Enteral Administration
![]() http://evolve.elsevier.com/Clayton
http://evolve.elsevier.com/Clayton
The routes of drug administration can be classified into three categories: enteral, parenteral, and percutaneous. With the enteral route, drugs are administered directly into the gastrointestinal tract by the oral, rectal, percutaneous endoscopic gastrostomy (PEG), or nasogastric (NG) method. The oral route is safe, convenient, and relatively economical, and dose forms are readily available for most medications. In case of a medication error or an intentional drug overdose, much of the drug can be retrieved for a reasonable time after administration. The major disadvantage of the oral route is that it has the slowest and least dependable rate of absorption of the commonly used routes of administration because of frequent changes in the gastrointestinal environment that are produced by food, emotion, and physical activity. Another limitation of this route is that a few drugs (e.g., insulin, gentamicin) are destroyed by digestive fluids and must be given parenterally for therapeutic activity. This route should not be used if the drug may harm or discolor the teeth or if the patient is vomiting, has gastric or intestinal suction, is likely to aspirate, or is unconscious and unable to swallow.
For patients who cannot swallow or who have had oral surgery, the NG or PEG method may be used. The primary purpose of the NG method is to bypass the mouth and the pharynx. Advantages and disadvantages are similar to those of the oral route. The irritation caused by the tube in the nasal passage and throat must be weighed against the relative immobility associated with continuous intravenous (IV) infusions, the expense, and the pain and irritation of multiple injections. For patients who require long-term NG methods, a permanent gastrostomy tube is placed for ongoing drug and feeding administration.
The administration of drugs via the rectal route has the advantages of bypassing the digestive enzymes and avoiding the irritation of the mouth, the esophagus, and the stomach. It may also be an acceptable alternative when nausea or vomiting is present. Absorption via this route varies depending on the drug product, the ability of the patient to retain the suppository or enema, and the presence of fecal material.
Administration of Oral Medications
Objectives
Key Terms
Dose Forms
Capsules
Capsules are small, cylindrical, gelatin containers that hold dry powder or liquid medicinal agents (Figure 9-1). They are available in a variety of sizes, and they are a convenient way of administering drugs that have an unpleasant odor or taste. They do not require coatings or additives to improve the taste. The color and shape of the capsules as well as the manufacturer’s symbol on the capsule surface are means of identifying the product.
Timed-Release Capsules
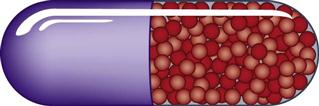
Timed-release or sustained-release capsules provide a gradual but continuous release of a drug, because the granules in the capsule dissolve at different rates (Figure 9-2). The advantage of this delivery system is that it reduces the number of doses administered per day. Trade names that indicate that the drug is a timed-release product are Spansules, Gyrocaps, and Contin.
Lozenges or Troches
Lozenges are flat disks that contain a medicinal agent in a suitably flavored base. The base may be a hard sugar candy or a combination of sugar with sufficient gelatinous substances to give it form. Lozenges are held in the mouth to dissolve slowly, thereby releasing the therapeutic ingredients.
Pills
Pills are an obsolete dose form that is no longer manufactured because of the development of capsules and compressed tablets. However, the term is still used to refer to tablets and capsules.
Tablets
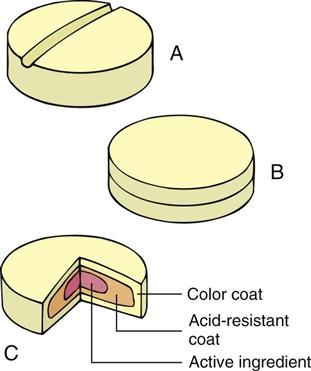
Tablets are dried powdered drugs that have been compressed into small disks. In addition to the drug, tablets also contain one or more of the following ingredients: binders, which are adhesive substances that allow the tablet to hold together; disintegrators, which are substances that encourage dissolution in body fluids; lubricants, which are required for efficient manufacturing; and fillers, which are inert ingredients that make the size of the tablet convenient. Tablets are sometimes scored or grooved (Figure 9-3, A); the indentation may then be used to divide the dose. When possible, it is best to request that the exact dose be prescribed rather than to attempt to divide even a scored tablet.
Tablets can be formed in layers (see Figure 9-3, B). This method allows otherwise incompatible medications to be administered at the same time.
An enteric-coated tablet has a special coating that resists dissolution in the acidic pH of the stomach but that is dissolved in the alkaline pH of the intestines (see Figure 9-3, C). Enteric-coated tablets are often used for administering medications that are destroyed by an acid pH.
A tablet that rapidly dissolves (usually within seconds) when placed on the tongue is known as an orally disintegrating tablet. These are differentiated from lozenges and from sublingual and buccal tablets, which take more than a minute to dissolve. Orally disintegrating tablets may be used for their rapid onset of action (e.g., for the treatment of migraine headache); for patients who have difficulty swallowing (e.g., patients with parkinsonism, Alzheimer’s disease, or after a stroke); and for those for whom administration must be ensured (e.g., patients with schizophrenia, who often attempt to avoid prescribed medication).
Elixirs
Elixirs are clear liquids that are made up of drugs that have been dissolved in alcohol and water. Elixirs are used primarily when the drug will not dissolve in water alone. After the drug is dissolved in the elixir, flavoring agents are often added to improve taste. The alcohol content of elixirs is highly variable, depending on the solubility of the drug.
Emulsions
Emulsions are dispersions of small droplets of water in oil or of oil in water. The dispersion is maintained by an emulsifying agent such as sodium lauryl sulfate, gelatin, or acacia. Emulsions are used to mask bitter tastes or to make certain drugs more soluble.
Suspensions
Suspensions are liquid dose forms that contain solid, insoluble drug particles dispersed in a liquid base. All suspensions should be shaken well before administration to ensure the thorough mixing of the particles.
Syrups
Syrups contain medicinal agents that have been dissolved in a concentrated solution of sugar, usually sucrose. Syrups are particularly effective for masking the bitter taste of a drug. Many preparations for pediatric patients are syrups, because children tend to like the flavored base.
Equipment
Unit Dose or Single Dose
Unit-dose packaging or single-dose packaging provides a single dose of medication in one package that is ready for dispensing (Figure 9-4). The package is labeled with both the generic and brand names, the manufacturer, the lot number, and the date of expiration. Depending on the distribution system, the patient’s name may be added to the package by the pharmacy. Most unit-dose package labels include a bar code for administration, the electronic charting of medication administration, and inventory control (Figure 9-5).

Soufflé Cup
A soufflé cup is a small paper or plastic cup that is used to transport solid medication forms such as capsules and tablets to the patient to prevent contamination by handling (Figure 9-6). A tablet that must be crushed can be placed between two soufflé cups and then crushed with a pestle. This powdered form of the tablet can then be administered in a solution, if soluble, or it may be mixed with a small amount of food (e.g., applesauce).

Medicine Cup
A medicine cup is a plastic container with scales (metric, household) for measuring liquid medications (Figure 9-7). Examine the medicine cup carefully before pouring any medication to ensure that the proper scale is being used for measurement (Table 9-1). The medicine cup should be placed on a hard surface when measuring liquid medication and then read at eye level. The medicine cup is inaccurate for measuring doses of less than 1 teaspoon, although it is reasonably accurate for larger volumes. A syringe comparable to the volume to be measured should be used for smaller volumes. For volumes of less than 1 mL, a tuberculin syringe should be used.
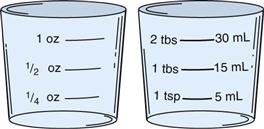
Table 9-1
Commonly Used Measurement Equivalents
| HOUSEHOLD MEASUREMENT* | METRIC MEASUREMENT |
| 2 Tbsp | 30 mL |
| 1 Tbsp | 15 mL |
| 2 tsp | 10 mL |
| 1 tsp | 5 mL |
tbsp, Tablespoon; tsp, teaspoon; oz, ounce; mL, milliliter.
Medicine Dropper
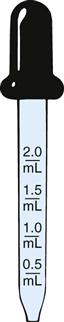
The medicine dropper may be used to administer eyedrops, eardrops, and, occasionally, pediatric medications (Figure 9-8). There is great variation with regard to the size of the drop formed, so it is important to use only the dropper supplied by the manufacturer for a specific liquid medication. Before drawing medication into a dropper, it is necessary to become familiar with the calibrations on the barrel. After the medication is drawn into the barrel, the dropper should not be tipped upside down, because the medication will run into the bulb, thereby causing some loss of the medication. Medications should not be drawn into the dropper and then transferred to another container for administration, because part of the medication will adhere to the second container, thus diminishing the dose delivered.
Teaspoon
Doses of most liquid medications are prescribed in terms using the teaspoon as the unit of measure (Figure 9-9). However, there is great variation between the volumes measured by various spoons in the home. In the hospital, 1 teaspoon is converted to 5 mL (see Table 9-1), and this is read on the metric scale of the medicine cup. For home use, an oral syringe is recommended. If this is not available, a teaspoon that is used specifically for baking may be used as an accurate measuring device.
Oral Syringe
A plastic oral syringe may be used to measure liquid medications accurately (Figure 9-10). Various sizes are available to measure volumes from 0.1 to 15 mL. Note that a needle will not fit on the tip.

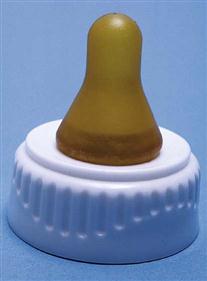
Nipple
An infant feeding nipple with additional holes may be used for administering oral medications to infants (Figure 9-11). (See also “General Principles of Liquid-Form Oral Medication Administration—For an Adult or Child” on p. 132.)
Administration of Solid-Form Oral Medications
Objective
Procedure Protocol
The term procedure protocol will be used as part of the medication administration technique for this text. This term includes the following nursing interventions:
1 Perform hand hygiene, and assemble the equipment.
2 Use the seven RIGHTS of medication preparation and administration throughout the procedure.
3 Provide privacy for the patient, and thoroughly explain the procedure.
4 Perform a premedication assessment; see the individual drug monographs for details.
Medication Card System
Perform premedication assessment. See individual drug monographs for details.
Equipment
Technique
1 Follow the procedure protocol described.
2 Read the entire medication card.
3 Obtain the prescribed medication from the cabinet.
5 Transfer the correct number of tablets or capsules from the lid to a soufflé cup or a medicine cup.
7 Replace the lid of the container.
8 RECHECK the SEVEN RIGHTS of the medication order.
9 Return the medication container to the shelf in the cabinet.
11 Go to the patient’s bedside when all medications are assembled for administration.
• Check pertinent patient monitoring parameters (e.g., apical pulse, respiratory rate).
Unit-Dose System
Perform premedication assessment. See individual drug monographs for details.
Equipment
Technique
1 Follow the procedure protocol described.
2 Read the patient medication profile for drugs prescribed and times of administration.
7 Proceed to the patient’s bedside:
• Check pertinent patient monitoring parameters (e.g., apical pulse, respiratory rate).
8 Hand the medication to the patient, and allow him or her to read the package label.
Electronic Control System
Perform premedication assessment. See individual drug monographs for details.
Equipment
Technique
1 Follow the procedure protocol described on the facing page.
2 Obtain and read the medication profile for the prescribed drugs and the time of administration.
3 Access the computerized medication system using the security access code and password.
4 Select the patient’s name from the list of patients on the unit.
5 Review the patient’s on-screen profile, and select the medications to be administered at this time.
6 Check all aspects of the on-screen order against the medication profile.
9 Proceed to the patient’s bedside.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


 ) (
) ( ) (
) ( ) (
) ( ) (
) ( ) (
) ( ) (
) ( ) (
) ( ) (
) ( ) (
) ( ) (
) ( ) (
) ( ) (
) ( ) (
) ( ) (
) (