Chapter 29 Assessment of the Respiratory System
Health Promotion and Maintenance
1. Encourage all people to use masks and adequate ventilation when engaging in activities that expose them to inhalation irritants and toxins.
2. Teach patients and family members about what to expect during tests and procedures to assess respiratory function and respiratory disease.
3. Assess the patient’s endurance in performing ADLs.
4. Use concepts of anatomy and appropriate psychomotor skills to apply respiratory assessment techniques correctly.
5. Perform a clinical respiratory assessment, including health history, genetic risk, physical assessment, and psychosocial assessment.
6. Distinguish between normal and abnormal (adventitious) breath sounds.
7. Explain the respiratory changes associated with aging.
8. Calculate the pack-year smoking history for the patient who smokes or who has ever smoked cigarettes.
9. Interpret arterial blood gas values to assess the patient’s respiratory status.
10. Explain nursing care needs for the patient after bronchoscopy or open lung biopsy.
http://evolve.elsevier.com/Iggy/
Animation: Patterns of Respiration
Animation: Percussion Tones Throughout the Chest
Animation: Pulmonary Circulation
Answer Key for NCLEX Examination Challenges and Decision-Making Challenges
Audio Clip: Bronchial Breath Sounds
Audio Clip: Bronchovesicular Breath Sounds
Audio Clip: High- and Low-Pitched Crackles
Audio Clip: High- and Low-Pitched Wheezes
Audio Clip: Pleural Friction Rub
Audio Clip: Vesicular Breath Sounds
Review Questions for the NCLEX® Examination
Video Clip: Diaphragmatic Excursion
Video Clip: Inspection of the Nose
Video Clip: Percussion: Anterior Thorax
Video Clip: Respiratory Excursion
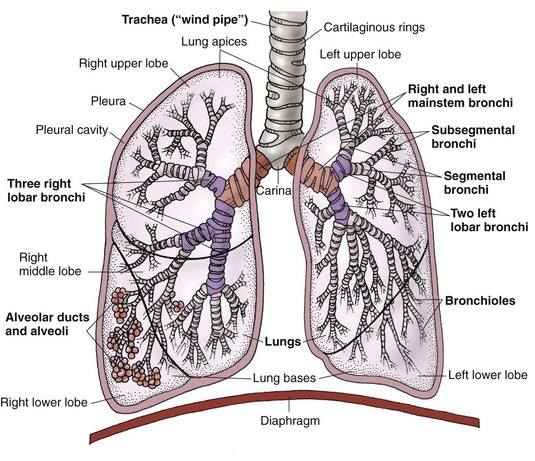
All cells need oxygen (O2) to live and perform their specific jobs. Oxygen intake depends on the respiratory system (Fig. 29-1). The respiratory system is important for oxygenation and tissue perfusion because the source of the oxygen for all body cells is the air we breathe. This system includes the upper airways, lungs, lower airways, and alveolar air sacs. Air with oxygen enters the nose and mouth and moves through the airways or respiratory tubes (trachea, bronchi, bronchioles) and into the air sacs (alveoli) of the lungs. Once in the air sacs, the oxygen from the air moves into the blood so that it can be carried to all tissues and organs. Carbon dioxide (CO2), the waste gas created in the tissues, moves from the blood into the lungs so it can be exhaled. All systems depend on adequate oxygen intake for tissue perfusion with oxygen. Any respiratory problem affects total body health and well-being.
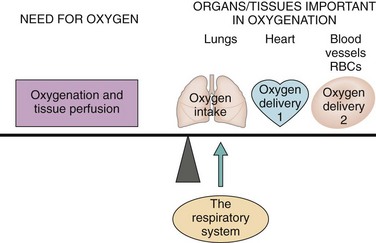
FIG. 29-1 Role of the respiratory system in oxygenation and tissue perfusion. RBCs, Red blood cells.
Lung and breathing problems are common and are the fifth leading cause of death in North America (McCance et al., 2010). Some respiratory problems are chronic, and the patient has physical and lifestyle limitations. Many acute health problems, medical therapies, and surgeries adversely affect respiratory function temporarily or permanently.
Anatomy and Physiology Review
Upper Respiratory Tract
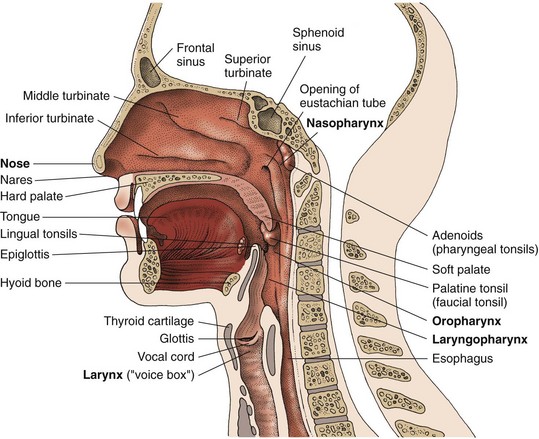
The upper airways consist of the nose, the sinuses, the pharynx, and the larynx (Fig. 29-2).
Nose and Sinuses
The turbinates are three bones that protrude into the nasal cavities from the internal portion of the nose (see Fig. 29-2). Turbinates increase the total surface area for filtering, heating, and humidifying inspired air before it passes into the nasopharynx. Inspired air entering the nose is first filtered in the nares. Particles not filtered out in the nares are trapped in the mucous layer. These particles are moved by cilia (hairlike projections) to the throat, where they are either swallowed or expectorated. Inspired air is humidified by the mucous membrane and is warmed by heat from the vascular network.
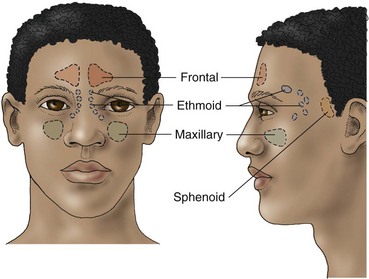
The paranasal sinuses are air-filled cavities within the bones that surround the nasal passages (Fig. 29-3). Lined with ciliated membrane, the purposes of the sinuses are to provide resonance during speech and to decrease the weight of the skull.
Pharynx
The pharynx, or throat, is a passageway for both the respiratory and digestive tracts. It is located behind the oral and nasal cavities. The throat is divided into the nasopharynx, the oropharynx, and the laryngopharynx (see Fig. 29-2).
Larynx
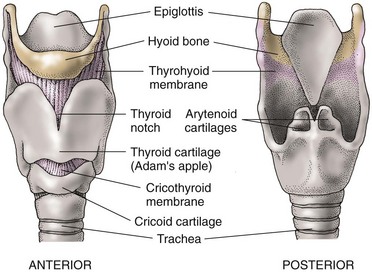
The larynx is the “voice box” and is located above the trachea, just below the throat at the base of the tongue. It is controlled by the recurrent laryngeal nerves. The larynx is composed of several cartilages (Fig. 29-4). The thyroid cartilage is the largest and is commonly called the “Adam’s apple.” The cricoid cartilage, which contains the vocal cords, lies below the thyroid cartilage. The cricothyroid membrane is located below the level of the vocal cords and joins the thyroid and cricoid cartilages. This site is used in an emergency for access to the lower airways. In this procedure, called a cricothyroidotomy, an opening is made between the thyroid and cricoid cartilage and results in a tracheostomy. The two arytenoid cartilages work with the thyroid cartilage in vocal cord movement.
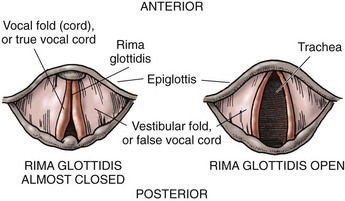
Inside the larynx are two pairs of vocal cords: the false vocal cords and the true vocal cords. The glottis is the opening between the true vocal cords (Fig. 29-5). The epiglottis is a leaf-shaped, elastic structure that is attached along one edge to the top of the larynx. Its hingelike action prevents food from entering the trachea (aspiration) by closing over the glottis during swallowing. The epiglottis opens during breathing and coughing.
Lower Respiratory Tract
Airways
The lower airways are the trachea; two mainstem bronchi; lobar, segmental, and subsegmental bronchi; bronchioles; alveolar ducts; and alveoli (Fig. 29-6). The lower respiratory tract (tracheobronchial tree) is an inverted treelike structure consisting of muscle, cartilage, and elastic tissues. This system of branching tubes, which decrease in size from the trachea to the respiratory bronchioles, allows gases to move to and from the lungs. Gas exchange takes place in the lung tissue between the alveoli and the lung capillaries, not in the airways.
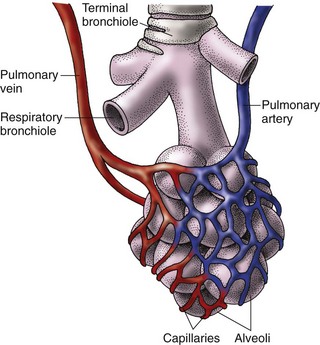
The bronchioles branch from the secondary bronchi and divide into smaller and smaller tubes, which are the terminal and respiratory bronchioles (Fig. 29-7). These tubes have a small diameter, have no cartilage, and depend entirely on the elastic recoil of the lung to remain open.
Alveolar ducts with alveoli attached branch from the respiratory bronchioles and resemble a bunch of grapes. Alveolar sacs arise from these ducts. The alveolar sacs contain groups of alveoli, which are the basic units of gas exchange (see Fig. 29-7). A pair of healthy adult lungs has about 290 million alveoli, which are surrounded by lung capillaries. These numerous small alveoli share common walls, making a large surface area for gas exchange. In a healthy adult, this surface area is about the size of a tennis court. Acinus is a term for the structural unit consisting of a respiratory bronchiole, an alveolar duct, and an alveolar sac.
Lungs
The pulmonary circulation is a highly vascular capillary network. Oxygen-poor blood travels from the right ventricle of the heart into the pulmonary artery, which eventually branches into arterioles that form capillary networks. These capillaries are meshed around and through the alveoli—the site of gas exchange (see Fig. 29-7). Freshly oxygenated blood travels from the capillaries to the pulmonary veins and then to the left atrium. From the left atrium, oxygenated blood flows into the left ventricle, where it is pumped throughout the systemic circulation.
Oxygen Delivery and the Oxygen-Hemoglobin Dissociation Curve
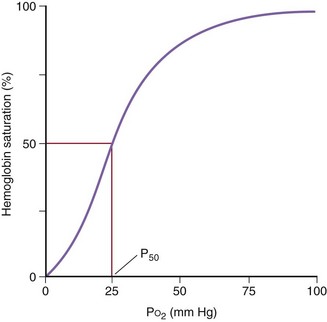
Oxygen delivery to the tissues requires the binding of oxygen to hemoglobin in red blood cells. Each molecule of hemoglobin can bind four oxygen molecules, which fills or saturates all of its binding sites. In the healthy person, each red blood cell normally has hundreds of thousands of hemoglobin molecules. When blood passes through the lung alveoli, where oxygen concentration is the greatest, oxygen diffuses from the alveoli into red blood cells and binds to all those hemoglobin molecules. This oxygen-rich blood then goes to the left side of the heart and is pumped out into systemic circulation. In tissues away from the source of oxygen, hemoglobin unloads (dissociates) the oxygen molecules and delivers them to the tissues. Fig. 29-8 shows the oxygen-hemoglobin dissociation curve.
Tissue oxygen delivery through dissociation or unloading from hemoglobin is based on tissues’ need for oxygen. The curve in Fig. 29-8 shows that the rate of this unloading changes depending on how much oxygen is already in the tissues. When blood perfuses tissues in which the oxygen levels are high, as indicated in the upper right-hand corner of the figure, hemoglobin binds oxygen very tightly and little oxygen is unloaded or dissociated from the hemoglobin into the tissues. This prevents oxygen delivery from being wasted by unloading it where it is not needed. When blood perfuses tissues in which oxygen levels are very low, as indicated in the lower left-hand corner of Fig. 29-8, hemoglobin binds oxygen less tightly and will rapidly and easily unload its remaining oxygen to provide these tissues with needed oxygen. So, how rapidly and easily hemoglobin dissociates oxygen to the tissues changes depending on oxygen need. The S-shaped curve indicates that it is harder for oxygen to dissociate from hemoglobin in tissues that are well-oxygenated and much easier in tissues that are “starving” for oxygen.
The curve in Fig. 29-8 indicates that, on average, 50% of hemoglobin molecules have completely dissociated their oxygen molecules when blood perfuses tissues that have an oxygen tension (concentration) of 26 mm Hg. This is considered a “normal” point at which 50% of hemoglobin molecules are no longer saturated with oxygen.
Respiratory Changes Associated With Aging
The respiratory changes that occur with aging are described in Chart 29-1. Many additional respiratory changes in older patients result from heredity and a lifetime of exposure to environmental pollutants (e.g., cigarette smoke, bacteria, industrial fumes and irritants).
Chart 29-1 Nursing Focus on the Older Adult
Changes in the Respiratory System Related to Aging
| PHYSIOLOGIC CHANGE | NURSING INTERVENTIONS | RATIONALES |
|---|---|---|
| Alveoli | ||
| Alveolar surface area decreases. Diffusion capacity decreases. Elastic recoil decreases. Bronchioles and alveolar ducts dilate. Ability to cough decreases. Airways close early. | Encourage vigorous pulmonary hygiene (i.e., encourage patient to turn, cough, and deep breathe), and to use incentive spirometry, especially if he or she is confined to bed or has had surgery. | Potential for mechanical or infectious respiratory complications is increased in these situations. |
| Encourage upright position. | The upright position minimizes ventilation-perfusion mismatching. | |
| Lungs | ||
| Residual volume increases. Vital capacity decreases. Efficiency of oxygen and carbon dioxide exchange decreases. Elasticity decreases. | Include inspection, palpation, percussion, and auscultation in lung assessments. | Inspection, palpation, percussion, and auscultation are needed to detect normal age-related changes. |
| Help patient actively maintain health and fitness. | Health and fitness help keep losses in respiratory functioning to a minimum. | |
| Assess patient’s respirations for abnormal breathing patterns. | Periodic breathing patterns (e.g., Cheyne-Stokes) can occur. | |
| Encourage frequent oral hygiene. | Oral hygiene aids in the removal of secretions. | |
| Pharynx and Larynx | ||
| Muscles atrophy. Vocal cords become slack. Laryngeal muscles lose elasticity, and airways lose cartilage. | Have face-to-face conversations with patient when possible. | Patient’s voice may be soft and difficult to understand. |
| Pulmonary Vasculature | ||
| Vascular resistance to blood flow through pulmonary vascular system increases. Pulmonary capillary blood volume decreases. Risk for hypoxia increases. | Assess patient’s level of consciousness and cognition. | Patient can become confused during acute respiratory conditions. |
| Exercise Tolerance | ||
| Body’s response to hypoxia and hypercarbia decreases. | Assess for subtle manifestations of hypoxia. | Early assessment helps prevent complications. |
| Muscle Strength | ||
| Respiratory muscle strength, especially the diaphragm and the intercostals, decreases. | Encourage pulmonary hygiene, and help patient actively maintain health and fitness. | Regular pulmonary hygiene and overall fitness help maintain maximal functioning of the respiratory system and prevent illness. |
| Susceptibility to Infection | ||
| Effectiveness of the cilia decreases. Immunoglobulin A decreases. Alveolar macrophages are altered. | Encourage pulmonary hygiene, and help patient actively maintain health and fitness. | Regular pulmonary hygiene and overall fitness help maintain maximal functioning of the respiratory system and prevent illness. |
| Chest Wall | ||
| Anteroposterior diameter increases. Thorax becomes shorter. Progressive kyphoscoliosis occurs. Chest wall compliance (elasticity) decreases. Mobility may decrease. | Discuss the normal changes of aging. | Patients may be anxious because they must work harder to breathe. |
| Discuss the need for increased rest periods during exercise. | Older patients have less tolerance for exercise. | |
| Osteoporosis is possible. | Encourage adequate calcium intake (especially during a woman’s premenopause phase). | Calcium intake helps prevent osteoporosis by building bone in younger patients. |
Respiratory disease is a major cause of illness and chronic disability in older patients. Although respiratory function normally declines with age, there is usually no problem keeping pace with the demands of ordinary activity. The sedentary older adult, however, often feels breathless during exercise (Touhy & Jett, 2010).
Assessment methods
Patient History
Obtaining accurate information from the patient is important for identifying the type and severity of breathing problems. Chart 29-2 lists questions to ask patients (based on Gordon’s Functional Health Patterns) to assess the impact of pulmonary function.
Respiratory Assessment
Using Gordon’s Functional Health Patterns
Activity-Exercise Pattern
• Do you feel you have sufficient energy to perform tasks or routines that are required of you?
• Do you feel you have sufficient energy to do what you would like to do?
• Do you exercise? How often? For how long each time? What type(s) of exercise do you perform?
• What activities do you perform in your spare time?
• What is your ability to perform these tasks?
Based on Gordon, M. (2011). Manual of nursing diagnosis (12th ed.). Boston: Jones & Bartlett.
Ask patients about their respiratory history (Table 29-1), including smoking history, drug use, travel, and area of residence.
TABLE 29-1 IMPORTANT ASPECTS TO ASSESS IN A RESPIRATORY SYSTEM HISTORY
< div class='tao-gold-member'> Only gold members can continue reading. Log In or Register to continue
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|