6 Assessment of risk and the medical patient
• To understand why risk assessments are important for medical patients
• To identify the risk assessments undertaken in the placement learning pathways throughout the patient journey
• To begin to understand the nursing actions taken when a risk is identified to ensure patient safety
• To understand the term ‘vulnerable adult’ and be able to identify patients who are vulnerable
• To understand safeguarding adult procedures and the use of the Mental Capacity Act in your placement area
• To understand what constitutes abuse
• To understand the needs of a patient with learning disabilities in your placement area
Introduction
Within your curriculum you will have a number of competencies and/or learning outcomes around risk assessment and safeguarding. This chapter aims to help you identify the essential knowledge and skills required to meet these learning outcomes and be able to identify opportunities within your medical placement to do this. The Essential Skills Clusters (Nursing and Midwifery Council (NMC) 2010a) include competencies around risk assessment and safeguarding vulnerable adults, organisational aspects of care, infection prevention and control and nutrition and fluid management.
The NMC (2010b) Domain ‘Professional Values’ is relevant to risk assessment and safeguarding. For example, the competencies include the following:
• You must understand and apply current laws relating to the care of adults and, where appropriate, children and young people. This includes safeguarding vulnerable individuals, including during end of life care.
• You must practise in a holistic, non-judgemental, caring and sensitive manner that supports social inclusion and recognises and respects diversity and the beliefs, rights and wishes of individuals of all ages, groups and communities. Where necessary, you must challenge inequality, discrimination or exclusion from access to care.
• You must support and promote the health, wellbeing, comfort, dignity and rights of individuals, groups, communities and populations whose lives are affected by transition, disability, mental capacity, ill health, distress, disease, ageing or death. You must understand how these can affect the care and health promotion of people from different communities.
• You must work closely with individuals, groups and carers, using a range of skills to carry out comprehensive, systematic and holistic assessments. These must take into account current and previous physical, social, cultural, psychological, spiritual, genetic and environmental factors that may be relevant to the individual and their families.
• You must know the limitations and known hazards in the use of a range of technical nursing skills, activities, interventions, treatments, medical devices and equipment. This must include safe application and evaluation of the outcome in a variety of care settings, including complex, technical, diverse environments, to provide effective person-centred care for people of all ages and backgrounds. Interventions will include safe medicines management, wound management, pain relief and infection prevention and control. You must report any concerns through appropriate channels and modify the plan of care to maintain safe practice.
• You must know when a person of any age is at risk and in a vulnerable situation in any environment and in need of extra support and protection. You must also act to safeguard them against abuse of any kind.
What is risk assessment?
It is also worth asking whether the risk assessment is locally driven or a nationally driven assessment. For example, is it linked to national best practice guidelines such as those developed by the National Institute for Health and Clinical Excellence: http://www.nice.org.uk/ (accessed July 2011)?
Examples of risk assessment tools
• Falls risk assessment, e.g. Morse (1997), STRATiFY (Oliver et al 1998).
• Bed rail assessment, e.g. National Patient Safety Agency (NPSA; 2007a) tools.
• Pressure ulcer risk assessment, e.g. Waterlow (2005), Norton et al (1962).
• Malnutrition risk assessment, e.g. Malnutrition Universal Screening Tool (British Association for Parenteral and Enteral Nutrition (BAPEN) 2008).
• Infection control, e.g. Visual Infusion Phlebitis score (Jackson 1998) to detect signs of phlebitis.
• Early warning scores to detect patient deterioration, e.g. Modified Early Warning score (Stenhouse et al 1999).
Different risk assessment tools will apply at different stages of your patients’ journey. Some of them will be common across all stages of the journey (Box 6.1).
Box 6.1 Examples of risk assessment across the patient journey
How are risk assessment tools developed?
It is important that you understand why certain factors put some people at an increased risk. Spending some time looking at a tool and working out how risk factors are determined is a useful exercise. Look at the Waterlow score (Waterlow 2005) in Figure 6.1 for assessing risk of developing pressure ulcers. Think about each category of risk and why such factors contribute to the development of pressure ulcers – you will need to think back to anatomy and physiology. Table 6.1 describes what each of the categories for risk within the Waterlow score mean.
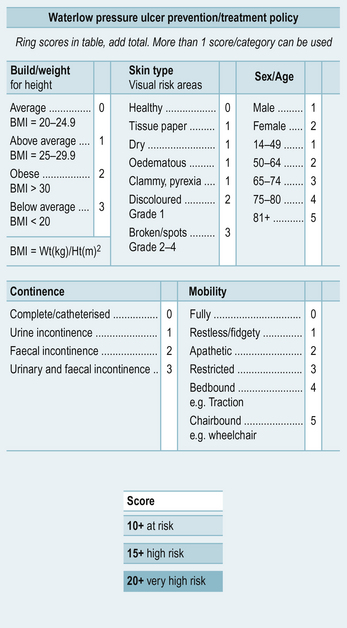
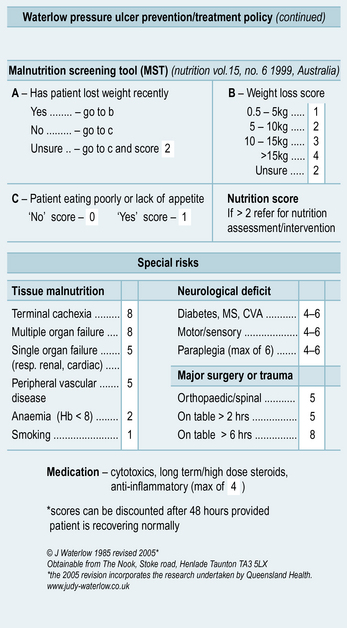
Fig 6.1 Waterlow score
(Printed with permission of Judy Waterlow MBE SRN RCNT: www.judy-waterlow.co.uk)
Table 6.1 The categories for risk within the Waterlow score
| Risk factor | How it contributes to pressure ulcer development |
|---|---|
| Build/weight for height | Being overweight restricts your mobility and consequently your ability to relieve the pressure on parts of your body when sitting or lying down. Being underweight reduces the subcutaneous fat that protects your bony prominences from increased pressure |
| Skin type | If skin is dry it is much more likely to crack and damage easily. Tissue paper skin is thin and more easily damaged. Skin that is stretched over oedematous areas is also thinner and more easily damaged. Oedema will also reduce the blood supply to the skin surface. Discoloration is a sign that damage has already occurred. Skin that is clammy or damp is more susceptible to friction and shearing forces |
| Sex/age | Skin loses its elasticity as it ages and a reduction in blood supply to the skin surface means that it will take longer to heal |
| Continence | Wet and soiled skin from incontinence can become easily excoriated, increasing risk of skin breakdown. It also makes the skin more susceptible to friction and shearing forces |
| Mobility | The less able a person is to move, the less able they are to relieve pressure when sitting or lying down |
| Tissue malnutrition | There are many conditions that contribute to a reduced perfusion and blood flow to tissues and reduced overall mobility of the patient. These will all increase the risk of skin breakdown and delay healing |
| Neurological deficit | A condition that results in a sensory deficit will mean the person is unable to fully feel pressure or pain and therefore will not change position to reduce pressure |
| Major surgery or trauma | The prolonged period of immobility associated with major surgery or trauma increases the risk of pressure damage |
| Medication | Medication that reduces the body’s own inflammatory response will affect the skin’s ability to heal |
| Nutrition | Being underweight, having significant weight loss and a poor appetite all contribute to an increased risk of acute illness and immobility and a reduced ability of the skin to heal |
The popularity of risk assessment tools also changes and new evidence may show that some well used tools are not as useful as they have been. Examples of this are falls risk assessment tools. Recent evidence has shown that they are not absolutely necessary in the prevention of falls for patients in hospital and that an assessment of modified risk factors should always be carried out with or without a numerical risk assessment (NPSA 2007b).
You may have considered that Mrs Kalra(see case history 6.1) would need a nutritional risk assessment as she is not eating and drinking well at present. As her mobility is reduced, she would require a manual handling risk assessment to determine the safest way for staff to help her mobilise, reducing the risk of injury both to Mrs Kalra and nursing staff. She may also be at risk of falls due to her confusion, dehydration and poor mobility so a falls risk assessment would be necessary. She already has a grade 2 pressure ulcer and her reduced mobility and oral intake will put her at risk of developing further pressure ulcers, so a pressure ulcer risk assessment would be required to help guide your management of her pressure ulcer risk. She is about to commence intravenous fluids, so her intravenous cannula site would require regular assessment for early detection of phlebitis or other complications.




















