Chronic Illness and Rehabilitation
Objectives
1. Define relevant nursing issues for patients with chronic illness.
2. Distinguish patients at risk for problems associated with immobility.
3. Describe the effect of immobility on each of the major systems of the body.
4. Explain the general goals for the resident in a long-term care facility and how to meet those goals.
5. Compare the role of the LPN/LVN in a long-term care facility of that in the hospital setting.
6. Describe the types of rehabilitation programs that might be found in a large city.
7. Apply the goals of rehabilitation.
3. Observe a rehabilitation team conference to see how a collaborative care plan is created or updated.
4. From assessment data, identify areas of psychosocial need for a home care patient and family.
Key Terms
disability (dĭs-ă-BĬL-ĕ-tē, p. 177)
handicap (HĂN-dē-kăp, p. 177)
hemiparesis (hĕm-ē-pă-RĒ-sĭs, p. 187)
impairment (ĭm-PĂR-mĕnt, p. 177)
orthostatic hypotension (ōr-thō-STĀT-ĭk hī-pō-TĔN-shŭn, p. 183)
rehabilitation (rē-hă-bĭl-ĭ-TĀ-shŭn, p. 187)
sundowning (SŬN-doun-ĭng, p. 186)
 http://evolve.elsevier.com/deWit/medsurg
http://evolve.elsevier.com/deWit/medsurg
Patients with chronic illnesses and disabilities are cared for in long-term care facilities, rehabilitation institutes, at home, at outpatient clinics, at rehabilitation agencies, and in physicians’ offices. When working with patients who have a chronic illness, or who are disabled, nurses need to be skilled in providing care and comfort, promoting coping skills and adaptive living capabilities, promoting self-care for independent living, and fostering quality of life.
Chronic Illness
Chronic illness affects millions of people. Diabetes, hypertension, heart disease, cancer, neurologic disorders (such as multiple sclerosis and stroke), asthma, arthritis, back disorders, and musculoskeletal deformities (such as those from arthritis and osteoporosis) all require continuous care. Although many people with a chronic illness can lead an active and productive life, about 46 million people in the United States have chronic illnesses or disabilities that interfere with normal function. People, and particularly the elderly, may have more than one chronic illness, which makes treatment and care very complicated. Many health insurance companies have a case management department that oversees services for those with chronic illnesses. The terms impairment, disability, and handicap are encountered with patients who have a chronic illness. Impairment refers to dysfunction of a specific organ or body system. Disability indicates a difficulty in performing certain tasks because of impairment, and having a handicap means that there is a physical or mental defect or characteristic that prevents or restricts a person from participating in a normal life or limits the capacity to work; a handicap is usually related to a disability.
When chronic illness causes the loss of function, usual roles may be changed. The person may no longer be able to be the primary breadwinner, or hold whatever positions in the workforce or community that formerly were held. Changes in the person’s role affect the family as well. Daily patterns are altered to accommodate treatments and therapy and to cope with the problems of disability. Sorrow is felt for all that has been lost. The patient may wonder, why did this happen to me? Spiritual distress may be experienced as the person is faced with the limitations of the illness or disability that has occurred. Holistic care that addresses spiritual and psychosocial needs as well as physical needs is essential.
Patients with a chronic illness often feel powerless, especially during the phases of diagnosis and early treatment. Patients realize that the chronic illness will dictate much of their course in life now, and that they have less control over what is happening to their body. Support of usual coping techniques—and teaching new ways to cope—help the patient effectively deal with the illness and the changes in life patterns it brings. Nurses can be instrumental in instilling hope for a good quality of life, despite the illness.
Preventing the Hazards of Immobility
Patients are immobilized to varying degrees and for different amounts of time. The multiple trauma patient may be on bed rest for several weeks. The patient with advanced multiple sclerosis may be able to move around only with a wheelchair. The patient who experiences great difficulty breathing from advanced lung disease or heart disease may have very little energy and does not move around much for that reason. Patients with spinal cord injury or brain damage from a stroke may be immobile for the rest of their lives. Patients who have pain or who have arthritic joints that cause pain with movement also tend to be less mobile. Patients who have any disorder requiring bed rest are at risk. All of these patients are subject to the problems of immobility.
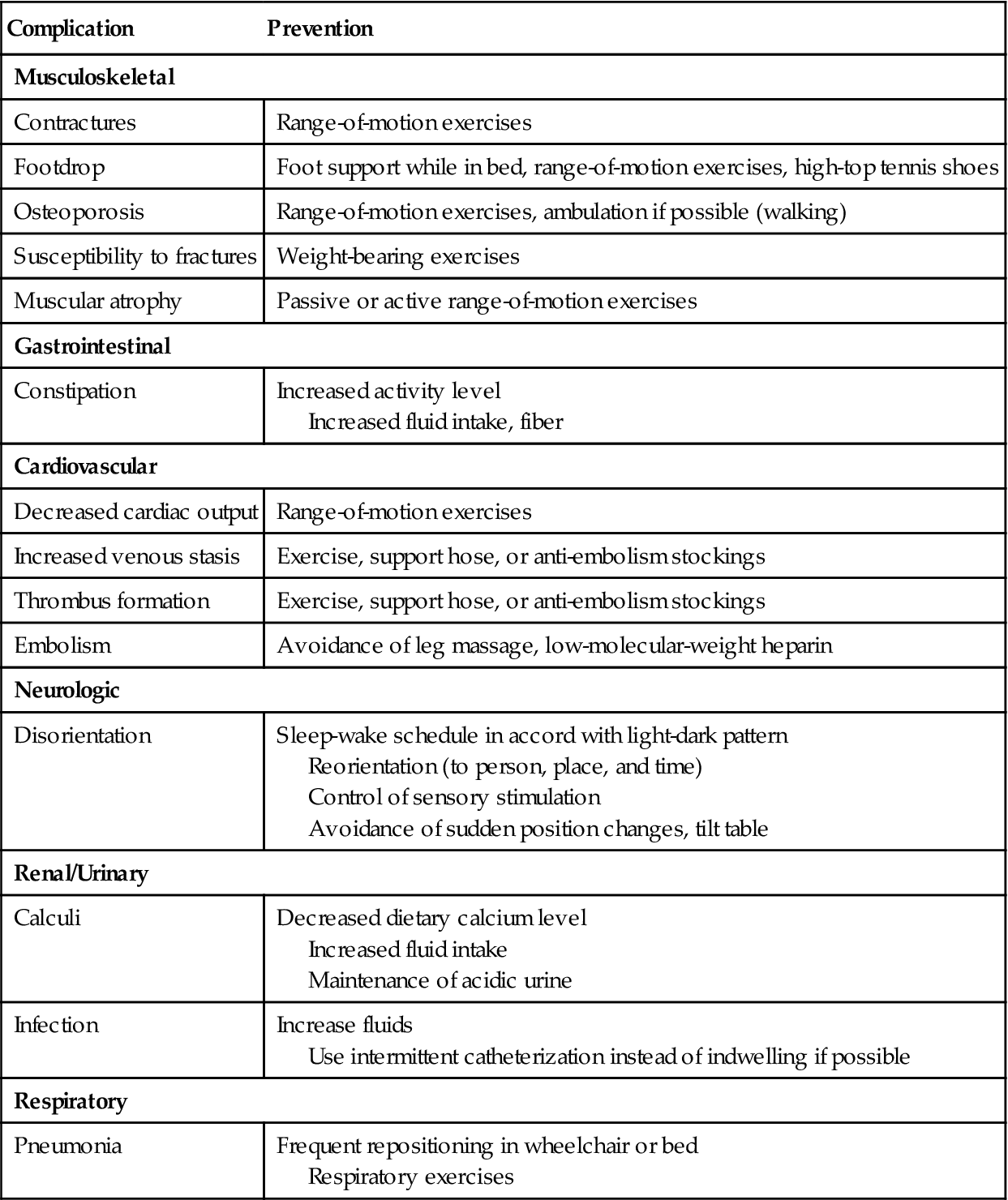
Evaluate each patient situation and determine whether the patient is at risk for problems related to immobility. Even if the patient is going to be immobile for only a few days, measures should be taken to prevent secondary problems. Patients with disorders causing immobility should be assessed for the degree of risk for the various problems of immobility, and interventions to prevent them should be initiated (Box 9-1). Early effects of immobility include a decrease in muscle strength, generalized weakness, easy fatigue, joint stiffness, decreased coordination, abdominal distention, and various metabolic changes detectable by laboratory test. Table 9-1 presents the more severe problems with measures for prevention when lack of activity occurs for more than a few days.
Table 9-1
Prevention of the Common Hazards of Immobility
| Complication | Prevention |
| Musculoskeletal | |
| Contractures | Range-of-motion exercises |
| Footdrop | Foot support while in bed, range-of-motion exercises, high-top tennis shoes |
| Osteoporosis | Range-of-motion exercises, ambulation if possible (walking) |
| Susceptibility to fractures | Weight-bearing exercises |
| Muscular atrophy | Passive or active range-of-motion exercises |
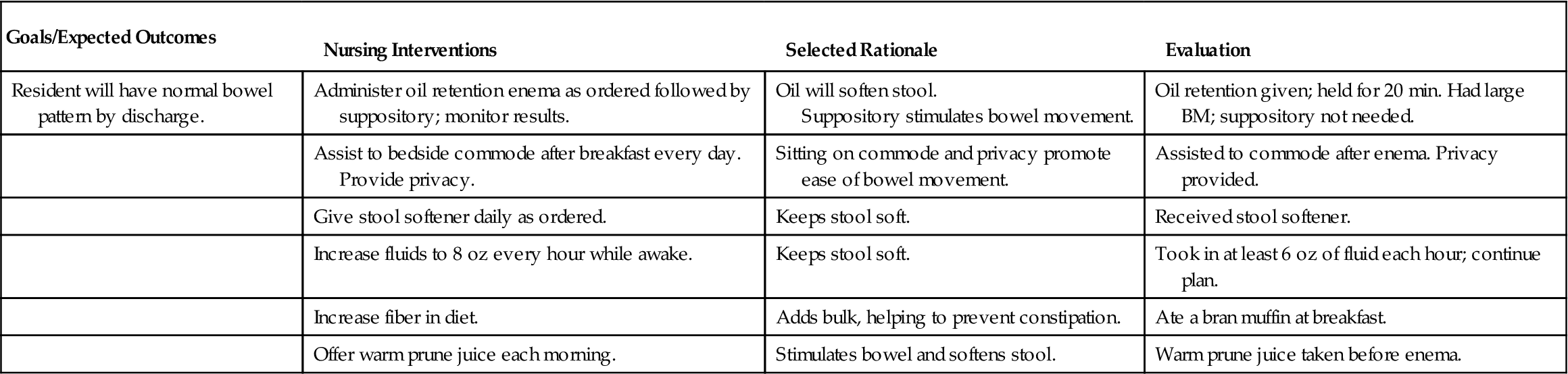
| Gastrointestinal | |
| Constipation | Increased activity level Increased fluid intake, fiber |
| Cardiovascular | |
| Decreased cardiac output | Range-of-motion exercises |
| Increased venous stasis | Exercise, support hose, or anti-embolism stockings |
| Thrombus formation | Exercise, support hose, or anti-embolism stockings |
| Embolism | Avoidance of leg massage, low-molecular-weight heparin |
| Neurologic | |
| Disorientation | Sleep-wake schedule in accord with light-dark pattern Reorientation (to person, place, and time) Control of sensory stimulation Avoidance of sudden position changes, tilt table |
| Renal/Urinary | |
| Calculi | Decreased dietary calcium level Increased fluid intake Maintenance of acidic urine |
| Infection | Increase fluids Use intermittent catheterization instead of indwelling if possible |
| Respiratory | |
| Pneumonia | Frequent repositioning in wheelchair or bed Respiratory exercises |
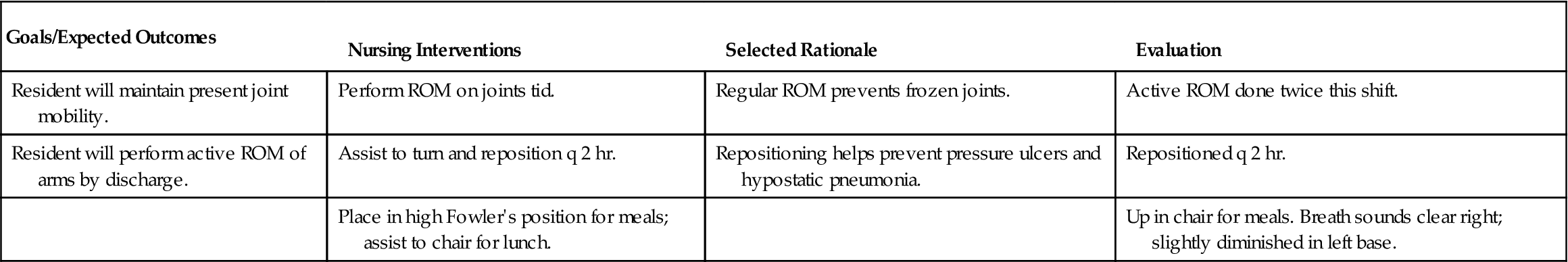
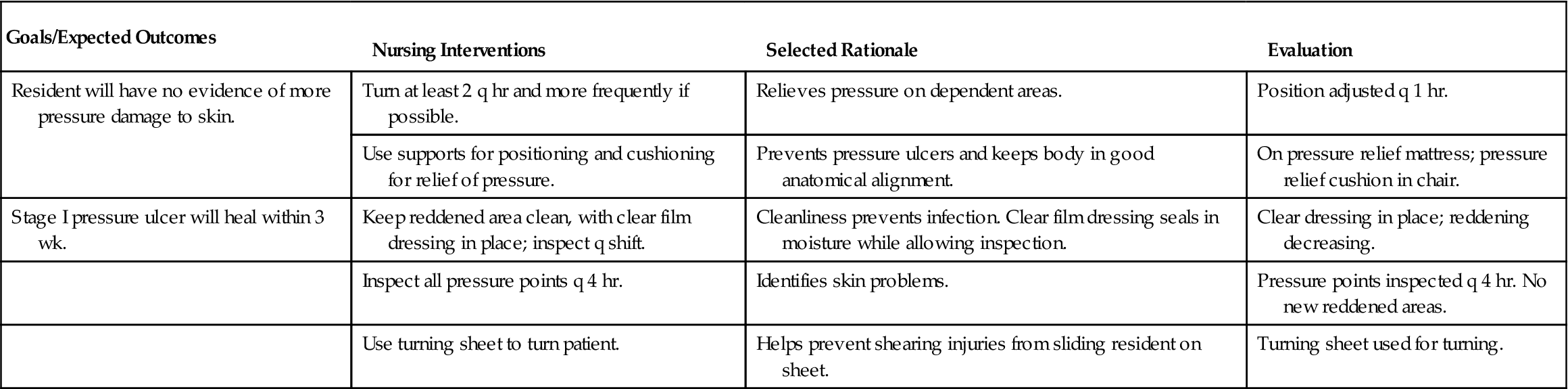
The prevention of problems related to immobility begins the moment a patient first becomes ill or injured. Preventive actions must continue as long as the patient needs health care. The systems of the body work together as a whole and lack of activity affects more than one system. The effects vary depending on the general health of the individual, his age, the degree of immobility, and the length of time of inactivity or bed rest. Lack of mobility may begin a cycle that leads to an ever-increasing loss of independence for the patient. As he becomes less able to move, the patient becomes more dependent, and as he becomes more dependent, he is less able to care for himself—which in turn leads to even more adverse effects from immobility. It is the nurse’s responsibility to avoid the beginning of such a cycle by helping the patient maintain normal functioning of each body system to the highest degree possible (see Nursing Care Plan 9-1 on pp. 180–182).
Assess the patient daily, looking closely at each body system in which a problem related to immobility might occur. Know the signs and symptoms of each type of problem and understand how to intervene to decrease or prevent it. The pathophysiology of the problems of immobility, including the signs and symptoms, medical treatment, and nursing care for each problem, is discussed in the relevant chapters of this text.
Chronic Illness and Rehabilitation Care
A chronic illness may develop following an acute illness or an accident. Some patients are transferred to a transitional unit or long-term care facility for a period of weeks for recovery after the most acute phase of illness or injury has passed. Many elderly, who have several chronic problems and deficits in self-care, enter long-term care facilities for the remainder of their lives. Other patients may enter a rehabilitation facility for an extended time. Some patients are discharged home to continue with rehabilitation services as an outpatient.
Long-Term Care
In the long-term care facility, an RN usually is the director of nurses. The RN supervisor manages the care for the entire facility on a 24-hour basis and delegates tasks to the LPN/LVN. An LPN/LVN often is the charge nurse, and certified nursing assistants (CNAs), patient care assistants, or restorative aides provide much of the basic direct care to the residents. An occupational therapist, physical therapist, speech pathologist, respiratory therapist, activity therapist, or other professional provides services as needed. A physician or advanced practice nurse supervises each resident’s care program. Although the RN ultimately is responsible for the nursing care plan of each resident, the LPN/LVN charge nurse often is the person who admits the resident and initiates the plan of care. If the LPN/LVN initiates a plan of care, collaboration with the RN is necessary to ensure that the plan is appropriate and complete. The LPN/LVN performs treatments and wound care, regularly assists with gathering assessment data from the residents, organizes the shift’s workload, administers medications, documents assessment findings and care given, assists with updating the nursing care plans, and assigns care tasks to patient care assistants. The LPN/LVN oversees care for a group of residents for a shift. The LPN/LVN assigns tasks to the patient care assistants. Those tasks may include assistance with toileting,
bathing, feeding, ambulation, or range-of-motion (ROM) exercises; care of the resident unit; and transfer of residents from bed to chair. Patient care assistants are the core caregivers of the long-term care facility. The skillful LPN/LVN will establish rapport, harmony, and respect among the work team by valuing these workers, appreciating their contributions, and listening to their concerns.
When planning care for residents in a long-term care facility, the LPN/LVN must keep in mind that the overall goals of care for the facility are to provide a safe environment, assist the resident to maintain or attain as much function as possible, promote individual independence, and allow the resident to maintain or achieve as much autonomy as possible.
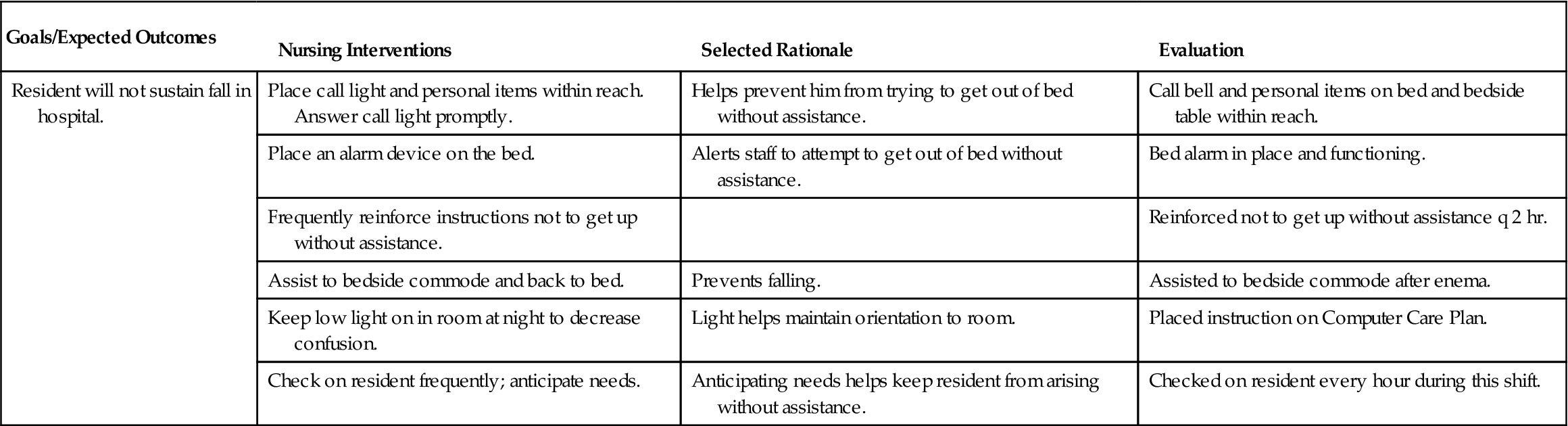
Safety
Providing a safe environment for a group of residents, many of whom may not be totally mentally competent, while allowing autonomy and independence is a great challenge. Two of the greatest safety concerns are to keep confused residents within the boundaries of the facility and to prevent falls. Those with physical disabilities need extra measures to ensure safety. National Patient Safety Goals (The Joint Commission [TJC], 2011) have been developed specifically for long-term care and rehabilitation facilities (Box 9-2). Meeting resident safety and independence needs without resorting to chemical or physical restraints requires caring, commitment, and ingenuity on the part of the nurse.



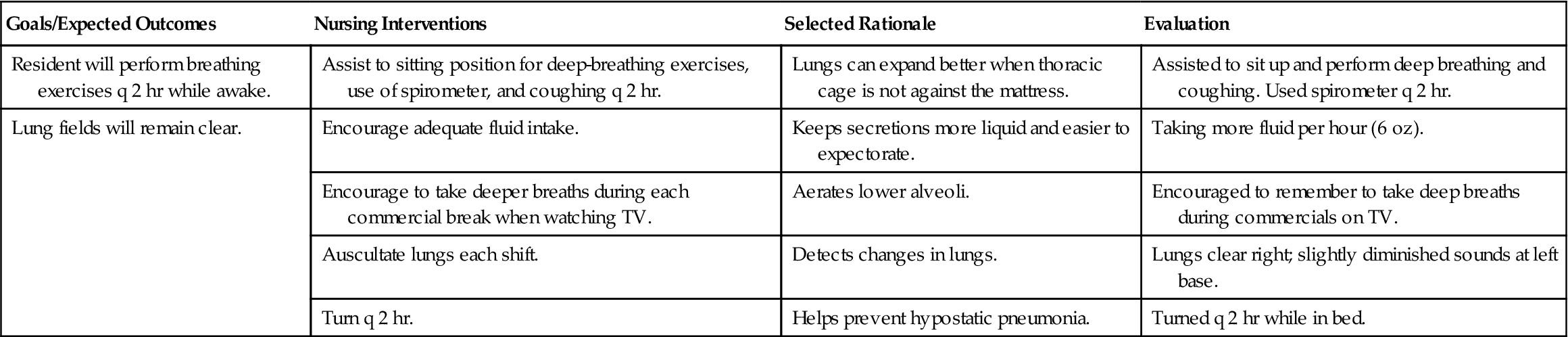
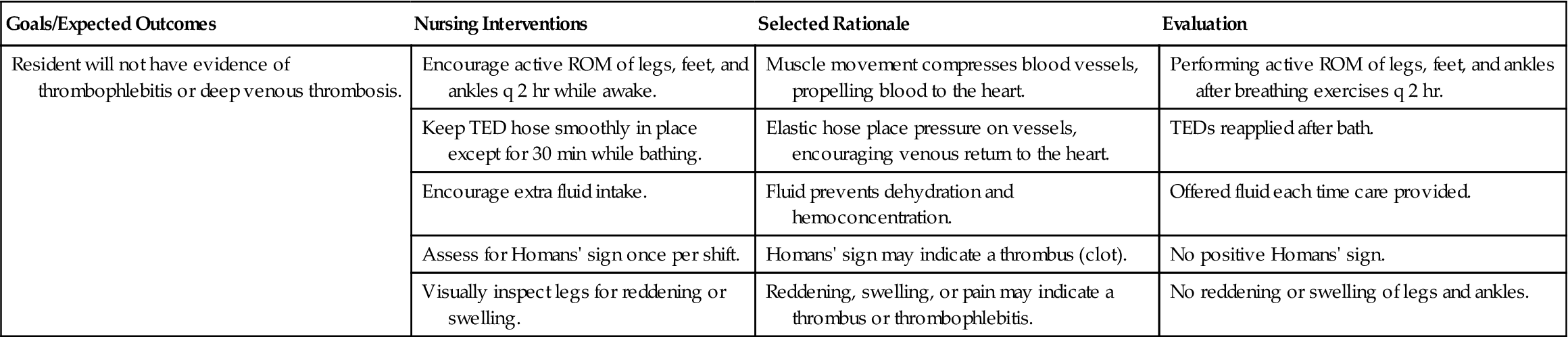
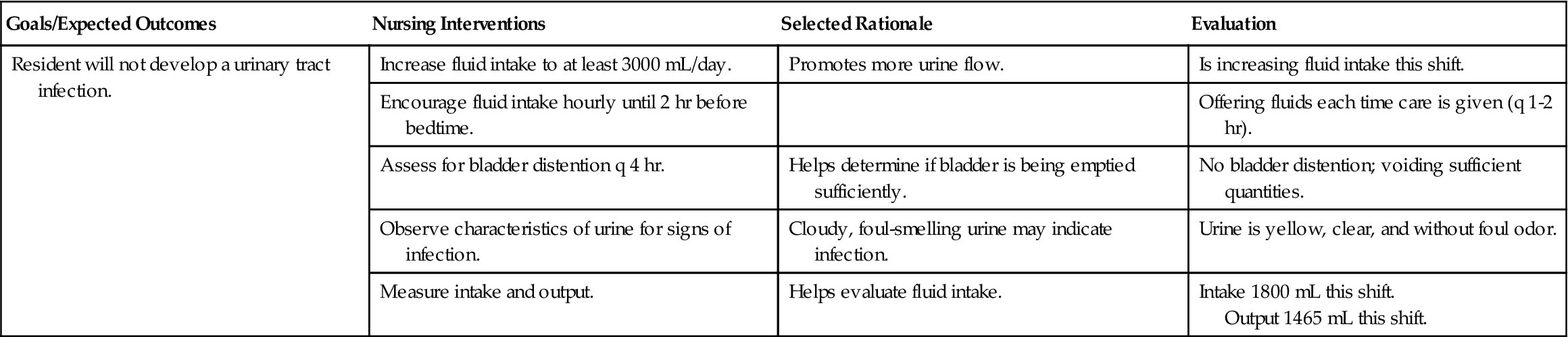
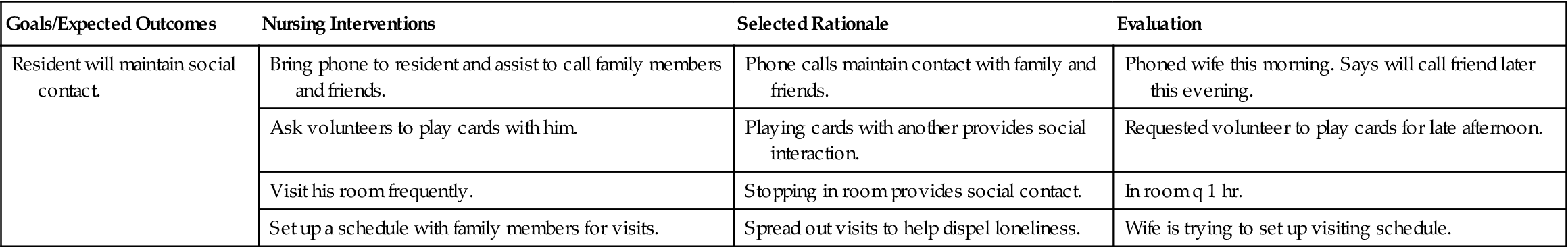
 Nursing Care Plan 9-1
Nursing Care Plan 9-1