CHAPTER 13
Aneurysmal Disease
Victoria R. Latessa
Anne Aquila
OBJECTIVES
1. Describe the anatomy and physiology relevant to aortic aneurysms and aneurysmal disease.
2. List appropriate diagnostic tests relevant to the diagnosis of aneurysmal disease.
3. Discuss the appropriate medical and surgical interventions relevant to aneurysmal disease.
4. Identify the nursing implications relevant to aneurysmal disease.
Introduction/Overview
The Ad hoc Committee of the Society for Vascular Surgery and International Society for Cardiovascular Surgery defines an aneurysm as a permanent localized dilation of an artery; an increase in diameter of greater than 50% or 1.5 times its normal diameter, normal diameter being determined by age, sex, and blood pressure (Johnston et al., 1991). Abdominal aortic aneurysm (AAA) is present in more than 5% of older men who have smoked. Aortic aneurysms constitute the 14th leading cause of death in the United States and the 10th leading cause of death in older men, who are the principal victims (Lederle, 2009).
Statistical data show that there is a 1% per year rupture rate for AAAs with a maximal diameter of less than 5.5 cm. The 1-year incidence of probable rupture for aneurysms between 5.5 and 5.9 cm was 9.4%, and there was a 10.2% rupture rate for aneurysms of 6 to 6.9 cm. Aneurysms greater than 7 cm had a 6-month rupture rate of 32.5%. These data indicate that due to the low incidence of rupture, physicians can recommend close observation of AAAs less than 5.5 cm. Aneurysms between 5.5 and 6.9 cm should be repaired promptly and those greater than 7 cm in diameter require urgent repair (Pappas, 2002). These are general recommendations that do not take into account the threshold for rupture in women that may be closer to 5 cm as opposed to men at 6 cm (Hannawa, Elias, & Upchurch, 2009).
A ruptured AAA is a catastrophic event. Overall, mortality of AAA rupture is 71% to 77% which includes all out-of-hospital and in-hospital deaths as compared to 2% to 6% for elective open surgical repair (Fillinger, 2010).
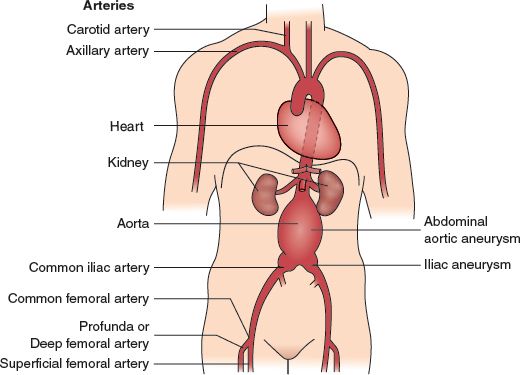
FIGURE 13.1 Aneurysms of some of the abdominal arteries.
 I. Aortic Anatomy and Aneurysm Location (see Fig. 13-1)
I. Aortic Anatomy and Aneurysm Location (see Fig. 13-1)
A. Aorta Begins at the Aortic Valve, ascends in the anterior mediastinum, arches posteriorly, descends in the posterior mediastinum, and traverses the retroperitoneum to end at the bifurcation into the common iliac arteries (Matsumura, 2004).
B. It is Posteriorly Situated in the chest and abdomen and is considered a posterior mediastinal and retroperitoneal structure once past the aortic arch.
C. The First Branches of the aorta are the left and right coronary arteries that feed the myocardium.
D. The Arch Vessels include the innominate artery that branches into the right subclavian and right common carotid arteries and the left common carotid artery and left subclavian artery.
E. The Descending Aorta gives off intercostal branches, some of which (usually in the T9 to L1 area) anastomose with the critical artery of Adamkiewicz, which feeds the spinal cord.
F. Abdominal Branches of the aorta include the celiac artery, the superior mesenteric artery (SMA), renal arteries, and the inferior mesenteric artery (IMA).
G. At the Level of the Umbilicus, the aorta divides into the common iliac arteries.
H. In the Pelvis, the common iliac arteries bifurcate into the external and internal iliac arteries.
I. The External Iliac Artery continues under the inguinal ligament and becomes the common femoral artery.
J. Adult’s Aorta normally measures approximately 2 cm (3/4”) in diameter at the celiac axis level, narrowing as it nears the aortic bifurcation.
K. Twelve Percent of aneurysms occur in the thoracoabdominal aorta.
1. Involves the segment of the aorta where the celiac axis, SMA, and renal arteries arise
2. Extent of aortic involvement for thoracoabdominal aortic aneurysms based upon Crawford Classification (see Fig. 13-2)
a. Type I: proximal descending thoracic aorta (DTA) to upper abdominal aorta
b. Type II: proximal TA to below renal arteries
c. Type III: distal DTA and abdominal aorta
d. Type IV: suprarenal and infrarenal
L. Eighty Percent of Aneurysms Occur in the Infrarenal Abdominal Aorta (Lederle, 2009; O’Connor, 2013).
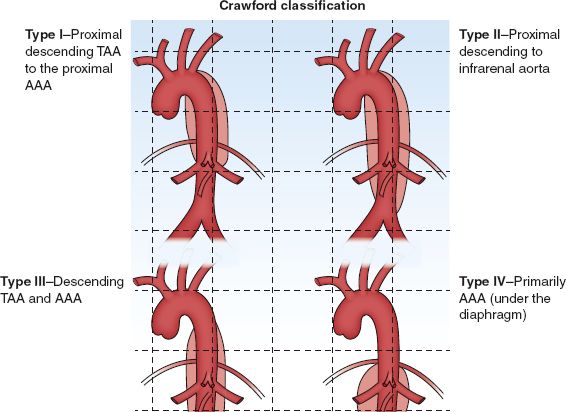
FIGURE 13.2 Crawford classification.
 II. Pathophysiology
II. Pathophysiology
A. Arteriosclerosis/Atherosclerosis: Plays a role in the development of most aneurysms (Cohen, 1990; Lawrence & Rigbirg, 2010; Lovell & Harris, 1991).
1. Traditional views held that most aneurysms were caused by degenerative atherosclerotic disease.
2. Atherosclerotic lesions weaken arterial wall rendering it brittle and susceptible to thinning.
B. Genetic Predisposition to Aneurysm Development
1. Clinical observations and biochemical data suggest that atherosclerosis/arteriosclerosis may not be the unique pathogenic factor of aneurysmal disease.
2. Some studies suggest that genetic predisposition is isolated to a single dominant gene with low penetrance that increases with age (Majumder, Jean, Ferrell, Webster, & Steed, 1991).
3. There may be a genetic predisposition to their development—alteration in systemic connective tissue metabolism (Anderson, 1994; Cohen, 1990, Curci, Baxter, & Thompson, 2005; Greenberg, Messina, & Thompson, 2000; Reilly & Tilson, 1989; Tilson, 1990).
4. Data over the past 20 years have revealed:
a. Presence of matrix metalloproteins (MMPs), a family of enzymes involved in breaking down elastin and collagen (Curci, Lee, & Thompson, 2001)
b. Chronic increase in aortic elastin breakdown brings about weakening of the wall and aneurysm dilation
c. Current theories suggest a spectrum of inflammation with all AAA (Lawrence & Rigbirg, 2010)
d. Cigarette smoking has major effect on enzyme activity—increasing serum elastase activity
e. Definite familial tendency; 15% to 25% of patients undergoing AAA repair have a first-degree relative with clinically apparent AAA (Curci et al., 2005; Lawrence & Rigbirg, 2010)
C. Aneurysmal Growth
1. Aneurysm thought to grow according to law of Laplace: tension = pressure × radius (T = P × r). With increasing pressure on the aortic wall or increase in wall radius, the wall tension becomes close to that of the tensile strength of collagen, resulting in rupture with any local wall weakness (Cohen, 1990).
2. Size of an aneurysm is the most important risk factor that determines risk of rupture, pressure (Goldstone, 2002; U.S. Preventive Services Task Force, 2005).
3. Sudden rupture of AAA accounts for approximately 15,000 deaths in the United States (Goldstone, 2002).
 III. Etiology or Precipitating Factors (Cronenwett, Krupski, & Rutherford, 2000)
III. Etiology or Precipitating Factors (Cronenwett, Krupski, & Rutherford, 2000)
A. Degenerative
1. Atherosclerosis
2. Medial necrosis
3. Fibrodysplasia
4. Pregnancy related
5. Site of graft anastomosis
B. Inflammatory
1. Arteritis
2. Bacterial/fungal/viral infections
C. Mechanical
1. Traumatic
2. Poststenotic
3. Anastomotic
4. Prosthetic
D. Congenital
1. Born with abnormal dilations of arteries
2. Marfan syndrome
3. Ehlers–Danlos syndrome
 IV. Assessment
IV. Assessment
A. Risk Factors
1. Gender
a. Males three to six times more likely to have AAA than females
b. Occurs in of every 20 elderly men (Lederle, 2003)
c. Males have a 40% higher likelihood of presenting with ruptured aneurysm and are older than females for intact and ruptured AAA (Fillinger, 2010)
d. Women more likely to fare worse, whether open repair of EVAR, elective surgery, or repair with rupture (Hannawa et al., 2009; Schermerhorn & Giles, 2010)
2. Age
a. Prevalence of AAA increases with age
b. Highest percent of patients with AAA between 70 and 80 years of age (Schermerhorn & Giles, 2010)
c. Ninety-five percent of patients dying with rupture AAA are older than 65 years (Singh, Bonaa, Jacobsen, Bjork, & Solberg, 2001)
3. Smoking
a. Smokers three to five times more likely than nonsmokers
b. Length of time smoking more important than amount
c. By-products of smoking are destructive to aortic wall (Lederle, 2003)
4. Hypertension
a. Accelerates the degeneration of the aortic wall
b. Higher intra-aortic pressure increases risk of rupture
5. Family history
a. AAA not an inherited disorder
b. Evidence of familial clustering
c. Risk of AAA for brother of patient treated for AAA is increased fourfold (Powell, 2003)
6. Aneurysm elsewhere
a. Patient with unilateral popliteal artery aneurysm has 8% chance of having AAA
b. Patient with bilateral popliteal artery aneurysms has 30% chance of AAA
c. Patient with AAA has 12% chance of thoracic aortic aneurysm (Goldstone, 2002)
7. Known history of connective tissue disease
a. Ehlers–Danlos
b. Marfan
8. Primary prevention
a. No biochemical markers available to detect early changes in matrix of aortic wall
b. Screen those at high risk for developing AAA with ultrasound (U.S. Preventive Services Task Force, 2005)
1) One time screening for all males 60 to 75 years old who have ever smoked or 55 years old for those with family history of AAA
2) Ultrasound screening for women 65 years and older who have smoked or have positive family history of AAA (Chaikof et al., 2009)
3) Screen men 60 to 85 years of age or older who are either the sibling or offspring of patients with AAA (Hirsch et al., 2006)
B. Patient History
1. Subjective findings
a. Asymptomatic
1) Usually found incidentally during evaluation for chronic back pain or kidney stones
2) Rarely symptomatic unless there is rapid expansion or rupture (Cronenwett et al., 2000; Lederle, 2009; Winterstein & Baxter, 2000).
3) Can have diffuse mid-abdominal pain caused by compression of adjacent structures
4) AAA rupture may have back, flank, or groin pain and tenderness
5) Gastrointestinal (GI) dysfunction, urinary dysfunction, syncope, hypotension, and shock (Lederle, 2009)
b. Past health history—Broad in scope but focused on vascular risk factors such as hypertension, angina, myocardial infarction, peripheral artery disease, transient ischemic attack, DM, dyslipidemias, chronic obstructive pulmonary disease (COPD)
c. Family history
1) Vascular, heart disease, hypertension
2) Aneurysmal disease
d. Social history—Cigarette smoking; a history of heavy tobacco use or family history of AAA should heighten awareness in older persons particularly men (Lederle, 2009)
e. Medication history—All current therapeutic drugs
2. Objective findings on physical examination
a. Inspection
1) Pulsatile abdomen
2) Mottling, cyanosis may be present with rupture
3) ‘‘Blue toes’’ may be evident with distal embolization (Fahey, 2004)
b. Palpation
1) Widened aortic pulsation or pulsatile abdominal mass at or above the umbilicus usually at least 5 cm to be reliably identified except in a very thin person
2) Has only moderate overall sensitivity for detecting AAA but appears to be highly sensitive for diagnosis of AAA large enough to warrant elective intervention in patients who do not have a large girth (Fink et al., 2000)
3) Check for associated femoral and popliteal aneurysms
3. Auscultation—Abdominal bruit rarely present
 V. Considerations Across the Life Span
V. Considerations Across the Life Span
A. Aging
1. Estimated incidence: 3% to 5% of elderly population >65 years of age (about one million people) have aneurysmal disease (Ohki, 2002)
2. Frequency of aneurysms increases steadily in men older than 55 years, reaching a peak of 5.9% at 80 to 85 years (Goldstone, 2002)
3. Astute physical examination needed in this population to identify aneurysms, follow individuals, and intervene when necessary
4. Continuous and diligent assessment of risk factors
5. Screening at risk populations (U.S. Preventive Services Task Force, 2005)
 VI. Pertinent Diagnostic Testing
VI. Pertinent Diagnostic Testing
A. Laboratory Tests: Complete blood count, platelet count, prothrombin time, partial prothrombin time, fibrinogen, electrolytes, blood urea nitrogen, creatinine, liver profile, urinalysis
B. Noninvasive Testing
1. Chest roentgenograms (CXR)
a. Anteroposterior (AP) and lateral x-rays
b. May be able to demonstrate aneurysm if there is sufficient calcium in the wall of the aneurysm sac (Lovell & Harris, 1991)
c. Advantages—With thoracic aneurysm, may be mediastinal widening; if leaking or rupture may have pleural effusion or pleural hematoma
d. Disadvantages—CXR is nondiagnostic, requires additional diagnostic studies
2. Abdominal ultrasonography (Barkin & Rosen, 2004; Nowygrod, 2001; Vogelzang, 2004)
a. Based on Doppler ultrasound principles—abdomen is scanned using a transducer utilizing low frequency such as 3 MHz
b. Sound waves are reflected and refracted by the structures beneath the transducer and are detected by the same transducer that is sending the signals
c. Returning sound waves are then converted to images and displayed on a monitor
d. Advantages
1) Provides noninvasive quantitative determination of severity of disease; gives estimate of size: length, width, AP diameter
2) Suitable for screening, diagnosis, and follow-up evaluation
3) Highly accurate (95%) with experienced technologist
4) Relatively inexpensive compared to invasive testing, without risks of complications
e. Disadvantages
1) Bowel gas may cause an inadequate study, so overnight fasting is usually successful in obtaining images
2) Resolution impaired by body habitus
3) Technician dependent
3. Computed tomography (CT) scan (Vogelzang, 2004)
a. Produces axial slices of the body, so that anatomy is depicted in cross-section
b. Patient placed supine in circular open gantry with x-ray tube and multiple x-ray detectors
c. Tube moves around body while emitting x-rays confined to narrow slice varying from 2 to 10 mm. Rays pass through body and are detected on opposite side by detectors
d. Advantages
1) More accurate in estimating size than ultrasonography
2) Demonstrates the relationship of the aneurysm to renal arteries and involvement of the iliac arteries
3) Helpful in identifying suprarenal extension of the aneurysm
4) Better at identifying extravasated blood and confirming the suspicion of a contained rupture
e. Disadvantages
1) Use of ionizing radiation
2) Use of intravenous contrast for best results (nephrotoxicity or allergic reaction)
3) Expensive equipment requiring experienced technical support staff and a radiologist who is familiar with interpretation of results
4) Patient must be able to lie flat in gantry without moving and intermittently hold breath for optimal imaging
4. Magnetic resonance angiography (MRA) (Vogelzang, 2004)
a. Images formed by placing patient in a magnetic field strong enough to cause a small fraction of atomic nuclei to orient with magnetic field
b. A radio frequency pulse wiggles the nuclei so that they emit signal. Through the collection of signals from hundreds of pulses, an image is created
c. Advantages
1) No ionizing radiation is used
2) Images are multiplanar (three-dimensional)
3) No arterial catheter
d. Disadvantages
1) If claustrophobia, patient will not tolerate
2) Careful screening for metals within body because of powerful magnet: avoid patients with pacemakers, implanted defibrillators, metal implants in eyes, cochlear implants
3) For patients with intracavitary metal such as staples or stents, images will reflect scatter effect from metal and may be difficult to interpret
4) User and equipment dependent for quality images
5) Gadolinium must be used with extreme caution in patients with renal insufficiency or renal failure due to increased incidence of nephrogenic systemic fibrosis (Diego, 2010)
6) Not suitable for unstable patient (O’Connor, 2013)
C. Invasive Testing
1. Arteriography (Vogelzang, 2004) (Gold Standard in outlining the vascular tree and patency of vessels)
a. Radiographic images of various segments of the arterial circulation via catheter-based injection of contrast media to outline vessel lumen
b. Transfemoral approach is the most widely used, safest, and most effective route of arteriography
c. Virtually all arteriography procedures are performed using the Seldinger technique, which involves a needle puncture of the artery followed by placement of a wire through the needle into the lumen of the vessel
d. Over this wire a catheter may be safely placed within the vessel, with the wire acting as a ‘‘guide’’ to the catheter
e. The wire is then withdrawn and the catheter can be directed to a specific location and an injection made with iodine contrast agent
1) Total contrast does not usually exceed 350 mL
2) Heparinized flush solution constantly infused to prevent thrombosis
f. Advantages
1) Useful in delineating anatomy of renal arteries and mesenteric circulation
2) Helpful in evaluating patency and involvement of iliac arteries and distal runoff below the aorta, as sites of stenosis or occlusion are identified by partial filling defect or complete lack of filling of vessel with contrast medium
g. Disadvantages
1) Invasive, arterial contrast dye injection required which may limit or prevent testing
2) Potential for arterial injury, distal embolization, or vessel occlusion from catheter
3) May require overnight hospital stay
h. Not routinely required unless reason to suspect complicating features such as associated renovascular hypertension or suspected additional aneurysms (femoral, popliteal)
 VII. Medical Management (Nonoperative)
VII. Medical Management (Nonoperative)
A. No known Evidence-Based medical treatment at present time other than optimal treatment of risk factors: hypertension, hyperlipidemia, diabetes, and smoking cessation (Chaikof et al., 2009)
B. Standard of Care is Surgical Repair to Prevent Rupture
C. Research Underway
1. Develop biochemical markers that would indicate changes in the composition and matrix of abdominal wall
2. High-resolution CT scans may be able to detect progressive loss of elasticity in aorta that might warrant closer observation
D. Research in Pharmacology (Cronenwett et al., 2000; Curciet al., 2001)
1. Beta blockers (propranolol): hemodynamic properties and biochemical effects on matrix proteins (Baxter, Terrin, & Dalman, 2008)
a. Sustained control of elevated BP
b. Blocks circulating tissue plasminogen activator and may decrease expansion by reducing plasminogen-mediated MMP activation
2. Indomethacin
a. Inhibition of aneurysm formation by lowering MMP-9 levels
3. MMP inhibitors such as doxycycline and roxithromycin
a. Inhibit a number of MMPs that stimulate the production and release of MMPs from medial smooth muscle cells (Fillinger, 2010)
b. Decrease inflammatory cell infiltrate thereby reducing expansion of small AAAs (Takagi, Masafumi, & Umemoto, 2010)
c. Need larger clinical trials
4. Statins
a. Reduce atherogenic lipoproteins, inhibit inflammation and protease inhibition in arterial wall (Buth, 2008)
b. Reduction of C-reactive protein levels that may be relevant to the pathogenesis of AAA disease (Baxter et al., 2008)
 VIII. Surgical Management (Operative)
VIII. Surgical Management (Operative)
A. Risk of Rupture
1. Natural history of AAA is enlargement and rupture
2. As a rule, the greater the size of the aneurysm, the more likely it is to rupture
3. Growth rate is 0.2 to 0.4 cm/yr and depends on aneurysm size, diastolic blood pressure, and COPD (Goldstone, 2002)
4. Information regarding growth rate and rupture risk is useful in balancing the risk of associated disease and its progression against the risk of aneurysm rupture as it increases in size
5. Aneurysms are repaired to avoid rupture
B. Indications for Surgery (Pappas, 2002)
1. Size >5.5 cm
2. Symptomatic: symptoms believed to come from aneurysm and pressure on adjacent structures
3. Rapid enlargement
4. Distal emboli: thrombotic material and atheromatous debris that line almost all AAAs may come loose and carry emboli distally to lower extremities
5. GI hemorrhage: stretching of duodenum over the enlarging aneurysm may bring about partial intestinal obstruction, or if erosion occurs, upper GI bleeding
6. Rupture
C. Preoperative Evaluation
1. Identification of preoperative risk factors as they may influence intraoperative and postoperative periods
a. Smoking
b. Angiographically significant coronary artery disease
c. Coronary artery disease
1) Angina
2) Myocardial infarction
3) Coronary artery bypass grafting
d. Hypertension
e. Peripheral vascular disease
f. Lung dysfunction
g. Congestive heart failure
h. Renal dysfunction
i. Cerebrovascular disease
j. Diabetes mellitus
2. Selective testing based upon patient status
a. Stress testing to identify underlying heart disease; if abnormal proceed with cardiac catheterization
b. Echocardiography to assess valvular function; valvular incompetence is a relative contraindication to cross-clamping of proximal aorta unless shunt or bypass technique is used
c. Carotid duplex scan to determine significant carotid stenosis
d. Pulmonary function testing to determine significant pulmonary disease; optimization may be needed prior to surgery
e. Ankle–brachial index to assess for lower-extremity disease
D. Types of Repair
1. Open aneurysmectomy (see Fig. 13-3)
a. First report of successful surgical resection and graft replacement of an infrarenal AAA in 1952
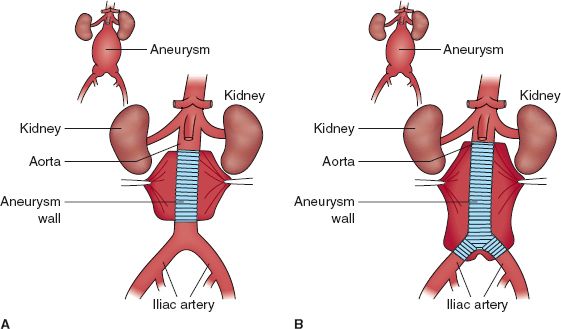
FIGURE 13.3 Aortic aneurysm repair with a tube graft (A) and a bifurcated graft (B) repair of an aortoiliac aneurysm.



