Understanding the resident
Objectives
• Define the key terms listed in this chapter.
• Identify the parts that make up the whole person.
• Explain Abraham Maslow’s theory of basic needs.
• Explain how culture and religion influence health and illness.
• Identify the emotional and social effects of illness.
• Describe persons cared for in nursing centers.
• Identify the elements needed for good communication.
• Describe how to use verbal and nonverbal communication.
• Explain the methods and barriers to good communication.
• Explain how to communicate with persons who have behavior problems.
• Explain how to communicate with persons who have disabilities or who are comatose.
• Explain why family and visitors are important to the person.
• Identify the courtesies given to the person, family, and friends.
Key terms
body language Messages sent through facial expressions, gestures, posture, hand and body movements, gait, eye contact, and appearance
comatose Being unable to respond to stimuli
disability Any lost, absent, or impaired physical or mental function
esteem The worth, value, or opinion one has of a person
need Something necessary or desired for maintaining life and mental well-being
nonverbal communication Communication that does not use words
optimal level of function A person’s highest potential for mental and physical performance
paraphrasing Restating the person’s message in your own words
religion Spiritual beliefs, needs, and practices
self-actualization Experiencing one’s potential
self-esteem Thinking well of oneself and seeing oneself as useful and having value
verbal communication Communication that uses written or spoken words
The resident is the most important person in the center. Age, religion, and nationality make each person unique. So do culture, education, occupation, and life-style. Each person is important and special. Each has value. The person is treated as someone who thinks, acts, feels, and makes decisions.
You will care for many residents. Most are old. Each person has fears, needs, and rights. Each has suffered losses—loss of home, family, friends, and body functions. Family and community roles have been lost, too.
Caring for the person
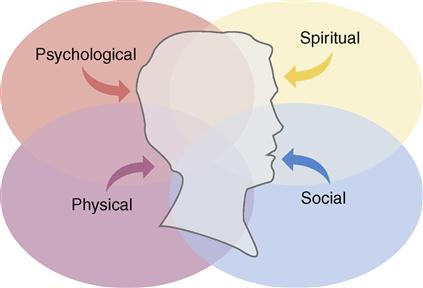
For effective care, you must consider the whole person. Holism means whole. Holism is a concept that considers the whole person. The whole person has physical, social, psychological, and spiritual parts. These parts are woven together and cannot be separated (Fig. 8-1).
Each part relates to and depends on the others. As a social being, a person speaks and communicates with others. Physically, the brain, mouth, tongue, lips, and throat structures must function for speech. Communication is also psychological. It involves thinking and reasoning.
To consider only the physical part is to ignore the person’s ability to think, make decisions, and interact with others. It also ignores the person’s experiences, life-style, culture, religion, joys, sorrows, and needs.
Disability and illness affect the whole person. For example, Mrs. Butler had a stroke. She needs help with her physical needs. She had to leave her home. Relationships with her husband and children are changed. She is angry with God for letting this happen to her. The health team plans care to help her deal with her problems.
Addressing the person
You must know and respect the whole person to provide effective, quality care. Too often a person is referred to as a room number. For example: “12A needs the bedpan,” rather than “Mrs. Brown in 12A needs the bedpan.” This strips the person of his or her identity. It reduces the person to a thing.
Residents are not things. They are not your relatives or children. They are complex, adult human beings. Follow these rules to address them with dignity and respect:
Basic needs
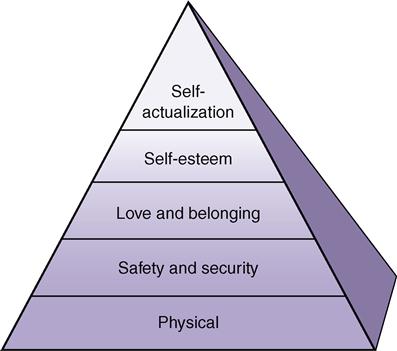
A need is something necessary or desired for maintaining life and mental well-being. According to Abraham Maslow, a famous psychologist, basic needs must be met for a person to survive and function. According to this theory, the needs are arranged in order of importance (Fig. 8-2). Lower-level needs must be met before the higher-level needs. Basic needs, from the lowest level to the highest level, are:
People normally meet their own needs. When they cannot, it is usually because of disease, illness, injury, or advanced age. Those who are ill or injured usually seek health care.
Physical needs
Oxygen, food, water, elimination, rest, and shelter are needed for life. They are needed to survive. A person dies within minutes without oxygen. Without food or water, a person feels weak and ill within a few hours. The kidneys and intestines must function. Otherwise, poisonous wastes build up in the blood. This can cause death. Without enough rest and sleep, a person becomes very tired. Without shelter, the person is exposed to extremes of heat and cold.
You help the person meet physical needs. You need to truly understand their importance. When choking, how do you feel? How do you feel when you are thirsty or hungry? How do you react without enough sleep? What are your fears when you need to use the bathroom right away?
Safety and security needs
Safety and security needs relate to feeling safe from harm, danger, and fear. Many people are afraid of nursing centers. Some care involves strange equipment. Some care causes pain or discomfort. People feel safer and more secure if they know what will happen. For every task, even a simple bath, the person should know:
Many persons do not feel safe and secure when admitted to a nursing center. They are not in their usual, secure home settings. They are in a strange place with strange routines. Strangers care for them. Some become scared and confused.
Be kind and understanding. Show them the new setting. Listen to their concerns. Explain all routines and procedures. You may have to repeat information many times. Sometimes the information may need repeating for many days or weeks until the person feels safe and secure. Be patient.
Love and belonging needs
Love and belonging needs relate to love, closeness, and affection. They also involve meaningful relationships with others. There are many cases in which people became weaker or died because they lacked love and belonging. This is seen in older persons who have out-lived family and friends.
Family, friends, and the health team can meet love and belonging needs. The center is the person’s home. You must help the person feel loved and accepted. Remind the person that you are there to help him or her.
Self-esteem needs
Esteem is the worth, value, or opinion one has of a person. Self-esteem means to think well of oneself and to see oneself as useful and having value. People often lack self-esteem when ill, injured, older, or disabled. For example:
• Cancer treatments caused a woman to lose her hair. She does not feel attractive or whole.
• A person has a slow, crippling disease.
You must treat all persons with respect. Although it takes more time, encourage them to do as much for themselves as possible. This helps increase self-esteem.
The need for self-actualization
Self-actualization means experiencing one’s potential. It involves learning, understanding, and creating to the limit of a person’s capacity. This is the highest need. Rarely, if ever, is it totally met. Most people constantly try to learn and understand more. This need can be postponed, and life will continue.
Culture and religion
Culture is the characteristics of a group of people—language, values, beliefs, habits, likes, dislikes, and customs. They are passed from one generation to the next. The person’s culture influences health beliefs and practices. Culture also affects thinking and behavior during illness and when in a nursing center.
People come from many cultures, races, and nationalities. Their family practices and food choices may differ from yours. So might their hygiene habits and clothing styles. Some speak a foreign language. Some cultures have beliefs about what causes and cures illness. (See Caring About Culture: Health Care Beliefs.) They may perform rituals to rid the body of disease. (See Caring About Culture: Sick Care Practices.) Many have beliefs and rituals about dying and death (Chapter 48). Culture also is a factor in communication.
Religion relates to spiritual beliefs, needs, and practices. A person’s religion influences health and illness practices. Religions may have beliefs and practices about daily living, behaviors, relationships with others, diet, healing, days of worship, birth and birth control, drugs, and death.
Many people find comfort and strength from religion during illness. They may want to pray and observe religious practices. Nursing centers offer religious services. Many have chapels or meditation areas for prayer. Assist residents to attend services as needed (Fig. 8-3). Some leave the center to worship.
A person may want to see a spiritual leader or advisor. Report this to the nurse. Make sure the room is neat and orderly. Have a chair ready for the cleric. Provide privacy during the visit.
The nursing process reflects the person’s culture and religion. The care plan includes the person’s cultural and religious practices.
You must respect and accept the person’s culture and religion. You will meet people from other cultures and religions. Learn about their beliefs and practices. This helps you understand the person and give better care.
A person may not follow all beliefs and practices of his or her culture or religion. Some people do not practice a religion. Each person is unique. Do not judge the person by your standards. And do not force your ideas on the person.
Effects of illness and disability
People do not choose sickness or injury. When they occur, they have physical, psychological, and social effects. Some result in disabilities. A disability is any lost, absent, or impaired physical or mental function. It may be temporary or permanent.
Normal activities—work, driving, fixing meals, yard work, hobbies—may be hard or impossible. Daily activities bring pleasure, worth, and contact with others. People often feel angry, upset, and useless when unable to perform them. These feelings may increase if others must help with routine functions.
Some people feel alone and isolated after out-living family and friends. Those who are disabled or have chronic illnesses may have many fears and concerns about nursing centers. They may feel lonely and abandoned by family and friends. They may fear depending on strangers. Many fear increasing loss of function. Some express their fears. Others do not or cannot.
Anger is a common response to illness and disability. Persons who need nursing center care are often angry. The person may direct anger at you. However, the person is usually angry at the situation. You might have problems dealing with the person’s anger. If so, ask the nurse for help.
You can help the person feel safe, secure, and loved. Take an extra minute to “visit,” to hold a hand, or to give a hug. (Remember to maintain professional boundaries. See Chapter 4.) Show that you are willing to help with personal needs. Respond promptly. Treat each person with respect and dignity.
Optimal level of function
Sometimes the health team cannot prevent increasing loss of function. However, residents are helped to maintain their optimal level of function. This is the person’s highest potential for mental and physical performance. Encourage the person to be as independent as possible. Always focus on the person’s abilities. Do not focus on disabilities.
Hospital patients are often treated as sick, dependent people. Promoting this “sick role” in a nursing center reduces quality of life. The health team focuses on improving the person’s quality of life. You must help each person regain or maintain as much physical and mental function as possible.
Nursing center residents
Most residents are older. Some are alert and oriented. Often they have chronic health problems that prevent them from living alone or with family (Fig. 8-4). Others are very confused and disoriented. They cannot care for themselves. Still others are recovering from fractures, acute illnesses, or surgery. Some residents are terminally ill (dying). They need special care to maintain comfort and make their last days as peaceful as possible.
Alert, oriented residents
Alert and oriented residents know who they are and where they are. They know the year and the time of day. These people need nursing center care because of physical problems. Some are paralyzed from a stroke, injury, or birth defect. Others are disabled from arthritis or multiple sclerosis. Still others have chronic heart, liver, kidney, or respiratory diseases.
The amount of care required depends on the degree of disability. Because these persons are alert and oriented, they may have problems adjusting to a nursing center. The care plan includes measures to help the person accept the nursing center as home.
Confused and disoriented residents
Many persons are mildly to severely confused and disoriented. Some cannot find the dining room. Others do not know the month or year. Others have more severe problems. For example, a man thinks he is waiting for a train. Or an older woman wants to feed her baby. The most severely disoriented persons do not know who they are.
Sometimes confusion and disorientation are temporary. This is especially true for new residents. Some persons have Alzheimer’s disease and other dementias. Confusion and disorientation are permanent and become worse (Chapter 44).
Complete care residents
Some people are very disabled. They also are confused and disoriented. They need total assistance with all activities. They cannot meet any of their own needs. Nor can they say what they need or want. The health team must keep them clean, safe, and comfortable. You must treat them with respect and compassion. Touch, massage, and music may provide comfort and decrease loneliness.
Short-term residents
Some people need nursing center care to recover from fractures, acute illness, or surgery. Often they are younger than most residents. They may need tube feedings, wound care, rehabilitation, or other treatments. Others may need therapy programs: physical, occupational, speech and language, or respiratory. Some need restorative nursing care (Chapter 46). The goal is to help them regain their optimal level of function so they can return home.
Some people are cared for at home. They are admitted to nursing centers for short stays. This is respite care. Respite means rest or relief. The caregiver can take a vacation, tend to business, or simply rest. Respite care may last from a few days to several weeks.
Life-long residents
Birth defects and childhood injuries and diseases can cause disabilities. Intellectual disabilities (mental retardation) and Down syndrome are common causes. A disability occurring before 22 years of age is called a developmental disability (Chapter 45). It may be a physical impairment, intellectual impairment, or both.
The person with a developmental disability has limited function in at least three of these areas:
The person needs life-long assistance, support, and special devices. Some nursing centers admit developmentally disabled children and adults.
Residents with mental health problems
Some people have problems coping or adjusting to stress (Chapter 43). Their behavior and function are affected. In severe cases, self-care and independent living are impaired. Some persons have physical and mental illnesses.
Terminally ill residents
Terminally ill persons are dying. They may have advanced cancer, liver, kidney, respiratory, or other diseases. Some are alert and oriented. Others are comatose. Comatose means being unable to respond to stimuli (p. 94). The person may still feel pain. Often pain is shown by grimacing or groaning.
Some persons have severe pain. They need frequent care to maintain comfort. Promptly report any sign of discomfort to the nurse. Drugs for pain relief are important. So is the care you give. Turning and re-positioning, gentle back rubs, and touch promote comfort and peace. So does holding a hand. Many centers work with hospice programs. The goal is to provide quality care to persons who are dying (Chapters 1 and 48).
Behavior issues
Many people accept illness and disability as part of aging. Others do not adjust well. They have some of the following behaviors. These behaviors are new for some people. For others, they are life-long. They are part of one’s personality.
• Anger. Anger is a common emotion. Causes include fear, pain, and dying and death. Loss of function and loss of control over health and life are causes. Anger is a symptom of some diseases that affect thinking and behavior. Some people are generally angry. Anger is communicated verbally and nonverbally (p. 89). Verbal outbursts, shouting, raised voices, and rapid speech are common. Some people are silent. Others are not cooperative. They may refuse to answer questions. Nonverbal signs include rapid movements, pacing, clenched fists, and a red face. Glaring and getting close to you when speaking are other signs. Violent behaviors can occur.
• Aggressive behavior. The person may swear, bite, hit, pinch, scratch, or kick. Fear, anger, pain, and dementia (Chapter 44) are causes. Protect the person, others, and yourself from harm (Chapter 12).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree