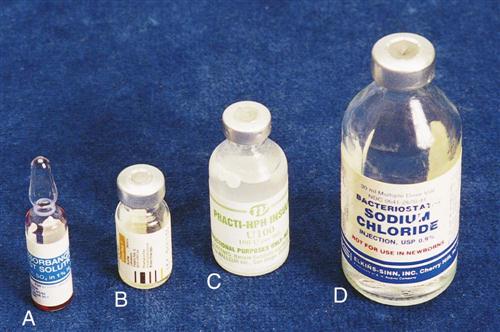
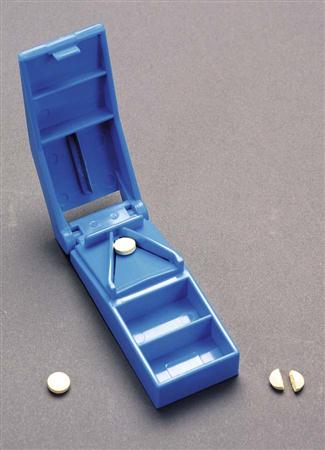
1. Define, spell, and pronounce the terms listed in the vocabulary. 2. Apply critical thinking skills in performing the patient assessment and patient care. 4. Analyze safety guidelines for specific patient populations. 5. Document the administration of a medication. 6. Summarize patient assessment factors that can affect medication administration. 7. Identify various drug forms and their administration guidelines. 8. Administer oral medications. 9. Specify parenteral administration equipment, including details about needles and syringes. 10. Follow OSHA guidelines in the management of parenteral administration. 11. Describe and demonstrate the types and locations of parenteral administrations. 12. Outline the principles of IV therapy. 13. Recognize the medical assistant’s role in patient education about the administration of drugs. 14. Assess legal and ethical issues in drug administration in the ambulatory care setting. aqueous (ak′-wee-uhs) A waterlike substance; a medication prepared with water. asymptomatic Without symptoms of a disease process. bevel (bev′-uhl) The angled tip of a needle. bronchoconstriction Narrowing of the bronchiole tubes. edema (i-dee′-muh) An abnormal accumulation of fluid in the interstitial spaces of tissues. hermetically (hur-met′-ik-lee) sealed Sealed so that no air can enter. immunosuppressant Substance that suppresses or prevents an immune system response. immunotherapy Administration of repeated injections of diluted extracts of a substance that causes an allergy; also called desensitization. induration (in-doo-rey′-shuhn) An abnormally hard, inflamed area. meniscus (meh-nis′-kus) The curved surface of liquids in a container. phlebitis (fluh-bi′-tis) Inflammation of a vein, with the possible complication of clot formation at the site (thrombophlebitis). polyuria (pah-le-yur′-e-uh) Excretion of an unusually large amount of urine. scored Slashed (e.g., a tablet manufactured with an indentation for division through the center). vasodilation An increase in the diameter of a blood vessel. viscosity (vis-kos′-uh-te) The quality of being thick and of lacking the capability of easy movement. volatile (vol′-uh-tl) Capable of vaporizing at a low temperature, such as an explosive substance. wheal (weel) A localized area of edema or a raised lesion. Dr. Anna Thau just opened a new primary care office in the community. She is in the process of hiring office staff, and Dorothy Gaston, CMA (AAMA), is being interviewed for a clinical assisting position. One of Dr. Thau’s chief requirements is that the medical assistants working in the clinical area be familiar with medications and competent in their administration. Her primary concern is the safety of her patients, so she requires that employees perform appropriate safety measures when dispensing and administering oral, topical, and parenteral drugs. While studying this chapter, think about the following questions: • Are there patient assessment factors that might affect medication administration? • Are there intravenous (IV) principles that Dorothy should understand? • Does Dorothy need to be aware of the legal implications of drug administration? Previous medication chapters in this text explained general pharmacologic principles and pharmacology math. In this chapter, you will learn about safety factors in drug administration, documentation guidelines, the forms of medications, and how they are administered. It is important to remember that medications can cause serious harm to a patient. Therefore, the process of dispensing and administering medications must always be treated with great care. Each member of the healthcare team involved in medication administration must be constantly vigilant to prevent errors and to deliver high-quality patient care. No matter the type of medication administered, the order first must come from the physician. If the physician delegates drug administration to the medical assistant, this must be allowable under state law. Each state has a medical practice act that defines whether a medical assistant can administer drugs under the supervision of a physician. Some states allow medical assistants to administer only certain types of medications; some prohibit medical assistants from giving injections. You should obtain from your local government or medical society information about the scope of practice for medical assistants in your particular state. You should know what the law states and how your duties fit into that law. To ensure patient safety in drug administration, the medical assistant must perform certain procedures every time a medication is ordered. First, it is essential that the medical assistant understand the physician’s order. Safety starts with a clearly written order that can be easily read and understood. Ask the physician for clarification if you have any questions about the medication, dose, strength, or route of administration. Once the order has been clarified, the medical assistant is responsible for looking up the drug in a pharmacology reference, such as the Physicians’ Desk Reference (PDR) (see Chapter 33). A medication should never be given until its purpose, possible side effects, precautions, and recommended dose are known. After the medical assistant learns about the drug ordered, the medication is dispensed and administered. To safeguard the patient during this process, the medical assistant uses the “seven rights” of proper drug administration. Remember, however, that the patient always has the right to refuse to take a medication. If this occurs, make sure you inform the physician immediately, because he or she may want to follow up with the patient about the importance of the prescribed medication. If a patient refuses to take an ordered medication, be sure to document this refusal in the patient record. The seven rights of drug administration are as follows: 2. The right drug. This begins with clarification of the physician’s order if needed. Every time a drug is dispensed, the label must be checked three times to confirm the right drug, dose, and strength. You must be competent in reading and understanding the information on the drug label. The drug’s name and strength on the label must exactly match the physician’s written order. Compare the physician’s written order with the medication label when you: • Take the medication from the storage area • Dispense the medication from the container • Replace the container to storage or before discarding the used container 7. The right documentation. Immediately after administering the drug, document the date and time of administration; the drug’s name, strength, dose, and route of administration; any reactions the patient has to the medication; and the details of patient education about the drug. For parenteral medications, inspect the site of injection before administration for scarring, altered pigmentation, or any other indication of a possible problem with medication absorption. The exact site of administration must be charted. If the patient calls in for a prescription refill, document all pertinent information on the patient’s chart as well. Procedures 35-1 and 35-2 present the safety measures to be followed in preparing and administering a medication and documenting it properly. As discussed in Chapter 33, the chosen route of drug administration determines the rate and intensity of the drug’s effect. A drug prepared for one route but administered by another route may not have any effect at all and is potentially dangerous. Each route requires different dosage forms. The basic forms for solid oral dosage are tablets, capsules, and lozenges (troches). Figure 35-1 depicts typical caplets, capsules, and tablets. Tablets are compressed powders or granules that, when wet, break apart in the stomach—or in the mouth if they are not swallowed quickly. Tablets may be sugar-coated to taste better, or enteric-coated (e.g., Ecotrin) to protect the stomach mucosa. Buffered tablets are also designed to prevent stomach irritation by combining the drug with a buffering agent that reduces the amount of acidity in the compound. Buffered or enteric-coated tablets should never be crushed or dissolved. Only scored tablets can be cut in half. This is accomplished with a pill cutter (Figure 35-2). Some tablets are coated with a volatile liquid that helps the medication quickly dissolve in the mouth, such as certain antacid tablets and Claritin RediTabs, which are designed to dissolve on the tongue rather than to be swallowed. Caplets are tablets without a coating; they are solid and oblong, similar in shape to capsules. Capsules are gelatin-coated and dissolve in the stomach, or they may be enteric-coated to protect them from stomach acids. Timed- or sustained-release (SR) capsules or spansules are designed to dissolve at different rates over a period of time to reduce the number of times a patient has to take a medication. These drugs should never be crushed or dissolved, because this negates their timed-release action. Another form of oral medication, the lozenge (or troche), is a flattened disk that is dissolved in the mouth to coat the throat, such as a lozenge for a sore throat. Many liquid forms of medication are available. They differ mainly in the type of substance used to dissolve the drug: water, oils, or alcohol. A solution is a mixture of a liquid (usually water) and a powdered drug product (e.g., Amoxicillin solutions for pediatric patients). A solution separates if left standing, so you must shake the container before administering the medication. Liquid forms include the following: • Suspensions: Suspensions are insoluble drug substances contained in a liquid. Examples include the following: A drug substance can be mixed with alcohol to enhance the drug’s properties. Examples include the following: If the drug is not intended to coat the oral cavity or throat, oral medications should be taken with enough water to transport the drug to the stomach. Make sure the patient is able to swallow the medication. It may be helpful to place the medication on the back part of the tongue. Liquid medications are ideal for children. Solid drugs should not be administered to children until they reach the age at which they can safely swallow a solid drug form without the danger that they will aspirate the drug. Oral syringes are the best way to give liquid medications to children because there is less likelihood the medication will be spilled (Figure 35-3). Liquid medications, especially those that stain the teeth, can be taken through a straw. If the patient has been vomiting or is nauseated, an alternative route of administration may be necessary. Always remain with the patient until all of the medication has been swallowed. Procedure 35-3 outlines how to dispense and administer oral medications. Some mucous membranes are selected for their ability to absorb medication for a systemic effect. The most commonly used areas are the gums, the cheeks (buccal), under the tongue (sublingual), the rectum, and the respiratory mucosa (inhalation). Nasal, ophthalmic, rectal, and vaginal preparations may also be applied to these mucous membranes for their localized effects. Inhalation drugs are discussed in Chapter 46. The rectal mucosa allows rapid absorption of a drug, even though the surface of the rectum is small. Drugs are absorbed directly into the bloodstream without being altered, as they would be by the digestive processes, and without irritating the patient’s gastric mucosa. Rectal medications are useful if the patient is nauseated, vomiting, or unconscious. For example, Tylenol or Compazine suppositories may be prescribed for a child who has fever, nausea, and vomiting. Manufacturers supply rectal medications in the form of gelatin- or cocoa butter–based suppositories, which melt in the warmth of the rectum and release the medication (Figure 35-4). Suppositories may also be used to soften the stool or to stimulate evacuation of the bowel; enemas are used to cleanse and evacuate the bowel. The best time to administer a rectal drug intended for a systemic effect is after a bowel movement or enema. The patient should be cautioned to remain lying down for 20 to 30 minutes to prevent accidental evacuation of the drug. Of course, suppositories intended to treat constipation are administered to bring about bowel evacuation. The patient should be instructed to remove the outer wrapping and insert the suppository approximately 2 inches above the rectal sphincter muscles; a little mineral oil or vegetable oil may be used as a lubricant. If suppositories are individually wrapped in foil, make sure the patient knows that the foil is the wrapper and is not part of the treatment. Suppositories are typically stored in the refrigerator to keep them firm. Vaginal suppositories, tablets, creams, and fluid solutions are used to treat local infections. Irrigating solutions (douches) may be used as anti-infective treatments. Creams and foams are available as local contraceptives. Vaginal instillation is most effective if the patient remains lying down after administration to prevent leakage; many preparations, therefore, are intended to be used at bedtime. The patient may need to wear a pad to absorb drainage. Solid suppositories and tablets may be lubricated or moistened with water and inserted by hand or with an applicator. Creams are instilled with applicators. Prepackaged, disposable irrigation kits are available for douching. When instructing patients, confirm that the patient can differentiate the urinary meatus from the vaginal orifice and the rectum. Mistakes could result in vaginal infections or in damage to or infection of the urinary tract. A simple drawing and explanation may be required. Mouth and throat agents come in the form of sprays, swabs, sublingual tablets, and buccal tablets. The mouth and throat membranes may be treated locally with antiseptics for oral hygiene and local infection, with anesthetics for pain relief, and with astringents that form a protective film over the mucous membranes. The patient may have to gargle, or the area may be painted or sprayed. To paint or spray the throat, first look for the area of inflammation to be treated. Otherwise, the part needing treatment may be missed entirely. Avoid touching the posterior pharynx (back of the throat); this causes gagging and possibly vomiting. Sublingual (SL) tablets are placed under the tongue, where they are rapidly absorbed into the bloodstream by the rich supply of capillaries. Sublingual absorption is systemic and bypasses the acids in the stomach. Nitroglycerin, used for treating the chest pains of angina pectoris, may be administered sublingually. Patients should not chew or swallow sublingual medications. The patient should be instructed not to smoke, eat, or drink immediately before administration of these drugs. Buccal tablets are placed between the cheek and the upper molars and are quickly absorbed by the oral capillaries. Nose drops and nasal sprays may be used for localized effect, but, like the inhalation drugs, they can spill over into the bloodstream. Some nasal preparations, such as decongestants, can cause an increased heart rate, elevated blood pressure, or central nervous system stimulation. Nasal medications are commonly used for blocked nasal passages (decongestants) and nosebleeds (hemostatics). Instillation of nasal medications is covered in Chapter 37. Nasal decongestant sprays are often misused by patients. Be sure to teach the patient not to exceed the amount or frequency ordered by the physician. If too much is used, these drugs can dry the mucosa and make congestion worse. Nasal inhalants can also be used for their systemic effect, such as the corticosteroid Flonase, which may be prescribed as part of asthmatic treatment. Topical drugs are prescribed for both local and systemic effects. Skin medication forms include lotions, liniments, ointments, and transdermal patches. The medical assistant should wear gloves when applying any topical treatment, to prevent self-administration of the drug. Often used to control itching, lotions are applied by dabbing with a soft cloth, a cotton ball, or a tongue blade. Calamine is an example. Some lotions are used to relieve inflammation and pain in muscles and joints. After the lotion has been applied, the area may be covered with a thick cloth to retain heat. However, the therapeutic value of these preparations is controversial. The effects of musculoskeletal lotions are limited to the skin surface where the medication is applied. Liniments (emulsions) have a higher portion of oil than lotions, and volatile active ingredients may be added. Liniments are often used to protect dried, cracked, or fissured skin. Ointments, such as bacitracin, are semisolid medications containing bases such as petrolatum and lanolin. An ointment should be removed from a jar or tube with a tongue blade to prevent contamination of the remaining medication. Certain medications can be absorbed slowly through the skin to create a constant, time-released systemic effect (Figure 35-5). The nitroglycerin patch is particularly useful for patients with frequent attacks of angina. Hormone patches, such as estrogen and testosterone, also can be absorbed slowly through the skin. With dermal patches, drugs can be administered in a time-released manner for as long as 7 days. The date and time the patch was applied should be written on the patch and documented in the patient’s record. Injectable medications must be sterile and in liquid form. These medications may be supplied in an ampule, a single-dose vial, or a multidose vial (Figure 35-6). The drug usually is in a solution that is minimally irritating to human tissues (e.g., physiologic saline solution, sterile water) and may contain a preservative or a small amount of antibiotic to prevent bacterial growth in the vial. All injectable medications are dated. Before use, check the expiration date and examine the solution for possible deterioration. If the medication is discolored or if any sediment has formed at the bottom of the vial, the vial should be discarded. A parenteral medication is administered with a sterile syringe and needle. Occupational Safety and Health Administration (OSHA) guidelines must be followed when any sharp is used, including all types of needles, because every needle used on a patient is contaminated with blood and body fluids. The medical assistant must wear disposable gloves when administering parenteral injections, must immediately dispose of the needle and syringe unit into a sharps container after use, and must never recap used needles. An ampule is a small, hermetically sealed glass flask that contains a single dose of medication. Its neck has a scored weak point where the ampule is broken just before use (Figure 35-6, A). Procedure 35-4 explains the special technique required for opening an ampule of medication and withdrawing medication for administration.
Administering Medications
Learning Objectives
Vocabulary
Scenario
Safety in Drug Administration
Drug Forms and Administration
Solid Oral Dosage Forms

Liquid Oral Dosage Forms
Oral Administration

Mucous Membrane Forms
Rectal Administration

Vaginal Administration
Oral Administration
Nasal Administration
Topical Forms
Lotions
Liniments
Ointments
Transdermal Patches

Parenteral Medication Forms
Ampule
Administering Medications
Get Clinical Tree app for offline access

 deltoid. Pt informed this is the first of 3 doses. No side effects noted. Appointment scheduled for patient to return in 1 mo for second dose. — — — — — — — — — — — — D. Gaston, CMA (AAMA) ________________________________________
deltoid. Pt informed this is the first of 3 doses. No side effects noted. Appointment scheduled for patient to return in 1 mo for second dose. — — — — — — — — — — — — D. Gaston, CMA (AAMA) ________________________________________