Ensuring the safety of the patient 100
Prioritising the initial management: GCS and ABCDE 101
Managing ‘medical’ and ‘neurological’ coma 107
Responding to neurological deterioration 195
Meningococcal meningitis 130
Introduction
The major issue in the patient who presents as a neurological problem is to decide whether the patient needs supportive care or whether the patient needs active intervention. Many cases who present as neurological emergencies will recover fully, given time and good supportive treatment, because their underlying disorder is fully reversible. Examples include coma due to self-poisoning and the confusional states that follow an epileptic fit. Other cases require a much more active approach: typical examples are antibiotics for acute meningitis, glucose for hypoglycaemia and neurosurgery for subarachnoid haemorrhage. Therefore management decisions can only be made safely if the correct diagnosis has been established. Time is critical in neurological cases, as the nervous system has limited powers of recovery – the diagnostic path has to be followed with an appropriate degree of urgency. The Acute Medical Unit has a duty to ensure the safety of the patient during this time and the nursing staff have the key role in this process (→Box 4.1).
Box 4.1
1. Ensure the safety of the patient
2. Prioritise the initial management
3. Differentiate and manage ‘medical’ and ‘neurological’ coma
4. Identify and respond to neurological deterioration
5. Reach appropriate outcomes
Role of the Acute Medical Unit in Acute Neurological Problems
Ensuring the Safety of the Patient
There must be confidence in the ability to support the patient while the correct diagnosis is being reached. The role of the Acute Medical Unit at this stage is to prioritise the initial management. It may, for example, be necessary to stabilise the patient’s condition before attempting to take a history.
There are four critical initial observations:
• Are the vital signs stable?
• Is the airway secure and is ventilation adequate?
• Is there a non-neurological condition that needs immediate attention?
• Is there anything neurological that needs urgent active intervention?
It is critical that the patient reaches the appropriate service in the best possible condition, be it the acute neurosurgical unit, the stroke unit, the general medical wards or the ITU.
Prioritising the Initial Management
GCS and ABCDE: Assessing and keeping the patient alive
Protection of the airway, ensuring adequate ventilation and maintaining the circulation are the immediate priorities in any patient. At the most basic level this means:
• ensuring the upper airway is patent
• giving sufficient oxygen
• securing i.v. access and maintaining the blood pressure
Warning: At this first stage, if meningococcal meningitis is suspected appropriate i.v. antibiotics must be given straight away.
If there is any suspicion of a neck injury (an example would be a patient who had been found at the bottom of some steps, having had an apparent fall), the neck must be protected and immediately X-rayed. If there is a cervical spine fracture, manipulating an unsupported neck either to establish an airway or to move a patient around in bed can damage the spinal cord beyond repair. At least be aware of the risk, know how to apply a stiff collar and use sand bags to support the neck, and if there is any doubt protect the neck and log-roll the patient until the neck films have been cleared by a radiologist.
Critical nursing observations
Blood sugar
Hypoglycaemia is the most important cause of a fully reversible neurological disorder. At blood sugars below 3mmol/L the patient becomes comatose and may fit, but any neurological picture can be caused by hypoglycaemia. Providing the patient has not suffered irreversible damage from sustained hypoglycaemia, correction of the blood sugar will lead to a full and rapid recovery.
Response of the pupils
The size, symmetry and reactivity of the pupils are fundamental neurological observations. The most common cause of bilaterally fixed and dilated pupils is self-poisoning with tricyclic antidepressants, whereas poisoning with both opiates and diazepam-like drugs produces fixed constricted pupils.
The major reason for following the change in the pupils is to identify ‘uncal herniation’: a shift of the brain because of cerebral oedema that results in the IIIrd cranial nerve being ‘pinched’ between the brain and part of the skull (→Fig. 4.3). As the IIIrd nerve is responsible for pupillary constriction, an early warning of uncal herniation is pupillary dilatation followed by loss of the light reflex.
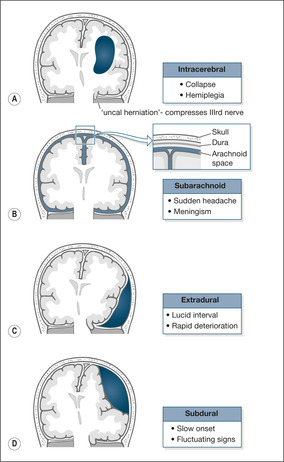 |
| Fig. 4.3 |
Any suspicion that a pupil is dilating and losing its light reflex must be reported to the medical staff for action to reassess the neurological status of the patient.
Temperature
In the right context, an increased temperature should be considered strong evidence of intracranial sepsis: meningitis, more rarely meningo-encephalitis, or even a collection of intracranial pus (intracerebral abscess).
Not every fever in a neurological emergency is due to intracranial sepsis, as there may be infection elsewhere such as aspiration pneumonia. High temperatures also characteristically occur in brain stem strokes. Nonetheless, intracranial infection should be the first consideration because of the need for immediate action.
Pulse
The rhythm and rate of the pulse are important. They may draw attention to non-neurological problems that need to be addressed. Extreme bradycardia, for example, may be the cause of an unexplained blackout. Atrial fibrillation is recognised by the irregularity of the pulse and its presence increases the likelihood that an acute stroke is due to a clot of blood finding its way from the left atrium (a fibrillating atrium encourages clot formation) to the brain: an embolic cerebral infarction. Changes in the pulse can be important: progressive slowing can indicate increasing ICP and is often accompanied by an increasing blood pressure.
Blood pressure
Hypertension is commonly seen as an acute response to neurological events such as intracranial haemorrhage or large cerebral infarction. Severe hypertension can also complicate coma caused by self-poisoning with sympathomimetic recreational drugs such as ecstasy, amphetamines and cocaine, and may need urgent correction. However, in most neurological conditions, including stroke, lowering the blood pressure acutely to ‘normalise’ it is fraught with danger. The brain is usually fairly impervious to changes in blood pressure as the cerebral blood flow ‘autoregulates’: if the blood pressure drops, the vessels open up to allow greater flow through them. If there is a major neurological insult this autoregulation is lost, so if the blood pressure falls the blood supply also decreases, which may worsen the neurological deficit. Therefore in acute situations, especially in strokes, the temptation to ‘treat’ a high blood pressure should in most situations be resisted. The only exceptions are in special situations when very high levels, say around 230/140mmHg, are considered dangerous. Nonetheless, any change in blood pressure must be gradual.
As already explained, the combination of a progressively falling pulse and an increasing blood pressure may, in the appropriate circumstances (such as the aftermath of a major intracranial bleed), be a sign of increased ICP.
Respiratory rate
The respiratory rate remains an essential observation in the patient who is critically ill, whatever the cause. It is particularly important to document any changes in respiratory rate. Thus in the neurological emergency a falling respiratory rate may reflect deepening coma. If the change in consciousness level is due to increasing ICP, the slowing respiration is accompanied by a falling pulse and rising blood pressure. It is instructive to contrast this with the signs that are seen in shock, in which a change in consciousness level is accompanied by an increase in the respiratory rate, an increase in the pulse and a decrease in the blood pressure.
Oxygen saturation
Hypoxia remains a common, yet easily correctable, cause of avoidable death on acute emergency wards. The normal oxygen saturation is around 97% and it must be appreciated that to decrease the saturation to 90% or less requires a major disturbance in ventilation that may be due to deepening coma and a worsening neurological state. A fall in oxygen saturation needs careful reassessment.
• Is the coma deepening?
• What about the lungs and the circulation?
• Should blood gases be checked?
• What is the respiratory rate?
It must be remembered that the oxygen saturation does not always reflect the level of ventilation. If the patient is on a high concentration of oxygen, the saturations can be more or less normal even when the patient is hardly breathing. The saturations must not be interpreted in isolation. There would be no reassurance from an oxygen saturation that had stayed constant for 4h at 95% if, during that time, the GCS had dropped from 12 to 4 and the respiratory rate had fallen from 15 to 8 breaths/min. This patient should be on ITU with a view to immediate ventilation.
Glasgow Coma Score
The GCS was described in 1974 as a way to assess any patient with an altered level of consciousness. It is based on three categories of response: eye opening, the best motor response and the best verbal response (→Table 4.1; Fig. 4.1). The GCS is the universal measurement of the depth of coma. It is simple to carry out and score and, provided it is performed properly, the result should be the same whoever makes the measurement.
| Response | Score |
|---|---|
| Eye opening (E) | |
| Spontaneously | E4 |
| To verbal command | E3 |
| To pain | E2 |
| No response | E1 |
| Best motor response (M) | |
| Obeys commands | M6 |
| Localises pain | M5 |
| Withdraws to pain | M4 |
| Abnormal flexion to pain | M3 |
| Extension to pain | M2 |
| No response | M1 |
| Best verbal response (V) | |
| Orientated and converses | V5 |
| Disorientated and converses | V4 |
| Inappropriate words | V3 |
| Incomprehensible sounds | V2 |
| No response | V1 |
| Total score (3 to 15) |
 |
| Fig. 4.1 |
The GCS can be documented on a chart as the grand total from the three categories against time or as E4 M6 V5, etc. As a general rule the scores reflect the severity of the neurological status:
| mild | 13 to 15 |
| moderate | 9 to 12 |
| severe | 3 to 8 |
Coma is defined as a GCS of less than 9.
The initial GCS, often performed by the paramedics outside hospital, acts as a baseline. A low initial GCS score (less than 9) will mean the airway is vulnerable and the patient is at risk from aspiration.
A change in the GCS is the single most important observation in the acute neurological patient. A fall in GCS needs immediate attention. Deepening coma may need increased supportive measures, perhaps involving a move to ITU with a view to ventilation. More critically, a fall in GCS is often the first sign of increasing ICP, which occurs in active intracranial bleeding, intracranial sepsis and during the development of brain oedema following a cerebral infarct.
Some triage systems use an abbreviated assessment of the consciousness level based on the acronym AVPU:
| A | Alert |
| V | Responds to voice |
| P | Responds to pain |
| U | Unresponsive |
This is quick to perform and easy to recall. It is useful as part of a rapid primary assessment, but it is not detailed enough to use for serial observations.
Top to toe examination
Those closely involved with the care of acute neurological disorders should be aware of the importance of quite subtle physical signs in giving clues, particularly of head injury and infection. A head injury can result in local bogginess or scalp bruising, perhaps a palpable depressed skull and bleeding or loss of CSF from the ears and nose. Fractures to the base of the skull characteristically produce bruising around the eyes (‘raccoon eyes’) and behind the ears (Battle’s sign). All these can and will be missed by clerking doctors, particularly if a ‘stroke’ label has been attached to the patient and the examination is less than thorough because of the pressures of time. Be particularly careful to look at any sites that appear to be the source of pain. Severe sinus sepsis is tender to the touch and very painful; falls from whatever cause lead to fractured hips; and grand mal fits can produce shoulder dislocation. A widespread haemorrhagic skin rash will clinch the diagnosis in meningococcal septicaemia, but it can appear with alarming speed, sometimes even after the patient has been clerked in.
A reliable history
One of the difficulties with neurology is the unreliability of the preadmission diagnosis. Unfortunately, diagnostic labels tend to stick and the consequences can sometimes be disastrous: the ‘cerebrovascular accident’ turns out to be a subdural bleed, ‘off legs’ a spinal cord compression, the ‘well-known epileptic’ a case of recurrent syncope due to intermittent heart block, and so forth. Every neurological patient who is admitted to hospital should be looked at afresh, particularly where there is a ‘known case of…’ Known by whom and with what degree of certainty? Are we sure that the original diagnosis still applies?
It is not advisable to make ‘stroke’ the initial diagnosis in a patient in coma, even if there is a past history of cerebrovascular disease. This is particularly the case in elderly patients. It is a dangerous tendency to attribute all changes in the consciousness level, all funny turns and all episodes of dizziness to a ‘CVA’ just because the patient is 80 years old.
Recent causes of coma initially labelled as stroke on our Acute Medical Unit included:
• post-ictal state
• respiratory failure
• overdose
• subarachnoid bleed
To make an accurate diagnosis, the history and eyewitness accounts are absolutely critical. By their nature, acute neurological problems are difficult to assess. The patients are often confused or uncooperative, making history taking and examination difficult. Nonetheless, these are the very patients in whom a correct diagnosis is paramount. Skills that are needed to assess patients with confusion or impaired consciousness levels must be perfected. Exact histories must be obtained from relatives and eyewitnesses, in particular to establish whether there is a possibility of trauma to the head or cervical spine. The typical sequence of events leading to a post-traumatic brain haemorrhage is of a head injury with transient loss of consciousness followed by amnesia for the event. The patient then becomes confused and aggressive and may fit. The GCS then starts to fall as a result of the haemorrhage. The patient may present at any of these stages. Intracranial infection is also easy to miss: here the critical questions are concerned with recent sinus or middle ear infections. Collections of pus in and around the brain present with stroke-like illnesses and are frequently missed because a proper history has not been taken and the conditions not even considered.
Managing ‘Medical’ and ‘Neurological’ Coma
Coma is defined as a GCS of 8 or less. Broadly there are two types: ‘medical’ coma, which is coma due to conditions such as liver failure, respiratory failure and DKA, in which the management is primarily aimed at the underlying disease; and ‘neurological’ coma due to conditions such as stroke, subarachnoid haemorrhage and meningitis.
The underlying mechanism in coma
Coma that lasts more than 4h is usually due to one of four groups of conditions (→Box 4.2). By far the most common cause is self-poisoning (40%).
Box 4.2
| • Self-poisoning with sedative drugs | 40% |
| • Post-hypoxic cerebral damage | 25% |
| • Stroke | 20% |
| • Metabolic disorders | 15% |
Several features of the patient’s initial observations can be used to identify coma that is due to causes other than a stroke (→Box 4.3). This has a practical purpose, because coma due to stroke has an extremely poor prognosis, whereas some of the other causes may be reversible.
Box 4.3
• Deep coma
• Reactive pupils
• Pyrexial
• No deviation of the eyes to one side
• Moves all four limbs
There are five causes of coma that must not be missed as they are all treatable and relatively easy to diagnose, provided that they are considered at the time of the initial assessment (→Box 4.4).
Box 4.4
• Sugar (high or low)
• Sepsis
• Sub- (and extra-) dural haemorrhage
• Special causes of coma (respiratory failure, renal failure and liver failure)
• Secret overdoses (late presentation of paracetamol/tricyclic overdose)
Practical management of coma
The systematic way to approach the patient with coma is to use the universal system of primary assessment based on the simple mnemonic ABCDE.
A is the airway
‘Are you all right?’ If the patient responds appropriately, there is unlikely to be an airway problem. The airway can be maintained with a jaw thrust or chin lift. Placing the patient in the recovery position may be necessary (providing there is no sign or suspicion of spinal injury). Use a Guedel oral airway if it can be tolerated. Administer high-flow oxygen immediately. Look, listen and feel for expired air.
B is the breathing
• Count the respiratory rate (breaths/min):
| Less than 10 | imminent respiratory arrest |
| more than 20 | ill |
| more than 30 | critically ill |
• Listen for noise (wheeze, upper airway gurgling, ‘croup’)
• Assess the effort
• Perform oximetry
• Continue high-flow oxygen
• Keep the saturations greater than 90%
C is the circulation
• Assess pulse rate and strength
• Assess capillary refill (press finger pulp for 5s and release; refill should be less than 2s). This gives an idea of the peripheral circulation
• Measure the blood pressure
D is the disability
• GCS
• Assess pupil size, equality and reaction
• Measure blood sugar (give sugar for hypoglycaemia and, if there is a suspicion of alcohol abuse, thiamine)
Importance of an eyewitness in coma
Any relatives or eyewitnesses must be kept on the ward and interviewed (or if necessary telephoned). Their information may provide vital clues to the likely diagnosis. It is unacceptable for the doctor or the nurse ever to conclude that a history is either unobtainable or unavailable. Cerebral malaria is the classic example to emphasise this point: fatal if undiagnosed, curable with drugs, but too rare to remember to consider as a cause of coma. Only the patient’s relatives will tell you of the safari holiday taken a week before the onset of headaches, fever and confusion. Patients who are most at risk are the least able to provide a good history for themselves. It is critical to ascertain whether there is a possibility of trauma. Patients with head injuries and trauma to the cervical spine are not usually admitted to the medical wards, but you should not lower your guard: in neurology the most challenging and difficult problems are those in which a history is unavailable and for which preadmission clinical details are scanty. Review all the details in the paramedics’ record. Their information is often comprehensive and systematic and dates from soon after the event. A good paramedic assessment will give you important data on the circumstances in which the patient was found, the initial GCS and their clinical course in the critical early stages of the illness.
Responding to Neurological Deterioration
It is not sufficient to document neurological observations. The reason for performing these time-consuming and exacting assessments is to act as soon as they change. The patient described below (→Case Study 4.1) sustained traumatic intracerebral bleeding and was ‘coning’ (a shift of the brain as a result of raised ICP). The signs of increasing ICP were identified, but immediate action was not taken. A one-sided dilated pupil is often the earliest warning sign of elevated ICP which, if not corrected urgently, leads to a pressure cone.
Case Study 4.1
A 59-year-old man on warfarin for a valve replacement was taken to the AED having collapsed and fallen backwards, striking and bruising his head. He appeared well, but X-rays showed a basal skull fracture. In view of his ‘medical’ problems, he was admitted to the Acute Medical Unit, where he was described as ‘drowsy and vague, complaining of headache’. He was moderately over-anticoagulated (INR 4.9). Half-hourly neurological observations recorded a systolic blood pressure increasing from 130 to 220mmHg and a sluggishly reacting right pupil which, over 3.5h, became more dilated. He was responsive to commands until 04.00h, 6h after admission, when he suddenly vomited copiously and became unresponsive (GCS 3).At this stage his right pupil was fixed and dilated. His anticoagulation was reversed with fresh frozen plasma. He was intubated, ventilated and sent urgently to the neurosurgeons.
How the clinical state can change in the first hours of admission
Case Study 4.2, Case Study 4.3 and Case Study 4.4 illustrate how the clinical state can change rapidly.
Case Study 4.2
A 55-year-old man became acutely confused the day after returning from a Turkish holiday. Over the next 48h his speech deteriorated and he became increasingly difficult to rouse. He then had a series of tonic-clonic convulsions. Investigations showed a severe viral encephalitis.
Case Study 4.3
A 19-year-old student was admitted on Christmas Eve with an acute abdomen. In the recovery room after a negative laparotomy, the anaesthetist noticed a petechial rash. Lumbar puncture was normal, but treatment for meningococcal infection was started. Repeat lumbar puncture 8h later yielded ginger-beer coloured CSF which grew meningococci. He recovered fully.
Case Study 4.4
An 80-year-old man developed dizziness and a mild hemiparesis. On admission his GCS was 15 but he could not swallow at all. He would not tolerate an airway. Late the same night he vomited and dropped his GCS to 5. He became acutely short of breath and pyrexial.The cause of his deterioration was an aspiration pneumonia. In spite of physiotherapy and antibiotics, he deteriorated and died.
Other important examples include:
• deepening coma in an overdose
• deterioration due to missed infection elsewhere (blood, urine, chest, etc.)
Reaching Appropriate Outcomes
The combination of good nursing and medical care should aim to reach an appropriate outcome for every patient. Important outcomes and the principles by which they can be achieved are listed below.
Transfer to the stroke unit in an optimum condition
• Coma management
• Swallowing assessment
• Early aspirin where indicated
Avoiding major stroke after a transient ischaemic attack
• Urgent investigation of suspected TIAs and minor strokes
Surviving intracranial sepsis
• Early treatment of meningitis
• Recognising and managing complications
Reaching the neurosurgeons alive and on time
• Recognising operable intracranial bleeds
• Diagnosing intracerebral masses
• Managing increased ICP
Full recovery from self-harm
• Responding to a changing GCS
Recovery from reversible causes of neurological emergencies
• Rapid and effective primary assessment
• Good coma management
Stroke and Stroke-Like Emergencies
The World Health Organisation’s definition of a stroke is a syndrome of rapidly developing clinical signs of focal (e.g. hemiplegia) or global (e.g. coma) disturbance of function, with symptoms lasting 24h or longer (or leading to death) with no apparent cause other than of vascular origin.
The time frame of 24h is to differentiate a stroke from a TIA, which recovers rapidly but is an important risk factor for developing a subsequent completed stroke. There are around 2.4 strokes per 1000 population per year. As 80% of these will be admitted as emergencies, most Acute Medical Units can expect to admit one to two strokes per day. It is important, however, not to overuse the stroke label on the Acute Medical Unit. Estimates suggest overdiagnosis, with up to a fifth of all ‘strokes’ turning out to be something else: post-epileptic states, toxic states due to infection, and metabolic problems such as respiratory failure.
Two factors have had a major impact on improving the outlook after a stroke in terms of mortality and long-term disability: the introduction of Acute Stroke Teams who become involved at, or soon after, emergency admission, and the increased availability of stroke rehabilitation in specialist Stroke Units. Nonetheless, stroke remains the most frequent cause of major disability in adults.
There is increasing emphasis on drugs that improve the outcome of stroke or prevent further damage. Aspirin, given as soon as a diagnosis of ischaemic stroke has been confirmed, reduces the risk of recurrence. Emergency thrombolysis (which needs to be given within three hours of the onset of symptoms) significantly improves the neurological outcome in cerebral infarction and should now be standard practice in the UK. Recent studies have shown that, after a stroke, lowering the blood pressure (for example with the combination of the ACE inhibitor, perindopril, and the diuretic, indapamide) and lowering the cholesterol with a statin improve the outlook – and that this benefit is obtained even if the initial blood pressure and cholesterol level were normal. High blood sugars after a stroke may also be harmful and careful sugar control is likely to become a routine part of emergency stroke management.
Causes
Most typical strokes are caused either by a cerebral infarction (an area of brain tissue death) or by an intracerebral haemorrhage (bleeding into and around the brain). Stroke-like illnesses are also caused by subarachnoid haemorrhage, subdural haemorrhage and extradural haemorrhage. Subarachnoid haemorrhage is an important cause of sudden severe headache and collapse and requires neurosurgical input. Subdural and extradural haemorrhages are rare but important causes of stroke-like illnesses that can be treated successfully if they are recognised in time.
Cerebral infarction (approximately 80% of all strokes)
A cerebral infarction occurs when the blood supply to part of the brain is cut off, resulting in a focal area of brain-tissue death (an ischaemic stroke). There are two ways in which the blood supply can be interrupted: by a clot that travels through the arterial system and becomes lodged somewhere critical in the cerebral circulation (cerebral embolus), or by a clot that forms within the cerebral arteries themselves (cerebral thrombosis).
Cerebral embolus
Left atrial clot. The most common cause of left atrial clot is atrial fibrillation. In atrial fibrillation, normal regular atrial contraction is replaced by irregular, uncoordinated atrial activity more akin to muscular shivering than proper contraction. As a result blood stagnates and can form a clot within the atrium. There is a particular risk of this happening if there is also heart disease in the form of heart muscle damage (which leads to further stagnation) or diseased valves (which can act as a focus for clot formation). Atrial fibrillation is a common age-related arrhythmia. It is found in around 8% of people older than 80 years and constitutes a major risk factor for stroke. However, the risk can be significantly reduced by anticoagulating patients who have atrial fibrillation so that there is less chance of clot formation, or by trying to restore a normal heart rhythm.
Left ventricular clot. It is quite common for a clot to form on the inside of the heart chamber over the scar of a recent myocardial infarction. In most cases the clot stays put, but there is always a risk of it breaking loose and travelling to the cerebral circulation. This is a particular problem in the first week or two after a myocardial infarction, when the clot is new.
Carotid artery clot. Atheromatous hardening of the carotid arteries has two relevant consequences for stroke formation. It may lead to critical narrowing (carotid artery stenosis) with a reduction in the blood supply to the brain. More importantly, blood clots form on the abnormally roughened arterial wall and can break off to lodge within the cerebral arterial tree. Small emboli produce minor stroke-like symptoms (TIAs), which are warning signs of a subsequent major stroke.
Cerebral thrombosis
Hardening of the cerebral arteries (cerebral arteriosclerosis) leads to narrowing of the vessels and can progress to atheromatous plaque formation and localised thrombosis with blockage. As with atheroma elsewhere in the body, there are several causes: these include smoking, high cholesterol and a positive family history.
The two most important risk factors are:
• hypertension
• diabetes
Of the two, hypertension is the more significant: a diastolic blood pressure of 110mmHg or more increases the stroke risk 15-fold. This compares with an increase of two to three times normal in diabetes.
Clinical picture of a cerebral infarction
The clinical features depend on the site and extent of the infarct, and range from immediate coma and death to minor short-lived clumsiness of a limb. It is helpful to use clinical features to divide cerebral infarctions into two categories: those affecting the circulation to the front of the brain (anterior circulation infarcts) and those affecting the back (posterior circulation infarcts) (→Fig. 4.2).
 |
| Fig. 4.2 |
Anterior circulation infarcts
Anterior circulation infarcts result in the picture of the ‘classic’ stroke with a variable combination of one-sided weakness (hemiparesis), one-sided sensory loss (hemianaesthesia), visual disturbance in the form of a gaze paralysis (the eyes are deviated away from the weak side) and partial loss of the visual field (the patient cannot see towards the weak side). In addition, there is a variable disturbance of higher functions (termed ‘cortical function’): language disturbance (if the dominant side of the brain is damaged), neglect of the affected side and incontinence.
‘Total’ anterior circulation infarct. TACI is a combination of motor or sensory deficit, visual field loss and cortical dysfunction (e.g. language disturbance).
‘Partial’ anterior circulation infarct. PACI consists of any two of:
• unilateral weakness/sensory loss
• visual field defect (hemianopia)
• cortical dysfunction (language disorder or neglect)
Lacunar infarct. LACI consists of very small infarcts within the anterior circulation that pick off single pathways at critical points in the brain. They are particularly associated with a history of hypertension. The clinical picture is of a ‘pure’ one-sided motor or sensory loss.
Posterior circulation infarcts
POCI, also termed a ‘brain stem CVA’, result in symptoms that often affect both sides of the body (the brain stem transmits information to and from both sides of the brain) and characteristically affect coordination in four vital functions: talking, swallowing, looking and balancing. These patients have combinations of dysarthria (slurred speech), dysphagia (difficulty swallowing), double vision and dizziness.
Site of the cerebral infarction and the outlook
Patients who suffer a TACI have a poor outcome: a high initial mortality and high levels of long-term dependence. Patients who have suffered a PACI have a much better outlook, with a low mortality but a high recurrence rate. A LACI is associated with a good outcome, low mortality and a low recurrence rate.
Posterior circulation strokes have the best overall outlook, although the swallowing difficulties need to be managed carefully to prevent the development of aspiration pneumonia. There is also a high recurrence rate.
Transient ischaemic attacks
Transient ischaemic attacks are minor strokes caused by the passage of small emboli that negotiate the cerebral circulation without producing any permanent damage. The clinical picture depends on the route the emboli take and varies from a paralysed or clumsy limb (→Case Study 4.5) to an isolated speech or visual disturbance. By definition the symptoms and signs of TIA last no longer than 24h, but in practice the clinical picture is of an immediate onset with resolution within 5–20min. It is unusual for any deficit to last longer than 1h. Clearly, such short-lived symptoms can be confused with several other conditions, including epilepsy, migraine, hypoglycaemia, syncope and acute vertigo (giddiness).
Case Study 4.5
A man was admitted with episodic weakness of the right arm and leg lasting 5min and associated with difficulties finding the right words. He returned to normal between attacks. During the previous week there had been four or five episodes. He had treated hypertension and a heart murmur. He was otherwise well. Subsequent urgent investigations showed a near total blockage of the right common carotid artery. His hypertension was controlled, and he was started on aspirin and referred for consideration of surgery to the blocked carotid.
The areas of narrowing and roughening within the carotid arteries from which the emboli usually arise can, in time, give rise to a major stroke. Someone who suffers a TIA is at more than 10 times the normal risk of having a major stroke and the risk is highest immediately after the event. As an approximate guide, the chances of a major stroke after a TIA or minor stroke are 8–12% at 7 days and 11–15% at 1 month. Treatment can significantly reduce these chances, but the situation is urgent and systems should be in place for those with TIAs and minor strokes to have specialist assessment within 24–48h.
The ABCD2 scale (→Table 4.2) is used in patients admitted with a TIA, but who have recovered, to identify those at high risk of an early stroke:
| Score | ||
|---|---|---|
| A | age = or > 60 | 1 |
| B | BP > 140/90 | 1 |
| C | Clinical: unilateral weakness | 1 |
| speech only | 1 | |
| other |




