive impairment such as dementia and an acute problem like delirium. Box 7.2 shows the main features of delirium.
Box 7.2 The main features of delirium
 Rapid onset, e.g. hours, days, weeks.
Rapid onset, e.g. hours, days, weeks.
 Fluctuating behaviour – comes and goes or increases/decreases in severity.
Fluctuating behaviour – comes and goes or increases/decreases in severity.
 Disturbed level of consciousness, e.g. drowsy or hyperalert.
Disturbed level of consciousness, e.g. drowsy or hyperalert.
 Reduced ability to focus or concentrate, easily distracted.
Reduced ability to focus or concentrate, easily distracted.
 Rambling, incoherent, switching from one subject to another.
Rambling, incoherent, switching from one subject to another.
 Suspicious or paranoid thinking.
Suspicious or paranoid thinking.
The confusion assessment method (CAM) is a useful screening tool to use to help identify delirium (Inouye et al 1990) (see Box 7.3).