Chapter 12. Administration of injections
Background
Administering a drug, by whichever route, is with the ultimate goal of enabling it to reach a target organ or site, in order to achieve a therapeutic effect. Some drugs cannot be taken orally because the acid in the stomach alters their effect, or because they cannot be absorbed into the bloodstream through the intestinal wall. The client’s condition may also make the drug difficult to absorb orally. For example, during active labour gastric motility is reduced (drugs are usually absorbed in the small intestine) and a woman’s oral intake may be restricted by self-limitations or hospital policy. Some women may feel nauseous in labour. Pain also reduces gastric motility (Jordan 2002) therefore active labour can render the use of oral preparations, requiring systemic action, inappropriate.
Injection routes
Drugs are very effectively transported to their target via the vascular system. The speed at which this happens depends on the richness of the blood supply at the site of administration. The route by which a drug is injected must be clearly stated on the prescription chart.
Intramuscular (i.m.)
This is a common route for the administration of drugs in maternity care, including analgesics (pain relief), antiemetics (anti-sickness drugs) and oxytocics (drugs that stimulate uterine contraction). A maximum of 4ml can be given in a single injection (Johnson & Taylor 2006). In normal circumstances, the drug usually takes minutes to reach the blood supply.
It is important that the site for injection is carefully chosen, to avoid damage to underlying nerves and bone. There are five sites for intramuscular injection (Timby 2005) although the thigh and buttock are the most common.
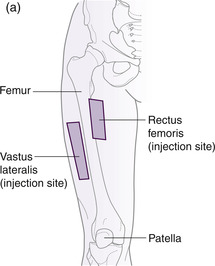
1. Thigh – into the quadriceps muscle (vastus lateralis) (Fig. 12.1a)
Consider where the arms fall when they hang loosely ‘by your side’ (you may need to stand up to appreciate this). This is the lateral aspect of the thigh; divide it into thirds, and locate the middle third. This is the intramuscular injection site, and it is particularly useful in midwifery care because it provides easy access for the administration of Syntocinon if required. It is a suitable injection site for infants.
 |
 |
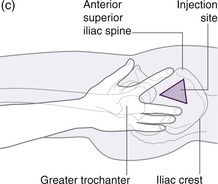 |
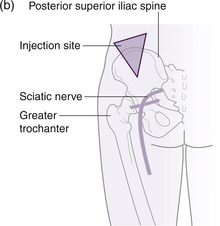
| Fig. 12.1 Sites used for intramuscular injection. (a) Vastus lateralis and rectus femoris sites. (b) Dorsogluteal site. (c) Ventrogluteal site. (Adapted from Rodger, MA and King, L (2000), with permission. Original illustration by Alison Tingle.) |
2. Thigh – into the rectus femoris muscle (Fig. 12.1a)
This site uses the middle third of the anterior aspect of the thigh and is also suitable for infants.
3. Buttock – the dorsogluteal site into the gluteus maximus (Fig. 12.1b)
Imagine someone lying on their front (prone). Looking at a buttock from above, imagine dividing it into four quarters. The injection site is the upper outer quadrant of the buttock. In practical terms, this site can be accessed whilst the woman lies on her side with her upper leg flexed, making her position more stable and the muscle relaxed.
4. Hip – the ventrogluteal site of the gluteus medius and minimus muscles (Fig. 12.1c)
This site is gaining in popularity and can be identified by placing the palm of the hand on the greater trochanter, the index finger on the anterior aspect of the superior iliac spine. Move the middle finger along the iliac crest keeping the index finger in place. The injection site is the centre of the triangle formed between the two fingers (Timby 2005).
5. Upper arm – into the deltoid muscle
This site is rarely used in midwifery practice, but is commonly used for vaccination. It is a smaller muscle and a maximum volume of 1ml should not be exceeded (Johnson & Taylor 2006). The injection site is the middle of the upper third of the upper arm (outer aspect).
Subcutaneous (s.c.)
This site is commonly used for the administration of insulin or heparin. The drug is introduced between the skin and the muscle and, because the tissue is less vascular, absorption is slower than via the muscular route. This site of injections should be rotated and may be:
The abdomen
The outer aspect of the upper arm
The outer aspect of the thigh.
The technique varies depending on the length of the needle. The needles of pre-packed syringes tend to be shorter and can be administered into the skin (grasped in the non-dominant hand) at an angle of 90°. Longer needles (including the orange 25 gauge needle) should be introduced at a 45° angle. A maximum of 2ml should be administered via this route (Johnson & Taylor 2006).
Intravenous (i.v.)
This is the site of choice when a drug needs to take rapid effect, for example, during a postpartum haemorrhage. The drug is delivered straight into the circulation and takes effect in seconds. Because the drug is in direct contact with the blood, only small doses of the drug are needed when given intravenously.
However, because of the rapid delivery of intravenous drugs and the potential for adverse reaction, this method is not routinely used in midwifery practice. Practitioners who are involved in high dependency obstetric or neonatal care may need to develop competency in the administration of intravenous drugs and should attend a detailed education and training programme in order to acquire and demonstrate this skill in line with professional standards.
Procedure for the administration of a drug by injection
The principle of safe drug administration must be adhered to in order not to put the client at risk. The practitioner must acknowledge the limitations of her knowledge and seek advice where there may be any uncertainty (NMC 2007).
It is good practice when drawing up drugs for injections that two practitioners check the drug together; however, this practice is essential when complex calculations are involved or when controlled drugs are being given (NMC 2007:38). A practitioner must never administer a drug that they did not themselves witness being drawn up. Student midwives should be supervised when they administer injections and have their signatures countersigned by the midwife (NMC 2005:10).
Another cardinal rule is that substances for injections must not be prepared in advance of their immediate use (NMC 2007:28). Although it is tempting to be well prepared for the baby’s birth, as in the introductory scenario, childbirth is an unpredictable process and unanticipated delays are common. Unattended or unidentified drugs are a potential hazard and may be inadvertently and inappropriately administered in an emergency situation.
Equipment
Anticipating an injection is not a pleasant thought and every action should be taken by the midwife to minimize the anxiety women experience before and during the procedure. It is particularly important that all equipment is gathered and prepared out of the woman’s sight and that she does not need to be left during the process in order to locate a missing piece of equipment. You will need to locate the drug card, sharps bin and collect the following in a receiver:
Needle, syringe, drug ampoule, cotton wool ball, non-sterile gloves and alcohol swab (depending on local policy).
For step-by-step guide to administration of an injection see Box 12.1.
Box 12.1




Get Clinical Tree app for offline access
Procedure for administration of a drug by intramuscular injection
■ Consult the client’s plan of care
Rationale To ensure accurate and timely administration
■ Consult the drug card, identify the drug, dose, route and time of administration, signature
Rationale To conform with legal requirements and professional guidance
■ Confirm and identify any known allergies
Rationale To prevent the risk of allergic reaction in response to contact with known allergens
■ Assess the possibility of confounding factors
Rationale To reduce the risk of drug interaction, contraindication, potentiation or overdose
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Get Clinical Tree app for offline access


