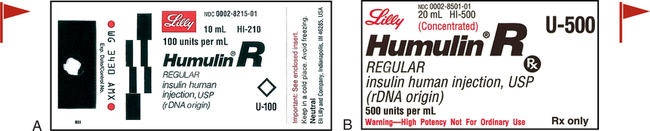
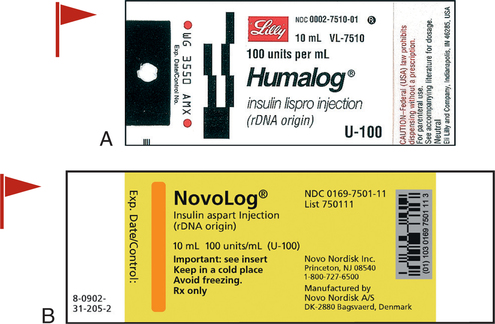
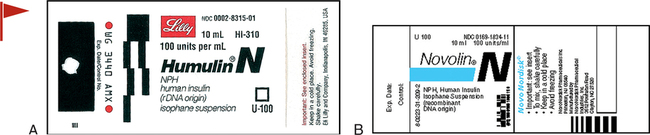
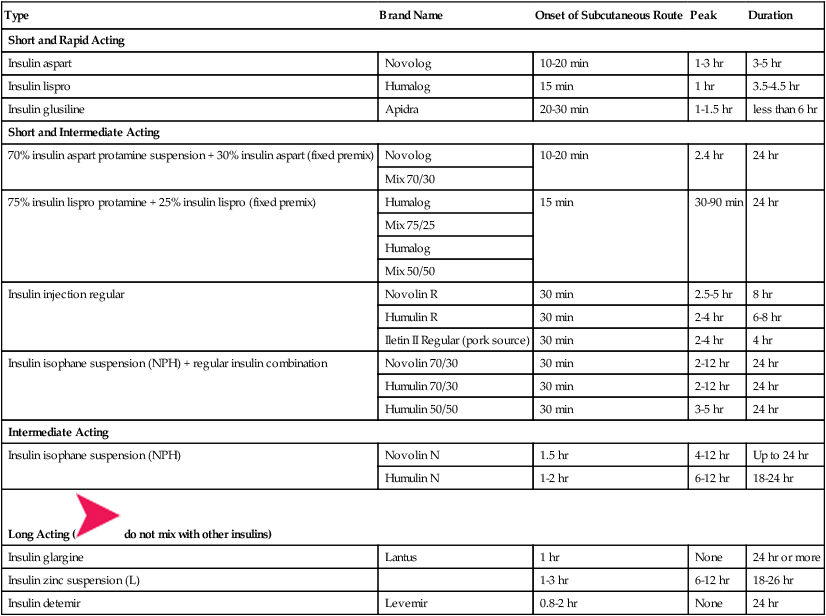
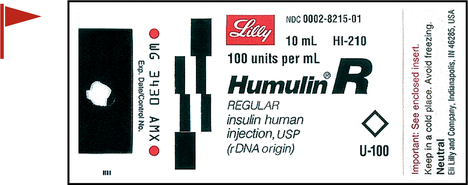
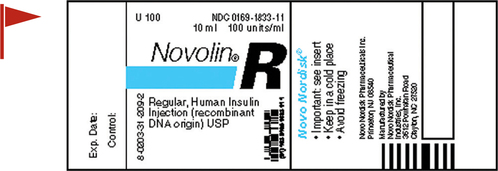
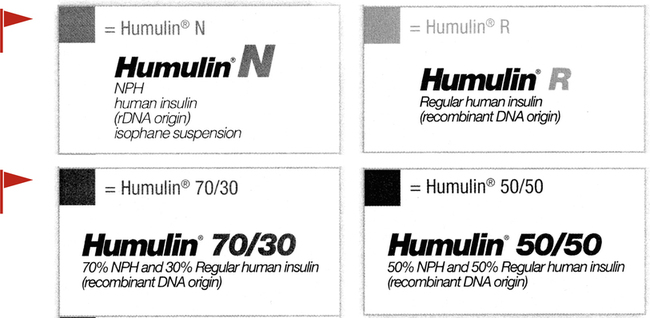
• Define terms related to tests and treatment for patients receiving medications for type 1 and type 2 diabetes. • Identify risks of look-alike generic oral antidiabetic products. • Contrast the various insulin products by onset of activity. • Calculate and titrate subcutaneous and IV insulin dosages based on blood glucose levels. • Evaluate blood glucose levels for prescribed insulin administration. • Select the appropriate syringe and measure syringe doses for subcutaneous insulin administration. • Identify the most common adverse effect of insulin therapy. • Define hypoglycemia and hyperglycemia. • Identify causes of, risks of, and nutrients needed for hypoglycemia. • Identify critical patient safety issues related to antidiabetic medications and blood glucose levels. Measuring an ordered insulin dose in a syringe for subcutaneous administration is a basic skill that does not require math. However, IV insulin administration does require math calculations. To administer antidiabetic agents safely, the nurse must understand frequently encountered terms, know how to interpret orders and labels, differentiate blood glucose laboratory levels, distinguish the various pharmacological products ordered for treatment, identify manifestations of hypo- and hyperglycemia, understand emergency treatment for those manifestations, and know when to withhold medication and seek further orders. Insulin is a high-alert medication, meaning that it has higher than average potential to cause harm if used in error.* This chapter focuses on basic concepts related to safe administration of insulin. • It is supplied in two concentrations: U-100 (100 units per mL) and U-500 (500 units per mL; Figure 11-1). • Insulin types are related to the product source as well as to the onset and duration of action. Recombinant DNA (rDNA) insulin, a highly purified version of human insulin, is similar in structure and function to human insulin. • Insulin is most often prescribed and administered subcutaneously. The IV route is reserved for specific acute-care situations. Examine the insulin activity chart in Table 11-1. Insulin fixed-combination mixes are supplied for patients who experience patterns of mealtime elevations. TABLE 11-1 Insulin Activity Chart for Subcutaneous Administration, in Order of Activity Onset* 1. What are the five column headings in Table 11-1 that reveal key pieces of information that the nurse must understand about each type of insulin? _____________________________________________ 2. Which type of insulin does not have a peak? 1. What is a basal dose of insulin? _____________________________________________ 2. What are two reasons that bolus doses would be added to basal doses? Take a few minutes to examine the insulin product labels and identify the following: • Concentration: U-100 or U-500 (U-500 rarely ordered) • Storage of insulin products, opened and unopened, is controversial. Some say refrigerate all. Others say current bottle can be at room temperature and unopened bottles must be refrigerated. Read the product insert and label information for each bottle used regarding room temperature storage and refrigeration storage and respective expiration dates. The nurse writes the date opened on the label and discards the bottle according to the manufacturer guidelines, usually a month. Insulin may not be effective after expiration dates of 28 days. There are several types and brands of short or rapid-acting insulins on the market. Short- and rapid-acting insulins are administered to treat a current blood glucose elevation or an anticipated elevation in the near future, such as after the next meal. Figures 11-2 to 11-5 illustrate product labels of various short-acting insulins. Humalog and Novolog insulin are to be given 10 to 15 minutes before a meal or with the meal, whereas Humulin R and Novolin R must be given 30 minutes before a meal (see Figures 11-2 to 11-4). 1. What does U-100 on the label of the insulin vial mean? _____________________________________________ 2. What is the most common adverse effect of insulin therapy? 1. What is the difference among each of these four types of Humulin insulin? Which are fast acting, intermediate, or both? _____________________________________________ 2. When reading two different numbers on the mixes, which number is the fast acting: the first or the second? 1. What would be expected to happen to the patient’s blood sugar levels if Humulin R, Novolin R, insulin lispro, or insulin aspart were given and the meal was delayed?
Antidiabetic Agents
Introduction
![]() If blood glucose levels are reported by a laboratory in millimoles per liter, multiply by 18 to convert to milligrams per deciliter. Divide milligrams per deciliter by 18 to obtain the equivalent millimoles per liter.
If blood glucose levels are reported by a laboratory in millimoles per liter, multiply by 18 to convert to milligrams per deciliter. Divide milligrams per deciliter by 18 to obtain the equivalent millimoles per liter.
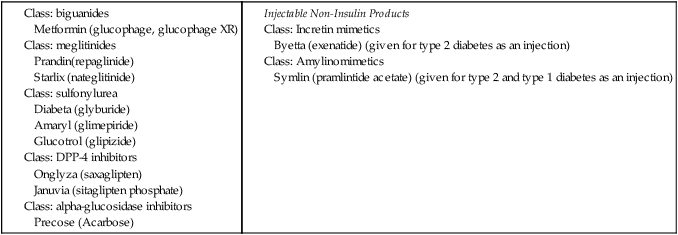
Oral and Injectable Non-Insulin Antidiabetic Agents
![]() Note carefully the similarities of generic names. Confusion of look-alike drug names has resulted in medication errors.
Note carefully the similarities of generic names. Confusion of look-alike drug names has resulted in medication errors.

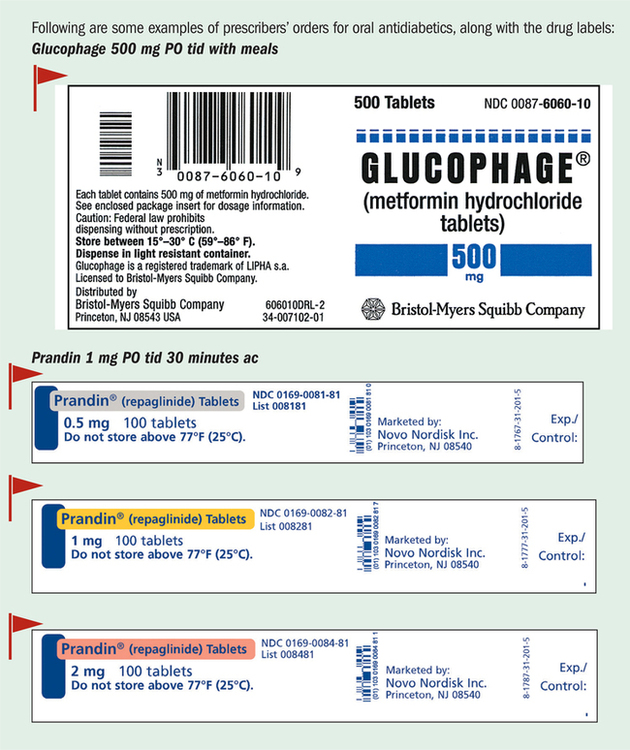
![]() Match the prescriber’s order, drug name, drug dose, and labels carefully. Do not try to guess the product contents from the name. The math is simple for the oral medications. The doses are available as ordered or in multiples of the amount ordered. They must be given at the prescribed time to control potential mealtime-generated elevations of glucose levels.
Match the prescriber’s order, drug name, drug dose, and labels carefully. Do not try to guess the product contents from the name. The math is simple for the oral medications. The doses are available as ordered or in multiples of the amount ordered. They must be given at the prescribed time to control potential mealtime-generated elevations of glucose levels.
Parenteral Antidiabetic Agents: Insulin Products
![]() Do not confuse U-100 with the total amount in the vial. U-100 refers to the concentration per milliliter (100 units per mL).
Do not confuse U-100 with the total amount in the vial. U-100 refers to the concentration per milliliter (100 units per mL).
![]() The most common adverse effect of insulin therapy is hypoglycemia.
The most common adverse effect of insulin therapy is hypoglycemia.
![]() Spell out “units” even though the abbreviation U may be seen in some orders and preprinted MARs. It can be mistaken for zero and is on the “Do Not Use” list of the TJC (p. 101).
Spell out “units” even though the abbreviation U may be seen in some orders and preprinted MARs. It can be mistaken for zero and is on the “Do Not Use” list of the TJC (p. 101).
![]() Warning: Insulin activity varies among individuals. Monitor blood glucose levels closely.
Warning: Insulin activity varies among individuals. Monitor blood glucose levels closely.
![]() Prescribed timing of insulin administration and timing of meals are linked to the time of onset of the insulin activity. Hypoglycemic reactions may occur at any time, but insulin onset and peak activity times warrant close observation for potential hypoglycemic reactions.
Prescribed timing of insulin administration and timing of meals are linked to the time of onset of the insulin activity. Hypoglycemic reactions may occur at any time, but insulin onset and peak activity times warrant close observation for potential hypoglycemic reactions.
![]() Consult manufacturer literature re: mixing with other insulins and oral antidiabetic products. There are important differences and interactions among the products.
Consult manufacturer literature re: mixing with other insulins and oral antidiabetic products. There are important differences and interactions among the products.
Type
Brand Name
Onset of Subcutaneous Route
Peak
Duration
Short and Rapid Acting
Insulin aspart
Novolog
10-20 min
1-3 hr
3-5 hr
Insulin lispro
Humalog
15 min
1 hr
3.5-4.5 hr
Insulin glusiline
Apidra
20-30 min
1-1.5 hr
less than 6 hr
Short and Intermediate Acting
70% insulin aspart protamine suspension + 30% insulin aspart (fixed premix)
Novolog
10-20 min
2.4 hr
24 hr
Mix 70/30
75% insulin lispro protamine + 25% insulin lispro (fixed premix)
Humalog
15 min
30-90 min
24 hr
Mix 75/25
Humalog
Mix 50/50
Insulin injection regular
Novolin R
30 min
2.5-5 hr
8 hr
Humulin R
30 min
2-4 hr
6-8 hr
Iletin II Regular (pork source)
30 min
2-4 hr
4 hr
Insulin isophane suspension (NPH) + regular insulin combination
Novolin 70/30
30 min
2-12 hr
24 hr
Humulin 70/30
30 min
2-12 hr
24 hr
Humulin 50/50
30 min
3-5 hr
24 hr
Intermediate Acting
Insulin isophane suspension (NPH)
Novolin N
1.5 hr
4-12 hr
Up to 24 hr
Humulin N
1-2 hr
6-12 hr
18-24 hr
Long Acting ( ![]() do not mix with other insulins)
do not mix with other insulins)
Insulin glargine
Lantus
1 hr
None
24 hr or more
Insulin zinc suspension (L)
1-3 hr
6-12 hr
18-26 hr
Insulin detemir
Levemir
0.8-2 hr
None
24 hr
Insulin Labels
Short- and Rapid-Acting Insulins
![]() If there is any chance that mealtime may be delayed, such as might occur in a hospital, do not give Humalog or Novolog until the meal arrives.
If there is any chance that mealtime may be delayed, such as might occur in a hospital, do not give Humalog or Novolog until the meal arrives.
![]() Avoid giving diet beverages or artificially sweetened foods, such as sugar alcohols and aspartame, for suspected hypoglycemic reactions. Follow prescriber and agency policies for insulin reactions. Dextrose (glucose) is the ingredient needed to raise the blood glucose level promptly. Dextrose administration is usually followed by a complex carbohydrate-containing meal to sustain a higher blood glucose level.
Avoid giving diet beverages or artificially sweetened foods, such as sugar alcohols and aspartame, for suspected hypoglycemic reactions. Follow prescriber and agency policies for insulin reactions. Dextrose (glucose) is the ingredient needed to raise the blood glucose level promptly. Dextrose administration is usually followed by a complex carbohydrate-containing meal to sustain a higher blood glucose level.
Nurse Key
Fastest Nurse Insight Engine
Get Clinical Tree app for offline access