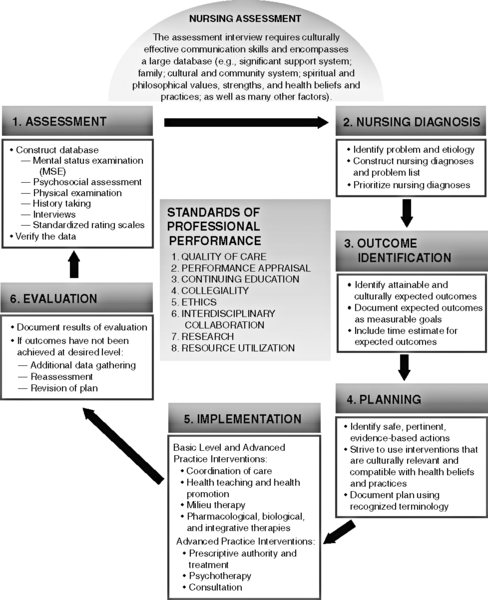
CHAPTER 1 The Diagnostic and Statistical Manual of Mental Disorders (DSM) is the official guidebook for categorizing and diagnosing psychiatric mental health disorders in the USA. The primary objective of the DSM is to provide clinicians, researchers, psychiatric drug regulation agencies, health insurance companies, pharmacological companies and policy makers with a common language and standard criteria for the classification of mental disorders. The DSM is used by clinicians as a guide for planning care and evaluating patients’ treatments. Physicians and researchers have formulated clear and accurate guidelines for identifying and categorizing clinical psychiatric disorders and syndromes. The APA provides specific criteria that must be met before a medical psychiatric diagnosis can be reached. The most current of these criteria are found in the Diagnostic and Statistical Manual of Mental Disorders, fifth edition (DSM-5), Appendix B-3 (APA, 2013). The DSM-5 is the latest manual (2013) since 1952, when the American Psychiatric Association (APA) first published the DSM-I. In each clinical chapter in this manual, characteristics of the major mental disorders are discussed as well as appropriate nursing diagnosis and suggested interventions for each nursing diagnoses pertaining to the disorder. The DSM-5 recommends using the international classification of diseases (ICD-10-Z) codes to identify psychosocial and environmental problems and to assess the global assessment of functioning. Clinicians use WHO Disability Assessment Schedule (WHODAS) for this purpose. A nursing diagnosis is a clinical judgment about individual, family, or community responses to actual or potential health problems/life processes. A nursing diagnosis provides the basis for selection of nursing interventions to achieve outcomes for which the nurse has accountability. (Approved at the ninth NANDA conference; amended in 2009). This manual will help guide you in forming appropriate nursing diagnoses (2012 to 2014) supported by specific assessment data and related factors in order to plan effective and safe care to meet the patient’s need(s). Safety and quality of care for patients has become the new standard for nursing education. The new national and initiatives centered on patient safety and quality of care is known as Quality and Safety Education for Nurses (QSEN), which is outlined in Box 1-1. The Psychiatric–Mental Health Clinical Nursing Practice Standards define the nursing process within the context of six standards of care and the practice of psychiatric nursing (Figure 1-1). Figure 1-1 The nursing process in psychiatric mental health nursing. (From Varcarolis, E. [2012]. Essentials of psychiatric mental health nursing: A communication approach to evidence-based care [2nd ed.]. Philadelphia: Saunders.) The nursing process is the basic framework for nursing practice with patients. The Psychiatric-Mental Health Nursing Scope and Standards of Practice (APNA, ANA, ISPN, 2007) contain the authoritative statements that describe the responsibilities for which nurses are accountable and provide direction for professional nursing practice and a framework for the evaluation of practice. The Psychiatric–Mental Health Clinical Nursing Practice Standards define the nursing process within the context of six standards of care (see Figure 1-1); the following discussion will include some of the QSEN competencies inherent in each step of the nursing process. The psychiatric mental health registered nurse collects comprehensive health data that are pertinent to the patient’s health or situation. In order to effectively assess a patient’s priority of needs, a holistic view of the patient is in keeping with a nurse’s holistic view of care. Whether working in a medical setting or a mental health setting, all nurses need to be aware of psychological, social, cultural, and spiritual issues as well as ethnicity, sexual orientation, and age. Depression, suicidal thoughts, anger, disorientation, delusions, and hallucinations might be encountered in medical-surgical wards, obstetric and intensive care units, outpatient settings, extended-care facilities, emergency departments, community centers, and home settings. Many emotional and/or psychiatric symptoms can be the result of medical/chemical imbalances and disease. The purpose of the assessment is to identify and clearly articulate specific problems in the individual’s life that are causing physical and/or mental disequilibrium or harm. The main purpose of the psychosocial assessment is to: • Obtain an understanding of current problems/illness • Review physical status, and obtain baseline vital signs • Understand how the illness/process has affected the patient’s life (self-esteem, loss of intimacy, role change, change in family dynamics, lifestyle change, and employment issues) • Assess for risk factors affecting the safety of the patient (suicidal, confused, homicidal thoughts); obtain information on previous psychiatric problems or disorder(s) • Assess psychosocial status (social patterns, interests and abilities, stress factors, substance use and abuse, relationship issues, social supports) • Perform a mental status examination (MSE) (Refer to Appendix D-9 for a tool to evaluate mental status.) Formulate a plan of care that meets the requirements of the Quality and Safety Education for Nurses (QSEN) Competencies (see Box 1-1) The basic components of the psychosocial/psychiatric nursing assessment include a patient history and a mental and emotional status evaluation. Because it is always preferable to verify the patient’s data, family members and/or friends and relatives should be a part of the assessment whenever possible. If a police officer is the one who brought the patient into the psychiatric emergency department, it is important for the nurse to know as much as possible about what the patient was doing that warranted police intervention. Past medical and psychiatric history can supply valuable information. This is particularly important if the patient is too psychotic, withdrawn, or agitated to provide a history. In many places, this information might be easily available through the use of informatics (e.g., electronic medical records). Laboratory reports also provide important information. As mentioned, abnormal body chemistry can cause personality changes and violent behavior. For example, abnormal liver enzymes can explain irritability, depression, and lethargy. The use of a standardized nursing assessment tool facilitates the assessment process. For an example of a general assessment tool, refer to Appendix B1. Today most all hospitals and clinics have their own assessment tools. With practice, the nurse becomes proficient in gathering information in an informal fashion, with the nurse clarifying, focusing, and exploring pertinent data with the patient. This method allows patients to state their perceptions in their own words and enables the nurse to observe a wide range of nonverbal behaviors. When the order and the questions on the assessment tool are too rigidly applied, spontaneity is reduced. Assessment is a skill that is learned over time. Practice, supervision, and patience enhance the development of this skill. A personal style of interviewing congruent with the nurse’s personality develops as comfort and experience increase. Box 1-2 is an example of a psychosocial assessment tool for use in the clinical area. Some areas that could be referred to social services and might need further investigation when planning long-term care, especially for patients with severe mental illness (SMI), are as follows: • Problems related to the social environment (death or loss of friends, inadequate social support, living alone, difficulty with acculturation, discrimination, adjustment to life-cycle transition [e.g., retirement]) • Educational problems (illiteracy, academic problems, discord with teachers or classmates, inadequate school environment) • Occupational problems (unemployment, threat of job loss, stressful work schedule, difficult work conditions, job dissatisfaction, job change, discord with boss or co-workers) • Economic problems (extreme poverty, inadequate finances, insufficient welfare support) • Problems with access to health care services (inadequate health care services, transportation to health care facilities unavailable, inadequate health insurance) • Problems related to interaction with the legal system/crime (arrest, incarceration, litigation, victim of crime) Health care providers are increasingly caring for culturally diverse populations, and it has become increasingly evident that providing effective care necessitates interventions that are congruent with the individual’s cultural background. All health care professionals, especially mental health professionals need to increase their knowledge and understanding of the complexity of the cultural and social factors that influence health and illness, and hopefully help mitigate health care workers stereotyping, stigmatizing, and labeling patients. It is especially important to broaden one’s understanding of how health and illness are influenced by culture and social factors. The importance of spirituality and religious beliefs is an often overlooked element of patient care, although numerous empirical studies have suggested that being part of a spiritual community is helpful to people coping with illness and recovering from surgery (Kling, 2011). Spirituality and religious beliefs have the potential to exert an influence on how people understand meaning and purpose in their lives and how they use critical judgment to solve problems (e.g., crises of illness). Box 1-3 provides suggestions for eliciting information that might make your plan of care better adapted to your patient’s needs.
The Nursing Process and Assessment
Standards of Care
MEDICAL DIAGNOSIS VS. NURSING DIAGNOSES
Medical Diagnosis: The Diagnostic and Statistical Manual of Mental Disorders (DSM)
Nursing Diagnoses
The Nursing Process
STANDARD I—ASSESSMENT
ASSESSMENT
Cultural and Social Assessment
Spiritual/Religious Assessment
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


