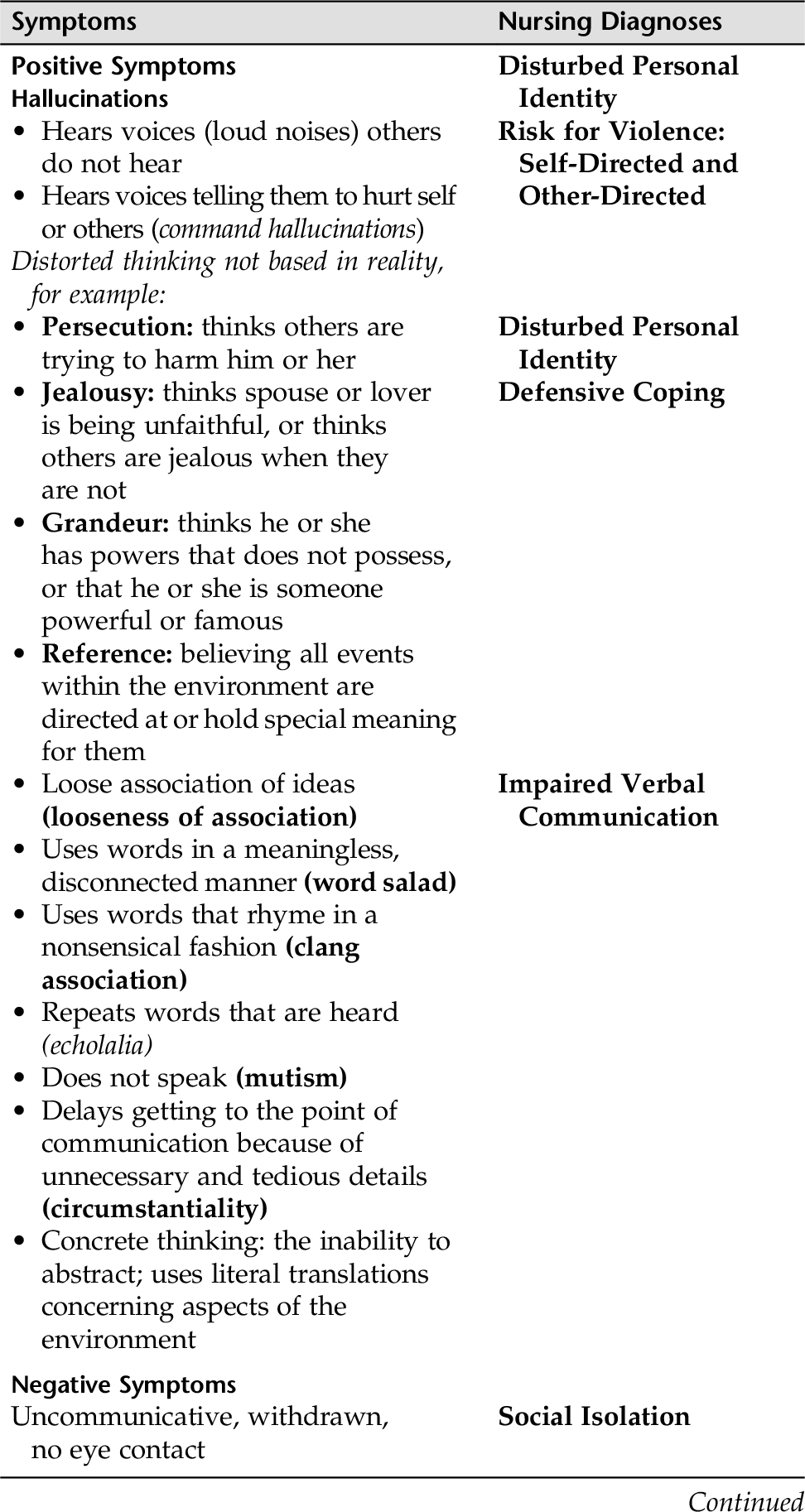
CHAPTER 9 The word psychosis refers to symptoms that include hallucinations (seriously impaired perception, e.g., seeing, hearing, smelling something that is not there), delusions (false beliefs, e.g., paranoid beliefs that people are out to harm them when it is not true), and disorganized thinking as evidenced in behavior and speech. Psychosis is either a primary or secondary psychosis. Primary psychoses have a biological or neurobiological origin. Examples of these disorders are schizophrenia, depression with psychotic features, schizoaffective disorder, bipolar disorder in full-blown mania. Secondary psychoses are referred to as “Psychotic Disorders Due to a General Medical Condition” such as metabolic disorders, head injuries, dementia, intracranial tumors, or drug and alcohol intoxication or withdrawal. The essential features of this disorder are exactly those of schizophrenia, except that: • Symptoms are the same as in schizophrenia but last a much shorter period of time. • Impaired social or occupational functioning during some part of the illness is not apparent (although it might occur). It is difficult to know the prognosis of a schizophreniform disorder because some individuals might return to their previous level of functioning, while others have a more difficulties in moving forward. In this disorder, there is a sudden onset of psychotic symptoms (e.g., delusions, hallucinations, disorganized speech) or grossly disorganized or catatonic behavior. The episode is usually short-lived, and the individual returns to his or her premorbid level of functioning. Brief psychotic disorders often follow extremely stressful life events. This disorder is characterized by an uninterrupted period of illness during which there is a major depressive, manic, or mixed episode, concurrent with symptoms that meet the criteria for schizophrenia. The symptoms must not be caused by any substance use or abuse or general medical condition. This disorder involves nonbizarre delusions (situations that occur in real life, such as being followed, infected, loved at a distance, deceived by a spouse, or having a disease) of at least 1 month’s duration. The person’s ability to function is not markedly impaired, nor is his or her behavior obviously odd or bizarre. Common types of delusions seen in this disorder are delusions of grandeur, persecution, jealousy, or somatic or mixed delusions. A shared delusional disorder is an occurrence in which one individual, who is in a close relationship with another who has a psychotic disorder with a delusion, eventually comes to share the delusional beliefs either in total or in part. This rare problem is known as folie à deux (“the folly of two”). Apart from the shared delusion, the person who takes on the other’s delusional behavior is not otherwise odd or unusual. Impairment of the person who shares the delusion is usually much less than the person who has the psychotic disorder with the delusion. The cult phenomenon is an example, as was demonstrated at Waco and Jonestown. Psychosis can be induced by substances (drugs of abuse, alcohol, medications, or toxin exposure) or caused by the physiological consequences of a general medical condition (delirium, neurological conditions, metabolic conditions, hepatic or renal diseases, and many more). Medical conditions and substances of abuse must always be ruled out before a primary diagnosis of schizophrenia or other psychotic disorder is made. Schizophrenia is a devastating chronic brain disease that is prone to recurring psychotic episodes. It is not a single disease, but rather a syndrome that involves cerebral blood flow, neuroelectrophysiology, neuroanatomy, and neurobiochemistry. The schizophrenias target young people in their teens or early twenties at the beginning of their productive lives (15 to 25 years of age for men, 25 to 35 years of age for women). It profoundly disrupts an individual’s ability to accurately perceive reality, to think clearly, to use language appropriately, to experience normal emotions, or to engage in normal social/occupational experiences. Schizophrenia spectrum disorders are a group of psychotic disorders. The schizophrenias are severe mental illnesses (SMIs), and people with schizophrenia compose a large percentage of our homeless population. The longer the individual with psychoses remains untreated, the poorer the prognoses. Schizophrenia affects approximately 1% of the population, and 95% of individuals who are diagnosed with a schizophrenia continue to suffer with the disorder throughout their lifetime. People who develop paranoid features usually have a later time of onset. Although schizophrenias are not caused by psychological events, stressful life events can trigger an exacerbation of the illness. Some people with schizophrenia function well with the aid of medications and social supports. Others are more disabled and need a higher level of support in terms of housing, health maintenance, monetary aid, and more. Although schizophrenia is treatable, it is not curable. Schizophrenia has been divided into three phases: Phase II—Years following onset. Patterns that characterize this phase are the ebb and flow of the intensity and disruption caused by symptoms, which might in some cases be followed by complete or relatively complete recovery. The core symptoms of schizophrenia are as follows: • Positive symptoms—Delusions, hallucinations, and perceptions that are not based in reality. Individuals with schizophrenia have a profound thought disorder that affects the ability to think clearly or use language appropriately (looseness of association). • Cognitive symptoms—Poverty of thought, poor problem solving, poor decision making, and illogical thinking most profoundly affect the individual’s ability to engage in normal social and occupational experiences. Positive symptom schizophrenia occurs suddenly, and patients have a normal premorbid personality and normal CT findings. Positive symptoms are active and include alterations in: • Perceptions (hallucinations and delusions) • Thinking (delusions, paranoia, disorganized thinking) • Agitation and emotional dyscontrol • Language (looseness of association, poverty of speech) Hallucinations and delusions can be very frightening and are often terrifying for individuals. They also can be very disconcerting initially and frightening to nurses and other health care individuals, as well as family and friends. Communicating with patients who are delusional and hallucinatory and have disorganized thinking is a skill learned with guidance and practice. Negative symptom schizophrenia occurs when there is a neurodevelopmental disorder. Negative symptoms usually begin in childhood. Others often view these children as odd and withdrawn. Symptoms are more insidious and the most damaging to the patient’s quality of life. Negative symptoms include alterations in: • Emotions—apathy, anhedonia, depression, feelings of emptiness, amotivational states • Social behavior—aggression, bizarre conduct or extreme withdrawal Cognitive symptoms are perhaps the most crucial because they interfere with the person’s ability to function in all areas of life (e.g., learn, hold a job, have friends). Cognitive symptoms that are altered in schizophrenia include (APNA, 2012): • Attention/vigilance • Verbal learning and memory • Reasoning and problem-solving • Speed of processing • Social learning/cognition • Co-occurring depression is a frequent complication in people with schizophrenia as is substance use problems and disorders. The Brief Psychiatric Rating Scale (BPRS) (Appendix D-5) is a useful tool for evaluating overall psychiatric functioning. It is particularly helpful in evaluating the degree to which psychotic symptoms affect a person’s ability to function. 1. Do you plan to follow the command? 2. Do you believe the voices are real? B. Assess whether the patient has fragmented, poorly organized, well-organized, systematized, or extensive system of beliefs that are not supported by reality (delusions). If yes: 2. Assess whether precautions need to be taken. 3. Assess for pervasive suspiciousness about everyone and their actions (paranoia), for example: • Is on guard, hyperalert, vigilant • Blames others for consequences of own behavior • Is hostile, argumentative, or often threatening in verbalization or behavior 1. Assess for negative symptoms of schizophrenia (Table 9-1 lists definitions and suggested interventions). 2. Assess whether patient is on medications, what the medications are, and if treatment is adherent with medications. 3. How does the family respond to increased symptoms? Are they overprotective? Hostile? Suspicious? 4. How do family members and patient relate? 5. Assess support system. Is family well informed about the disorder (e.g., schizophrenia)? 6. Does family understand the need for medication adherence? Is family familiar with family support groups in the community or where to go for respite and family support? 1. Assess the severity of the cognitive symptoms 2. Assess how the cognitive symptoms interfere with the patient’s functioning 3. Identify patient’s strengths and personal attributes that can be gateways to interventions People with schizophrenia often have multiple needs. Basic to these is safety. Refer to Chapters 17 and 18 for nursing care plans identifying nursing interventions for suicide intent and violence toward others. Suicide and threat of violence to others are basic to nursing interventions for all patients in all settings, not just for people with schizophrenia or the hospitalized person. Table 9-2 lists potential nursing diagnoses for patients with schizophrenia. Relating to people with schizophrenia can be a challenge, especially in the acute phase; therefore guidelines for Impaired Verbal Communication are included. Again, during the acute phase, relating to others is difficult. Guidelines for interacting and gradually adding social skills are included in Impaired Social Interaction. Because patients with schizophrenia are often unable to distinguish between inner and outer stimuli, they often hear things that are not based in reality (hallucinations), misinterpret the environment, and have false fixed ideas that cannot be corrected by reasoning (delusions). Therefore Disturbed Personal Identity is appropriate. Working with a patient who is paranoid (Defensive Coping) can be a great challenge. Importantly, families are often left to cope with the exhaustive needs of their mentally ill family member. Interrupted Family Processes should always be assessed, and referrals and teaching should be readily available. • Communicates thoughts and feelings in a coherent, goal-directed manner (to patient’s best ability) • Demonstrates reality-based thought processes in verbal communication (to patient’s best ability) Patient will: • Use two diversionary tactics that work for him or her to lower anxiety, thus enhancing ability to think clearly and speak more logically by (date) Patient will: • Spend three 5-minute periods with nurse, sharing observations in the environment within 4 days • Spend time with one or two other people in a structured activity involving neutral topics by (date) • Improves social interaction with family, friends, and neighbors • Engages in social interaction in a goal-directed manner • Uses appropriate social skills in interactions • Seeks out supportive social contacts Patient will: • Engage in one or two activities, with minimal encouragement from nurse or family members by (date) • Use appropriate skills to initiate and maintain an interaction by (date) • State that he or she is comfortable in at least three structured activities that are goal directed by (date) • Demonstrate interest in starting coping skills training when ready for learning Patient will: • Engage in one activity with nurse/family member/friend by the end of each day • Attend one structured group activity within 1 week • Maintain an interaction with another patient while doing an activity (drawing, playing cards, cooking a meal)
Schizophrenia Spectrum and Other Psychotic Disorders
OVERVIEW
Some Primary Psychotic Disorders-DSM-5
Schizophreniform Disorder
Brief Psychotic Disorder
Schizoaffective Disorder
Delusional Disorder
Shared Delusional Disorder (Folie à Deux)
Substance Induced or Secondary Psychosis
Schizophrenia Spectrum Disorders
Phases of Schizophrenia
ASSESSMENT
Presenting Signs and Symptoms
Assessment Tool
Assessment Guidelines
Schizophrenias
Assessing Positive Symptoms
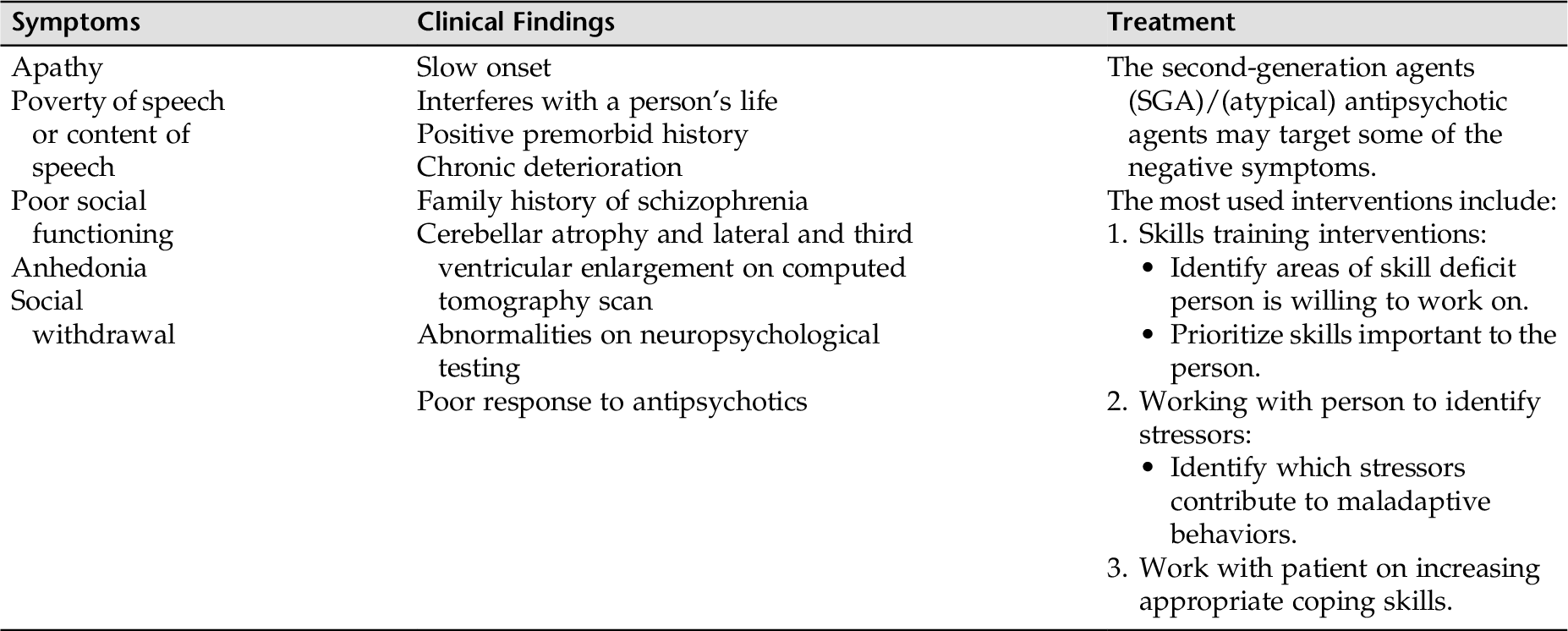
Assessing Negative Symptoms
Assessing Cognitive Symptoms
NURSING DIAGNOSES WITH INTERVENTIONS
Selected Nursing Diagnoses and Nursing Care Plans
Some Related Factors (Related To)
 Psychological barriers (e.g., psychosis, lack of stimuli)
Psychological barriers (e.g., psychosis, lack of stimuli)
 Biochemical alterations in the brain
Biochemical alterations in the brain
Defining Characteristics (As Evidenced By)
 Difficulty expressing thoughts verbally
Difficulty expressing thoughts verbally
 Difficulty comprehending and maintaining the usual communication pattern
Difficulty comprehending and maintaining the usual communication pattern
 Looseness of associations, perseveration, neologisms
Looseness of associations, perseveration, neologisms
 Inability to distinguish internally stimulated thoughts from actual environmental events or commonly shared knowledge
Inability to distinguish internally stimulated thoughts from actual environmental events or commonly shared knowledge
Outcome Criteria
Long-Term Goals
Short-Term Goals
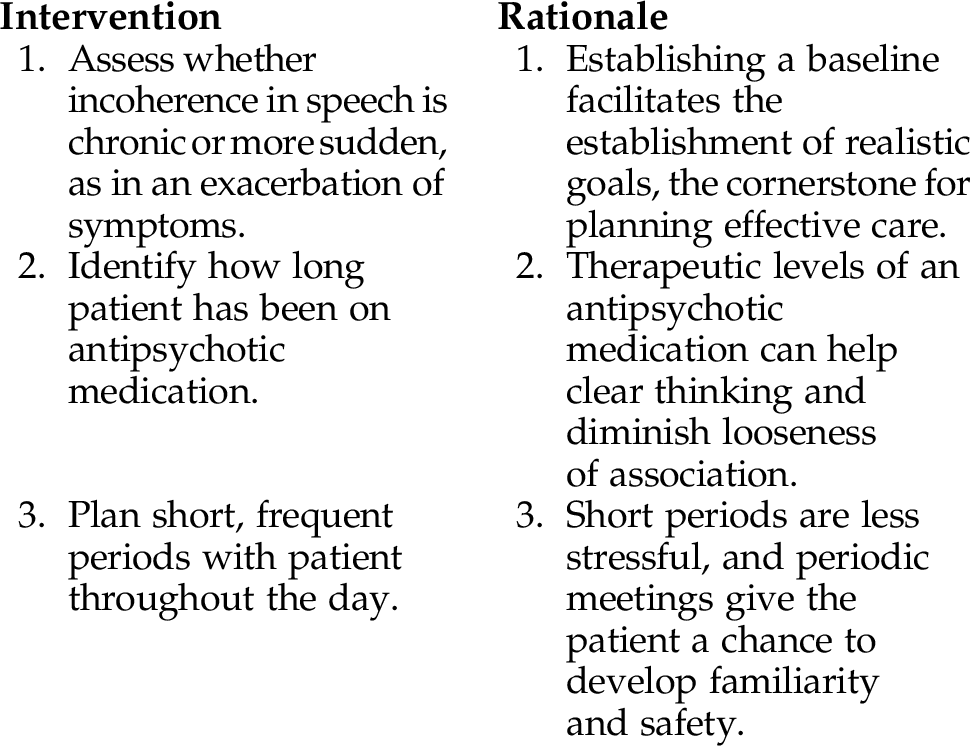
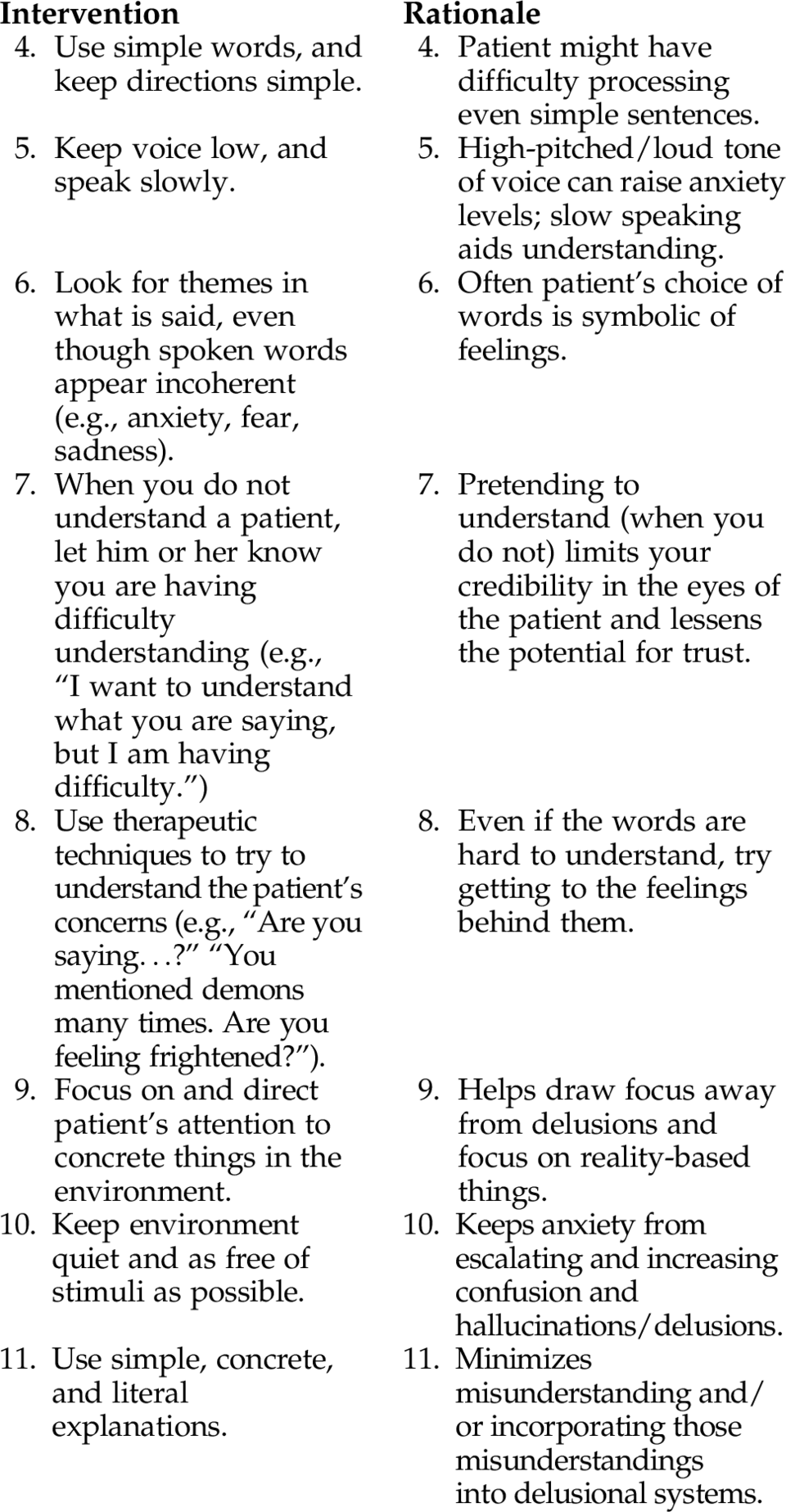
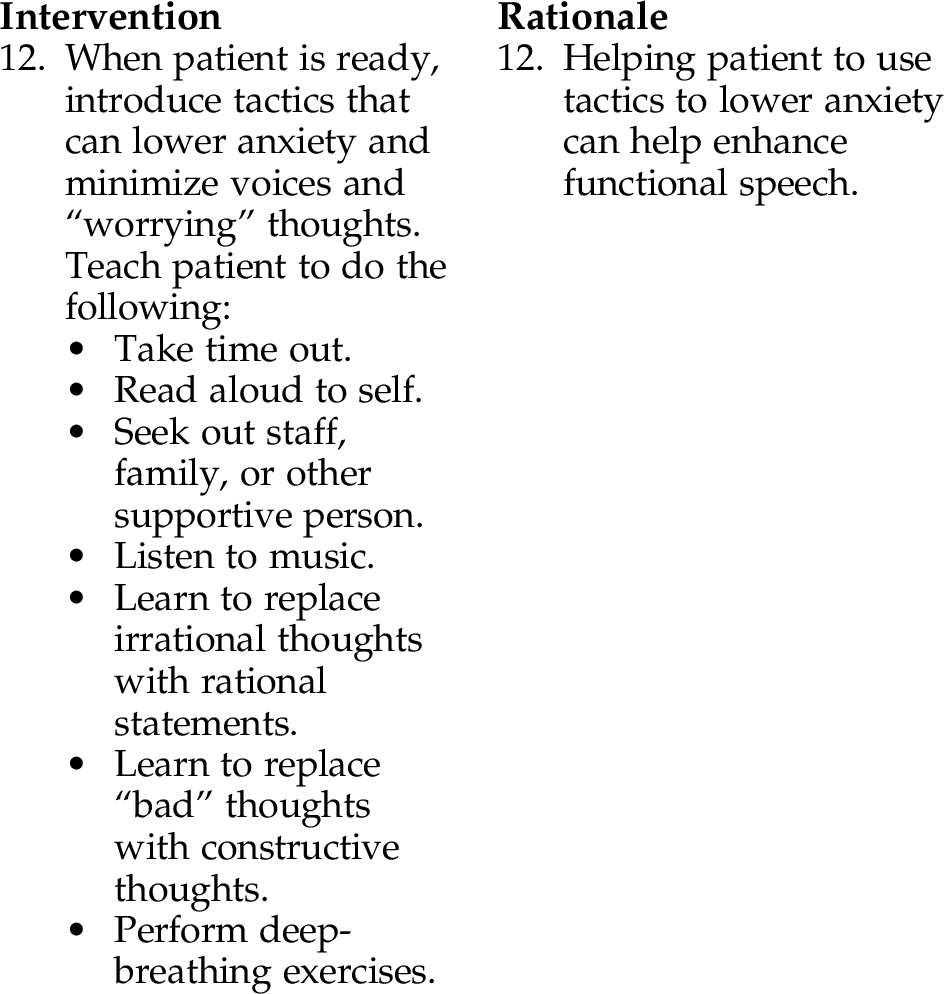
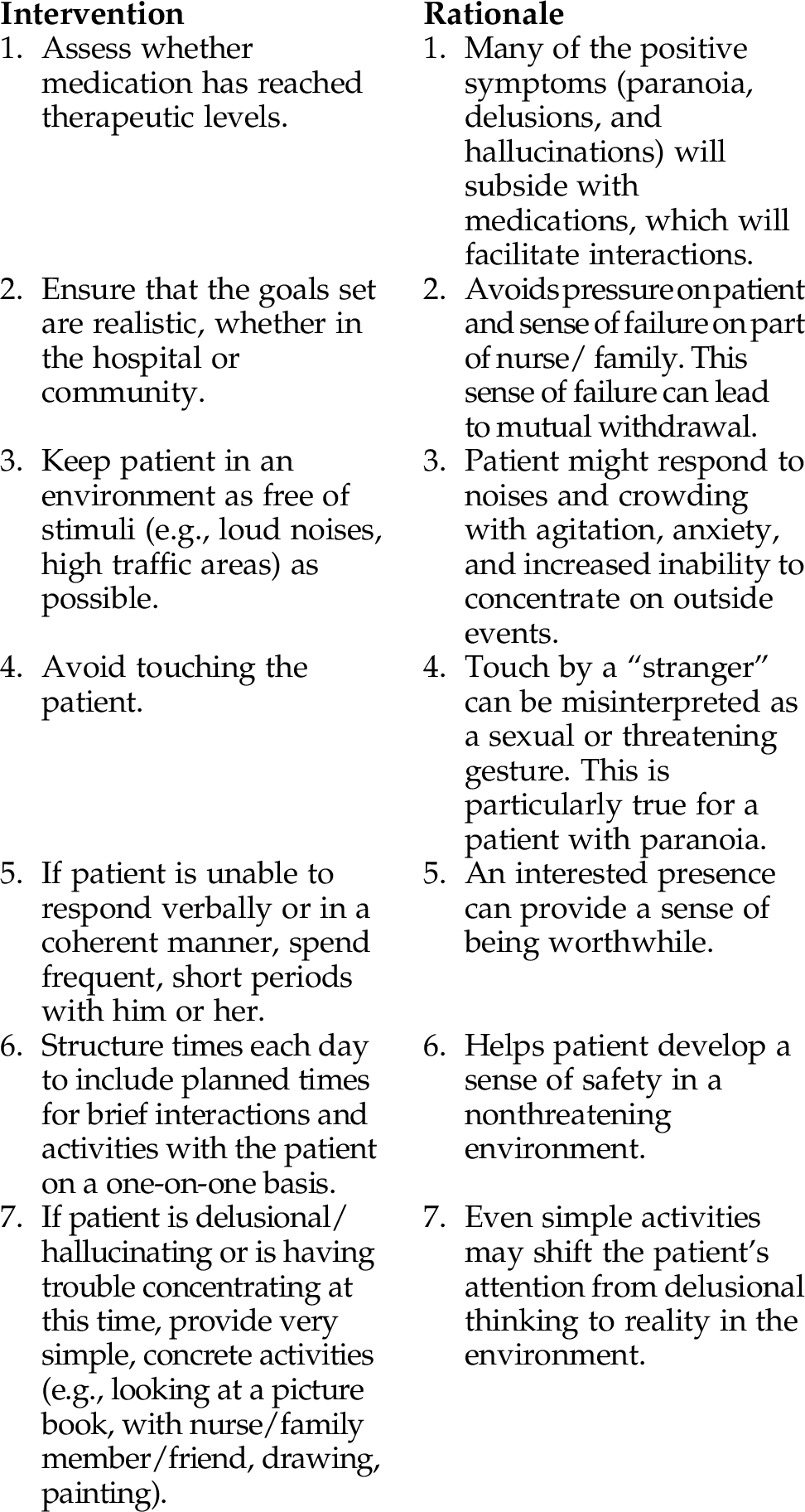
INTERVENTIONS AND RATIONALES
Some Related Factors (Related To)
 Self-concept disturbance (might feel “bad” about self or “no good”)
Self-concept disturbance (might feel “bad” about self or “no good”)
 Difficulty with communication (e.g., looseness of association)
Difficulty with communication (e.g., looseness of association)
 Inappropriate or inadequate emotional responses
Inappropriate or inadequate emotional responses
 Feeling threatened in social situations
Feeling threatened in social situations
 Exaggerated response to stimuli
Exaggerated response to stimuli
 Impaired thought processes (hallucinations or delusions)
Impaired thought processes (hallucinations or delusions)
Some Defining Characteristics (As Evidenced By)
 Discomfort in social situations
Discomfort in social situations
 Use of unsuccessful social interaction behaviors
Use of unsuccessful social interaction behaviors
 Dysfunctional interaction with peers
Dysfunctional interaction with peers
 Inappropriate or inadequate emotional response
Inappropriate or inadequate emotional response
 Does not make eye contact or initiate or respond to social advances of others
Does not make eye contact or initiate or respond to social advances of others
 Appears agitated or anxious when others come too close or try to be engaged in an activity
Appears agitated or anxious when others come too close or try to be engaged in an activity
Outcome Criteria
Long-Term Goals
Short-Term Goals
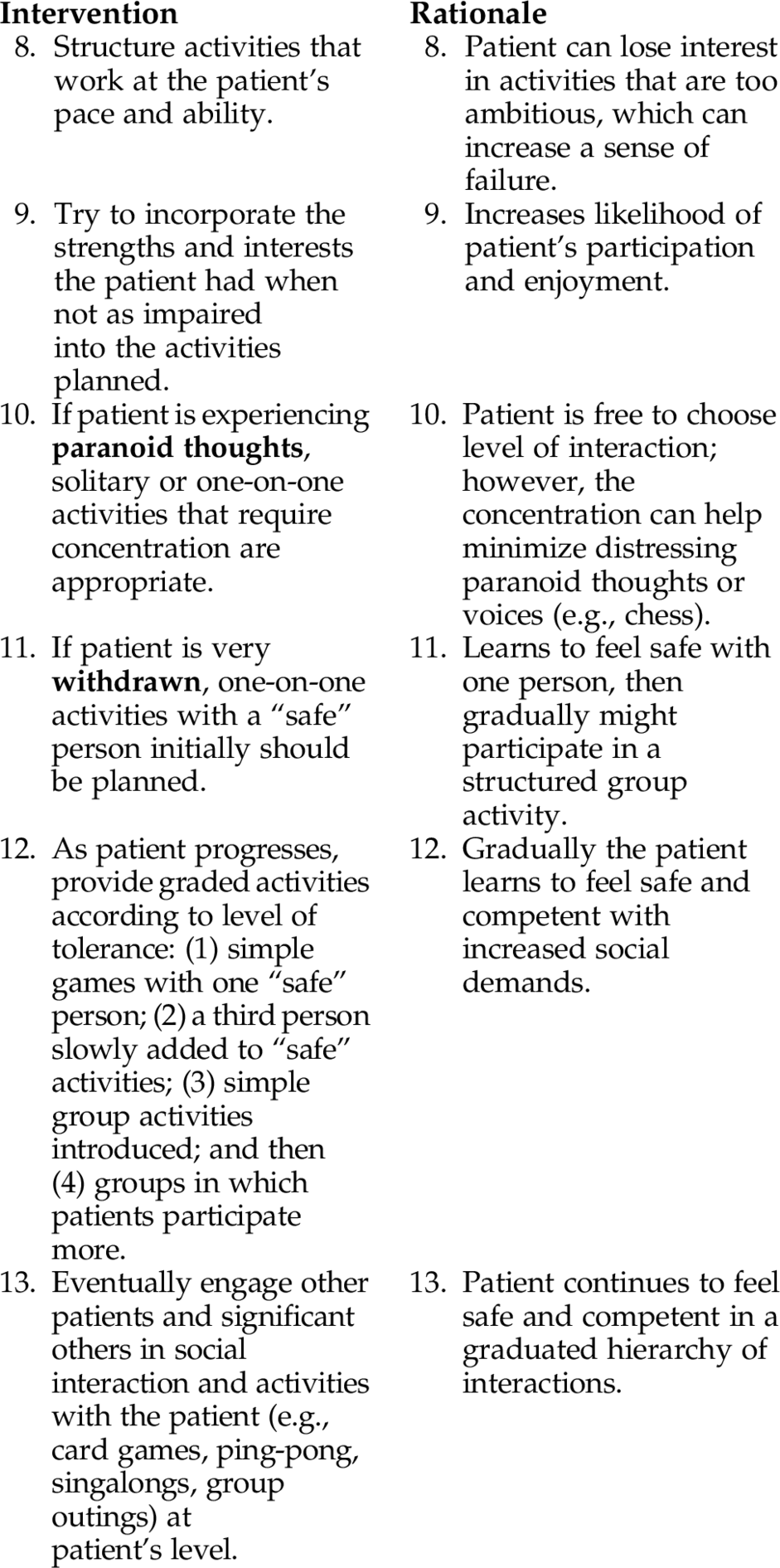
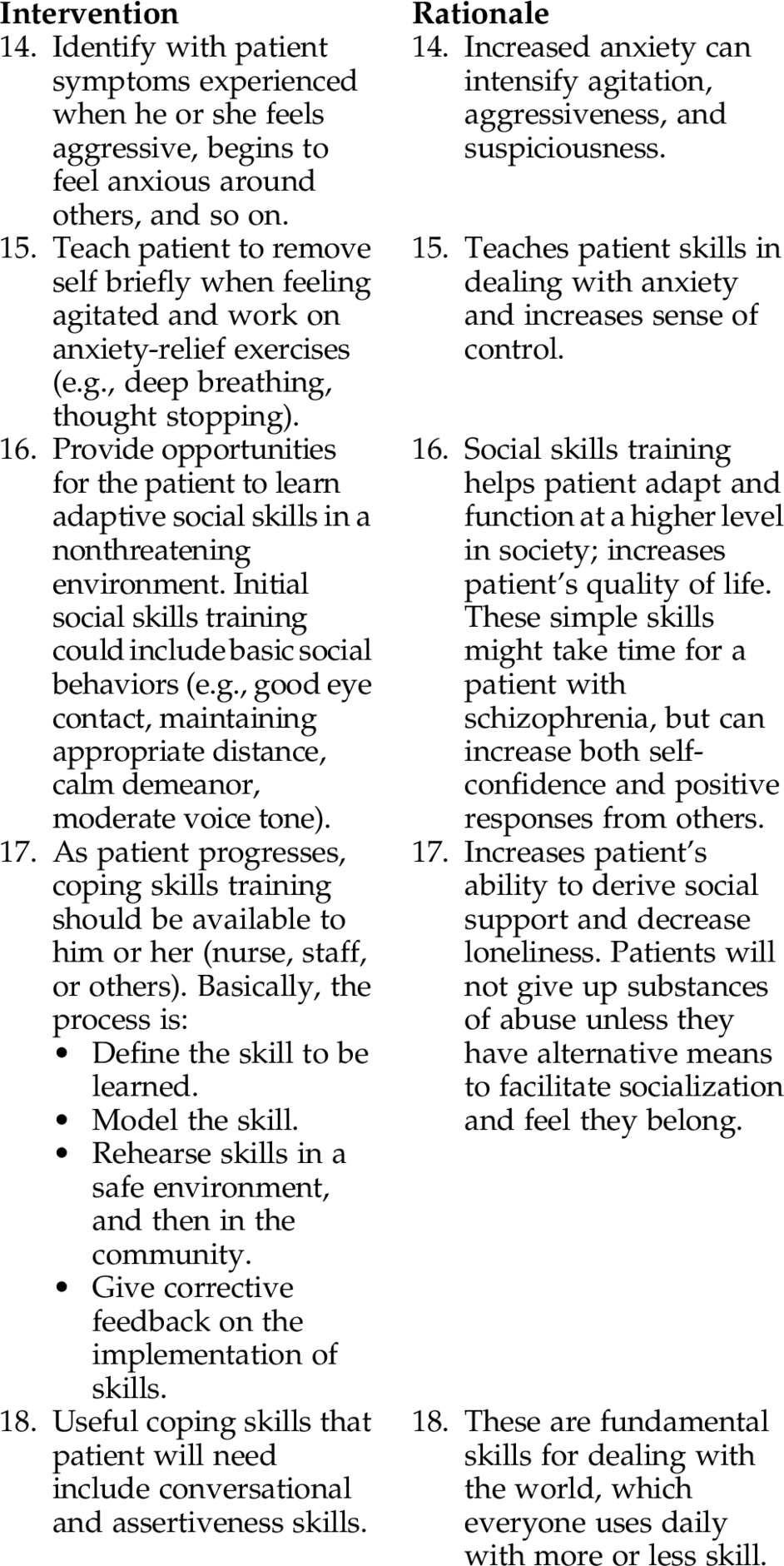
INTERVENTIONS AND RATIONALES
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree