Chapter 68 Assessment of the Renal/Urinary System
Safe and Effective Care Environment
1. Use Standard Precautions when handling urine specimens or examining the patient’s genitalia.
2. Determine whether the patient has risks for an allergic reaction to contrast dyes or a drug–contrast dye adverse interaction before testing procedures.
3. Verify that informed consent has been obtained and that the patient has a clear understanding of the potential risks before he or she undergoes invasive procedures to assess the kidneys and urinary function.
4. Examine individual patient factors contributing to safety risks.
Health Promotion and Maintenance
5. Teach all people about the importance of maintaining an adequate oral fluid intake.
6. Teach about or assist with cleansing of the perineum or urinary meatus after using the toilet and during daily bathing or showering.
7. Use language comfortable for the patient during assessment of the kidneys and urinary system.
8. Encourage the patient to express feelings or concerns about a change in kidney or bladder function.
9. Respect the patient’s dignity when performing kidney and urinary assessment.
10. Explain all diagnostic procedures, restrictions, and follow-up care to the patient scheduled for tests.
11. Briefly review the relevant anatomy and physiology of the kidney and urinary system.
12. Describe age-related changes in the kidney and urinary system.
13. Describe the correct techniques to use in physically assessing the kidney and urinary system.
14. Use laboratory data to distinguish between dehydration and kidney impairment.
15. Describe how to obtain a sterile urine specimen from a urinary catheter.
16. Coordinate nursing care for the patient during the first 24 hours after IV urography.
17. Coordinate nursing care for the patient during the first 24 hours after a kidney biopsy.
http://evolve.elsevier.com/Iggy/
Answer Key for NCLEX Examination Challenges and Decision-Making Challenges
Review Questions for the NCLEX® Examination
Anatomy and Physiology Review
Kidneys
Structure
Gross Anatomy
Normally, two kidneys are located behind the peritoneum, not really in the abdominal cavity, one on either side of the spine (Fig. 68-1). The adult kidney is 4 to 5 inches (10 to 13 cm) long, 2 to 3 inches (5 to 7 cm) wide, and about 1 inch (2.5 to 3 cm) thick. It weighs about 8 ounces (250 g). The left kidney is slightly longer and narrower than the right kidney. Larger-than-usual kidneys may indicate obstruction or polycystic disease. Smaller-than-usual kidneys may indicate chronic kidney disease (CKD).
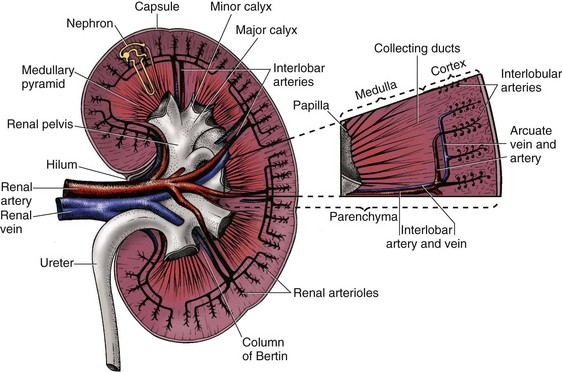
Several layers of tissue surround the kidney, providing protection and support. On the outer surface of the kidney is a layer of fibrous tissue called the capsule (Fig. 68-2). This capsule covers most of the kidney except the hilum, which is the area where the renal artery and nerve plexus enter and the renal vein and ureter exit. The renal capsule is surrounded by layers of fat and connective tissue.
Microscopic Anatomy
• The peritubular capillaries around the tubular part of the cortical nephrons
• The vasa recta around the tubular part of juxtamedullary nephrons
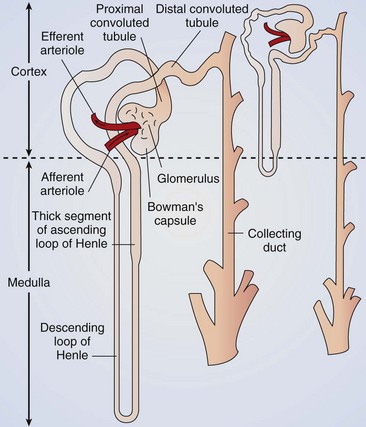
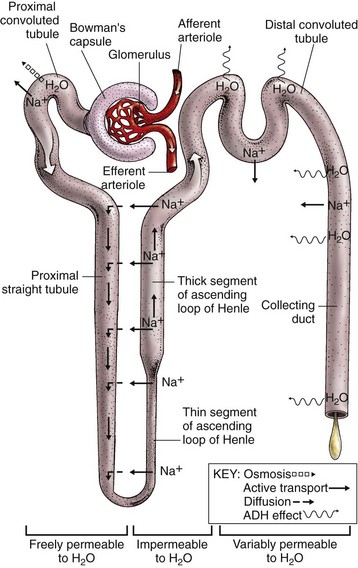
Each nephron is a tubelike structure with distinct parts (Fig. 68-3). The tube begins with Bowman’s capsule, a saclike structure that surrounds the glomerulus. The tubular tissue of Bowman’s capsule narrows into the proximal convoluted tubule (PCT). The PCT twists and turns, finally straightening into the descending limb of the loop of Henle. The descending loop of Henle dips in the direction of the medulla but forms a hairpin loop and comes back up into the cortex as the ascending loop of Henle.
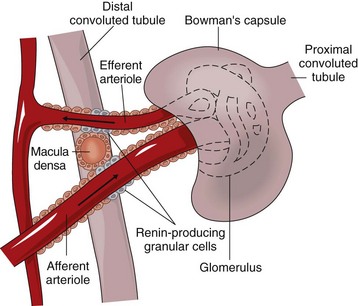
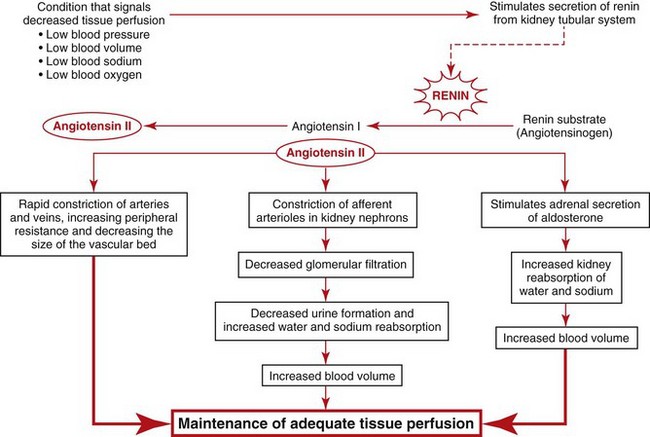
Special cells in the afferent arteriole, efferent arteriole, and DCT are known as the juxtaglomerular complex (Fig. 68-4). These specialized cells produce and store renin. Renin is a hormone that helps regulate blood flow, glomerular filtration rate (GFR), and blood pressure. Renin is secreted when sensing cells in the DCT (called the macula densa) sense changes in blood volume and pressure. The macula densa lies next to the renin-producing cells. Renin is produced when the macula densa cells sense that blood volume, blood pressure, or blood sodium level is low. Renin then converts renin substrate (angiotensinogen) into angiotensin I. This leads to a series of reactions that cause secretion of the hormone aldosterone (Fig. 68-5). Aldosterone increases kidney reabsorption of sodium and water, restoring blood pressure, blood volume, and blood sodium levels. It also promotes excretion of potassium. (See Chapter 13 for more discussion of the renin-angiotensin-aldosterone pathway.)
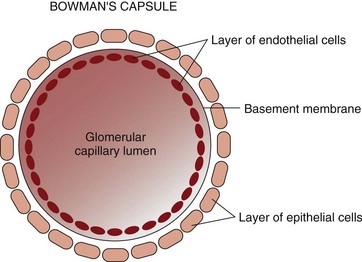
The glomerular capillary wall has three layers (Fig. 68-6): the endothelium, the basement membrane, and the epithelium. The endothelial and epithelial cells lining these capillaries are separated by pores that filter water and small particles from the blood into Bowman’s capsule. This fluid is called the “filtrate” or “early urine.”
Function
Regulatory Functions
The kidney processes that maintain fluid, electrolyte, and acid-base balance are glomerular filtration, tubular reabsorption, and tubular secretion. These processes use filtration, diffusion, active transport, and osmosis. (See Chapter 13 for a review of these actions.) Table 68-1 lists the functions of nephron tubules and blood vessels.
TABLE 68-1 VASCULAR AND TUBULAR COMPONENTS OF THE NEPHRON
| STRUCTURE | ANATOMIC FEATURES | PHYSIOLOGIC ASPECTS |
|---|---|---|
| Vascular Components | ||
| Afferent arteriole | Delivers arterial blood from the branches of the renal artery into the glomerulus | Autoregulation of renal blood flow via vasoconstriction or vasodilation |
| Renin-producing granular cells | ||
| Glomerulus | Capillary loops with thin, semipermeable membrane | Site of glomerular filtration |
| Glomerular filtration occurs when hydrostatic pressure (blood pressure) is greater than opposing forces (tubular filtrate and oncotic pressure) | ||
| Efferent arteriole | Delivers arterial blood from the glomerulus into the peritubular capillaries or the vasa recta | Autoregulation of renal blood flow via vasoconstriction or vasodilation |
| Renin-producing granular cells | ||
| Peritubular capillaries (PTCs) and vasa recta (VR) | PTCs: surround tubular components of cortical nephrons | Tubular reabsorption and tubular secretion allow movement of water and solutes to or from the tubules, interstitium, and blood |
| VR: surround tubular components of juxtamedullary nephrons | ||
| Tubular Components | ||
| Bowman’s capsule (BC) | Thin membranous sac surrounding  of the glomerulus of the glomerulus | Collects glomerular filtrate (GF) and funnels it into the tubule |
| Proximal convoluted tubule (PCT) | Evolves from and is continuous with Bowman’s capsule | Site for reabsorption of sodium, chloride, water, glucose, amino acids, potassium, calcium, bicarbonate, phosphate, and urea |
| Specialized cellular lining facilitates tubular reabsorption | ||
| Loop of Henle | Continues from PCT | Regulation of water balance |
| Juxtamedullary nephrons dip deep into the medulla | ||
| Permeable to water, urea, and sodium chloride | ||
| Descending limb (DL) | Continues from the loop of Henle | Regulation of water balance |
| Permeable to water, urea, and sodium chloride | ||
| Ascending limb (AL) | Emerges from DL as it turns and is redirected up toward the renal cortex | Potassium and magnesium reabsorption in the thick segment |
| Thin segment is impermeable to water | ||
| Distal convoluted tubule (DCT) | Evolves from AL and twists so the macula densa cells lie adjacent to the juxtaglomerular cells of afferent arteriole | Site of additional water and electrolyte reabsorption, including bicarbonate |
| Potassium and hydrogen secretion | ||
| Collecting ducts | Collect formed urine from several tubules and deliver it into the renal pelvis | Receptor sites for antidiuretic hormone regulation of water balance |
The tubules return about 99% of all filtered water back into the body (Fig. 68-7). Most water reabsorption occurs as the filtrate passes through the PCT. Water reabsorption continues as the filtrate flows down the descending loop of Henle. The thin and thick segments of the ascending loop of Henle are not permeable to water, and water reabsorption does not occur here.
Bicarbonate, calcium, and phosphate are mostly reabsorbed in the PCT. Bicarbonate reabsorption helps balance acids and maintain a normal blood pH. Blood levels of calcitonin and parathyroid hormone (PTH) (see Chapters 13 and 66) control calcium balance.
Action Alert
Hormonal Functions
The kidneys produce renin, prostaglandins, bradykinin, erythropoietin, and activated vitamin D (Table 68-2). Other kidney products, such as the kinins, change kidney blood flow and capillary permeability. The kidneys also help break down and excrete insulin.
TABLE 68-2 RENAL HORMONE PRODUCTION AND HORMONES INFLUENCING RENAL FUNCTION
| SITE | ACTION | |
|---|---|---|
| Renal Hormone Production | ||
| Renin | Renin-producing granular cells | Raises blood pressure as result of angiotensin (local vasoconstriction) and aldosterone (volume expansion) secretion |
| Prostaglandins | Kidney tissues | Regulate intrarenal blood flow by vasodilation or vasoconstriction |
| Bradykinins | Juxtaglomerular cells of the arterioles | Increase blood flow (vasodilation) and vascular permeability |
| Erythropoietin | Kidney parenchyma | Stimulates bone marrow to make red blood cells |
| Activated vitamin D | Kidney parenchyma | Promotes absorption of calcium in the GI tract |
| Hormones Influencing Kidney Function | ||
| Antidiuretic hormone (ADH, vasopressin) | Released from posterior pituitary | Makes DCT and CD permeable to water to maximize reabsorption and produce a concentrated urine |
| Aldosterone | Released from adrenal cortex | Promotes sodium reabsorption and potassium secretion in DCT and CD; water and chloride follow sodium movement |
| Natriuretic hormones | Cardiac atria, cardiac ventricle, brain | Cause tubular secretion of sodium |
CD, Collecting duct; DCT, distal convoluted tubule.
Renin release causes the production of angiotensin II through a series of steps (see Fig. 68-5). Angiotensin II increases systemic blood pressure through powerful blood vessel constricting effects and triggers the release of aldosterone from the adrenal glands. Aldosterone increases the reabsorption of sodium in the distal tubule of the nephron. Therefore more water is reabsorbed and blood pressure is increased because of increases in blood volume. When blood flow to the kidney is reduced, this system also regulates pressures in the nephron to prevent fluid loss and maintain circulating blood volume (see also Chapter 13).
Ureters
• In the upper third of the ureter, at the point at which the renal pelvis becomes the ureter, is a narrowing known as the ureteropelvic junction (UPJ).
• The ureter also narrows as it bends toward the abdominal wall (aortoiliac bend).
• Each ureter narrows at the point it enters the bladder; this point is called the ureterovesical junction (UVJ).
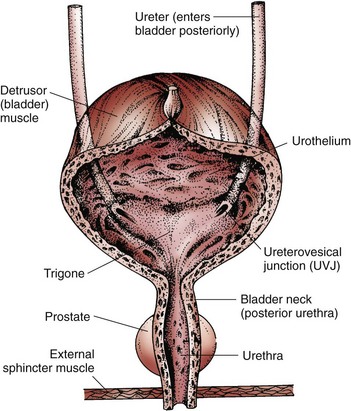
The ureter tunnels through bladder tissue for a short distance and then opens into the bladder at the trigone (Fig. 68-8).
Urinary Bladder
Structure
The urinary bladder is a muscular sac (see Fig. 68-8). The upper surface lies next to the peritoneal cavity. In men, the bladder is in front of the rectum. In women, it is in front of the vagina. The bladder lies directly behind the pubic bone.
Urethra
• The prostatic urethra, which extends from the bladder to the prostate gland
• The membranous urethra, which extends to the wall of the pelvic floor
• The cavernous urethra, which is external and extends through the length of the penis
Kidney and Urinary System Changes Associated with Aging
Kidney Changes
Kidney size and function decrease with aging (Chart 68-1). Blood flow to the kidney declines by about 10% per decade as blood vessels thicken. This means that blood flow to the kidney is not as adaptive in older adults compared with younger adults, leaving nephrons more vulnerable to damage during episodes of either hypotension or hypertension.
Chart 68-1 Nursing Focus on the Older Adult
Changes in the Renal/Urinary System Related to Aging
| PHYSIOLOGIC CHANGE | NURSING INTERVENTIONS | RATIONALES |
|---|---|---|
| Decreased glomerular filtration rate (GFR) | Monitor hydration status. | With aging, the ability of the kidneys to regulate water balance is decreased. |
| Ensure adequate fluid intake. | The kidneys are less able to conserve water when necessary. | |
| Administer potentially nephrotoxic agents or drugs carefully. | Dehydration results in decreased renal blood flow and increases the nephrotoxic potential of many agents. Acute or chronic kidney failure may result. | |
| Nocturia | Ensure adequate nighttime lighting and a hazard-free environment. | Nocturia may occur from decreased renal concentrating ability associated with aging. |
| Ensure the availability of a toilet, bedpan, or urinal. | The desire to maintain continence prompts people to seek the bathroom. Falls and injuries are common among older patients seeking bathroom facilities. | |
| Discourage excessive fluid intake for 2-4 hr before the patient retires for the evening. | Excessive fluid intake at night may increase nocturia. | |
| Evaluate drugs and timing. | Some drugs increase urine output. | |
| Decreased bladder capacity | Encourage the patient to use the toilet, bedpan, or urinal at least every 2 hr. | By emptying the bladder on a regular basis, urinary incontinence from overflow may be avoided. |
| Respond as soon as possible to the patient’s indication of the need to void. | A quick response may alleviate episodes of urinary stress incontinence. | |
| Weakened urinary sphincter muscles and shortened urethra in women | Provide thorough perineal care after each voiding. | The shortened urethra increases the potential for bladder infections. |
| Good perineal hygiene may prevent skin irritations and urinary tract infection (UTI). | ||
| Tendency to retain urine | Observe the patient for urinary retention (e.g., bladder distention) or urinary tract infection (e.g., dysuria, foul odor, confusion). Provide privacy, assistance, and voiding stimulants such as warm water over the perineum as needed. Evaluate drugs for possible contribution to retention. | Urinary stasis may result in a UTI. UTIs may become bloodstream infections, resulting in urosepsis or septic shock. |
| Nursing interventions can help initiate voiding. | ||
| Anticholinergic drugs promote urinary retention. |
Urinary Changes
African Americans have more rapid age-related decreases in GFR than do white people (Brenner, 2008). Kidney excretion of sodium is less effective in hypertensive African Americans who have high sodium intake, and the kidneys have about 20% less blood flow as a result of anatomic changes in small renal vessels and intrarenal responses to renin. Thus African-American patients are at greater risk for kidney failure than are white patients. Yearly health examinations should include urinalysis and checking for the presence of microalbuminuria.
Assessment Methods
Patient History
One way to assess kidney and urologic function is to use Gordon’s Functional Health Patterns (Gordon, 2011). The patterns most related to the renal system are Nutritional/Metabolic and Elimination (Chart 68-2).
Renal/Urinary Assessment
Using Gordon’s Functional Health Patterns
Nutritional/Metabolic Pattern
• What is your typical daily food intake? Describe a day’s meals, snacks, and vitamins.
• How much salt do you typically add to your food? Do you use salt substitutes?
• Have you experienced any nausea or vomiting?
• What is your typical daily fluid intake?
• What types of fluids do you drink (water, juices, soft drinks, coffee, tea)?
• How much fluid do you drink each day?
• Have you had any recent change in your weight? Weight gain? Weight loss? How much?
• Have you noticed a change in the tightness of your rings or shoes? Tighter? Looser?
• Have you noticed any skin changes lately? More dry? Less dry? Itchy?
Elimination Pattern
Based on Gordon, M. (2011). Manual of nursing diagnosis (12th ed.). New York: Jones & Bartlett.
• Chemical or environmental toxin exposure in occupational or other settings
• Recent travel to geographic regions that pose infectious disease risks
The language used by patients may be different from that used by the health care professional. Anatomic or medical terms may have no meaning for the patient (Table 68-3). When obtaining a history, listen to and explore the terms used by the patient. By using the patient’s own terms, you may help him or her provide a more complete description of the problem. This technique may increase the amount of information obtained and decrease the patient’s discomfort when discussing bodily functions.
TABLE 68-3 COMMONLY USED RENAL AND URINARY TERMS
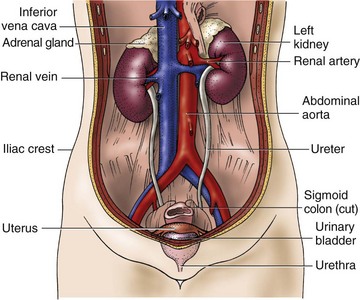
 inch (1.25 cm) in diameter and about 12 to 18 inches (30 to 45 cm) in length. The diameter of the ureter narrows in three areas:
inch (1.25 cm) in diameter and about 12 to 18 inches (30 to 45 cm) in length. The diameter of the ureter narrows in three areas: