Nursing Care of Women with Complications During Labor and Birth
Objectives
1. Define each key term listed.
2. Discuss each obstetric procedure discussed in this chapter.
3. Illustrate the nurse’s role in each obstetric procedure.
4. Analyze the nurse’s role in a cesarean birth.
5. Describe factors that contribute to an abnormal labor.
6. Explain each intrapartum complication discussed in this chapter.
7. Discuss the nurse’s role in caring for women with each intrapartum complication.
Key Terms
artificial rupture of membranes (AROM) (p. 175)
cephalopelvic disproportion (sĕf-ăh-lō-PĔL-vĭk dĭs-prŏ-PŎR-shŭn, p. 181)
chignon (SHĒN-yŏn, p. 180)
chorioamnionitis (kō-rē-ō-ăm-nē-ō-NĪ-tĭs, p. 192)
dysfunctional labor (p. 183)
dystocia (dĭs-TŌ-sē-ă, p. 183)
fibronectin test (fī-brō-NĔK-tĭn tĕst, p. 193)
hydramnios (hī-DRĂM-nē-ŏs, p. 184)
laminaria (lăm-ĭ-NĂ-rē-ăh, p. 176)
macrosomia (măk-rō-SŌM-ē-ă, p. 186)
oligohydramnios (ŏl-ĭ-gō-hī-DRĂM-nē-ŏs, p. 174)
shoulder dystocia (SHŌL-dŭr dĭs-TŌ-sē-ă, p. 186)
spontaneous rupture of membranes (SROM) (p. 175)
tocolytics (tō-kō-LĬT-ĭks, p. 176)
version (p. 178)
![]() http://evolve.elsevier.com/Leifer
http://evolve.elsevier.com/Leifer
Childbirth is a normal, natural event in the life of most women and their families. When the many factors that affect the birth process function in harmony, complications are unlikely. However, some women experience complications during childbirth that threaten their well-being or that of the infant.
Obstetric Procedures
Nurses assist with several obstetric procedures during birth; they also care for women after the procedures. Some procedures, such as amniotomy or amnioinfusion, are performed to prevent complications during birth. Other procedures are needed when the woman has a complication that necessitates an intervention to promote a positive outcome for the mother and fetus.
Amnioinfusion
An amnioinfusion is the injection of warmed sterile saline or lactated Ringer’s solution into the uterus via an intrauterine pressure catheter during labor after the membranes have ruptured. Indications for this procedure include the following:
• Oligohydramnios (lower-than-normal amount of amniotic fluid)
• Umbilical cord compression resulting from lack of amniotic fluid
• Goal of reducing recurrent variable decelerations in the fetal heart rate
Amnioinfusion replaces the “cushion” for the umbilical cord and relieves the variable decelerations of the fetal heart rate that may occur during contractions when decreased amniotic fluid is present. It can be administered as a one-time bolus for 1 hour or as a continuous infusion. Continuous monitoring of uterine activity and fetal heart rate is essential. The nurse should change the underpads on the bed as needed to maintain patient comfort and should document the color, amount, and any odor of the fluid expelled from the vagina.
Amniotomy
Amniotomy is the artificial rupture of membranes (amniotic sac) (AROM) by using a sterile sharp instrument. It is performed by a physician or nurse-midwife. The nurse assists the health care provider with the procedure and cares for the woman and fetus afterward.
Amniotomy is done to stimulate contractions. It may provide enough stimulation to start labor before it begins naturally, but more often it is done to enhance contractions that have already begun. It may be done to permit internal fetal monitoring (see Chapter 6). The amniotomy stimulates prostaglandin secretion, which stimulates labor, but the loss of amniotic fluid may result in umbilical cord compression.
Technique
To determine if amniotomy is safe and indicated, the health care provider does a vaginal examination to assess the cervical effacement and dilation and the station of the fetus. A disposable plastic hook (Amnihook) is passed through the cervix, and the amniotic sac is snagged to create a hole and release the amniotic fluid.
Complications
Three complications associated with amniotomy may also occur if a woman’s membranes rupture spontaneously (spontaneous rupture of membranes [SROM]). These complications are prolapse of the umbilical cord, infection, and abruptio placentae.
Prolapse of the Umbilical Cord.
Prolapse may occur if the cord slips downward with the gush of amniotic fluid (pp. 194–195).
Infection.
Infection may occur because the membranes no longer block vaginal organisms from entering the uterus. Once performed, an amniotomy commits the woman to delivery within a certain time frame; the physician or nurse-midwife delays amniotomy until he or she is reasonably sure that birth will occur before the risk of infection markedly increases.
Abruptio Placentae.
Abruptio placentae (separation of the placenta before birth) is more likely to occur if the uterus is overdistended with amniotic fluid (hydramnios) when the membranes rupture. The uterus becomes smaller with the discharge of amniotic fluid, but the placenta stays the same size and no longer fits its implantation site (see Chapter 5 for more information about abruptio placentae).
Nursing Care
The nursing care after amniotomy is the same as that after spontaneous membrane rupture: observing for complications and promoting the woman’s comfort.
Observing for Complications.
The fetal heart rate is recorded for at least 1 minute after amniotomy. Rates outside the normal range of 110 to 160 beats/min for a term fetus suggest a prolapsed umbilical cord. A large quantity of fluid increases the risk for prolapsed cord, especially if the fetus is high in the pelvis.
The color, odor, amount, and character of amniotic fluid are recorded. The fluid should be clear, possibly with flecks of vernix (newborn skin coating), and should not have a bad odor. Cloudy, yellow, or malodorous fluid suggests infection. Green fluid means that the fetus passed the first stool (meconium) into the fluid before birth. Meconium-stained amniotic fluid is associated with fetal compromise during labor and infant respiratory distress after birth.
The woman’s temperature is taken every 2 to 4 hours after her membranes rupture according to facility policy. A maternal temperature of 38° C (100.4° F) or higher suggests infection. An increase in the fetal heart rate, especially if above 160 beats/min, may precede the woman’s temperature increase.
Promoting Comfort.
When amniotomy is anticipated, several disposable underpads are placed under the woman’s hips to absorb the fluid that continues to leak from the woman’s vagina during labor. Disposable underpads are changed often enough to keep her reasonably dry and to reduce the moist, warm environment that favors the growth of microorganisms.
Induction or Augmentation of Labor
Induction is the intentional initiation of labor before it begins naturally. Augmentation is the stimulation of contractions after they have begun naturally.
Labor involves the complex interaction between fetus and mother. Before labor is induced, it is important that fetal maturity be confirmed by ultrasound or amniotic fluid analysis (lecithin/sphingomyelin [L/S] ratio) (see Chapter 5), and the status of the cervix is determined. The Bishop score is used to assess the status of the cervix in determining its response to induction (Table 8-1). A score of 6 or more indicates a favorable prognosis for induction. Continuous uterine activity and fetal heart rate monitoring during labor induction is essential.
Table 8-1
| SCORE | 0 | 1 | 2 | 3 |
| Dilation of cervix (cm) | 0 | 1-2 | 3-4 | 5-6 |
| Consistency of cervix | Firm | Medium | Soft | — |
| Length of cervical canal (cm) | >2 | 1-2 | 0.5-1 | <0.5 |
| Cervical effacement (%) | 0-30 | 40-50 | 60-70 | 80 |
| Position of cervix | Posterior | Midline | Anterior | — |
| Station of presenting part related to ischial spines | −3 | −2 | −1 | +1, +2 |
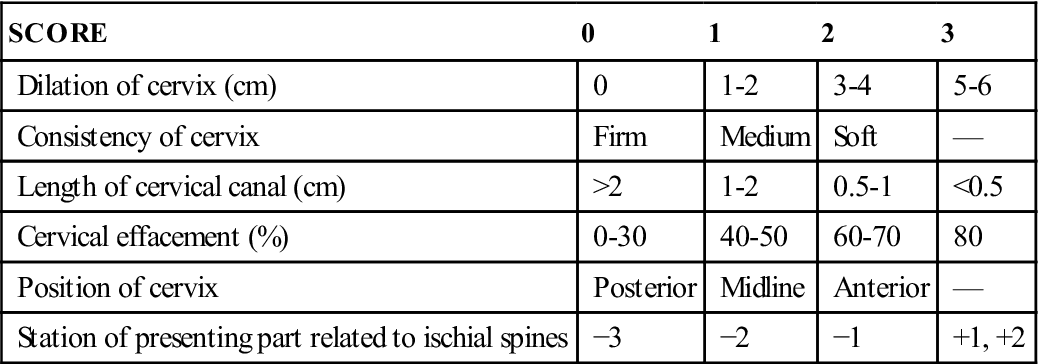
A high score is predictive of a successful labor induction because the cervix has ripened, or softened, in preparation for labor. The American College of Obstetricians and Gynecologists (ACOG) recommends a score of 6 or above before induction of labor. Modified from Stables, D., & Rankin, J. (2005). Physiology in childbearing: With anatomy and related biosciences (2nd ed.). Edinburgh: Elsevier; Gabbe, S., Niebyl, J., Simpson, J., et al (Eds.), (2009). Obstetrics: Normal and problem pregnancies (5th ed.). New York: Churchill-Livingstone.
Indications
Labor is induced if continuing the pregnancy is hazardous for the woman or the fetus. The following are some of the indications for labor induction:
• Gestational hypertension (see Chapter 5)
• Ruptured membranes without spontaneous onset of labor
• Fetal problems, such as slowed growth, prolonged pregnancy, or incompatibility between fetal and maternal blood types (see Chapter 5)
Convenience for the health care provider or the family is not an indication for inducing labor. However, the woman who has a history of rapid labors and lives a long distance from the birth facility may have her labor induced because she has a higher risk of giving birth en route if she awaits spontaneous labor.
Contraindications
Labor is not induced in the following conditions:
• Placenta previa (see Chapter 5)
• Umbilical cord prolapse (see pp. 194–195)
• High station of the fetus, which suggests a preterm fetus or a small maternal pelvis
• Active herpes infection in the birth canal, which the infant can acquire during birth
• Abnormal size or structure of the mother’s pelvis
• Previous classic (vertical) cesarean incision (see Figure 8-4, p. 182)
The physician may attempt to induce labor in a preterm pregnancy if continuing the pregnancy is more harmful to the woman or the fetus than the hazards of prematurity would be to the infant.
Technique
Amniotomy may be the only method used to initiate labor, but it is more likely to be used in combination with oxytocin (Pitocin) administration to stimulate contractions. Induction and augmentation of labor may rely on both pharmacological and nonpharmacological methods.
Pharmacological Methods to Stimulate Contractions
Cervical Ripening.
Induction of labor is easier if the woman’s cervix is soft, partially effaced, and beginning to dilate. These prelabor cervical changes occur naturally in most women. Methods to hasten the changes, or “ripen” the cervix, ease labor induction because oxytocic drugs have no effect on the cervix.
Prostaglandin in the form of a gel or commercially prepared vaginal insert softens the cervix when applied before labor induction. The procedure should be explained to the woman and her family. A fetal heart rate baseline is recorded. An intravenous (IV) line with saline or heparin sodium (Hep-Lock) may be placed in case uterine hyperstimulation occurs and IV tocolytics (drugs that reduce uterine contractions) are needed. After insertion of the prostaglandin gel, the woman remains on bed rest for 1 to 2 hours and is monitored for uterine contractions. Vital signs and fetal heart rate are also recorded. Oxytocin induction can be started when the insert is removed—usually after 6 to 12 hours. Signs of uterine hyperstimulation include uterine contractions that last longer than 90 seconds and/or more than five contractions in 10 minutes.
The vaginal insert can be removed by pulling on the netted string that protrudes from the vaginal orifice. The contractions and fetal heart rate are monitored, and oxytocin may be started as needed. Some women who receive cervical ripening products begin labor without additional oxytocin stimulation. Misoprostol (Cytotec) is frequently used during labor.
An alternative to prostaglandin for cervical ripening is insertion of one or more laminaria into the cervix (Hacker et al., 2009). A laminaria is a narrow cone of a substance that absorbs water and is known as an “osmotic dilator.” The laminaria swells inside the cervix, thus beginning cervical dilation. Oxytocin induction follows, usually on the next day.
Oxytocin Administration.
Initiation or stimulation of contractions with oxytocin (Pitocin) is the most common method of labor induction and augmentation. Oxytocin is administered by registered nurses with additional training in the induction of labor and electronic fetal monitoring. Augmentation of labor with oxytocin follows a similar procedure.
Oxytocin for induction or augmentation of labor is diluted in an IV solution. The oxytocin solution is a secondary (piggyback) infusion that is inserted into the primary (nonmedicated) IV solution line so it can be stopped quickly while an open IV line is maintained. The infusion of oxytocin solution is regulated with an infusion pump. Administration begins at a very low rate and is adjusted upward or downward according to how the fetus responds to labor and to the woman’s contractions. The dose is individualized for every woman. When contractions are well-established, it is often possible to reduce the rate of oxytocin. Augmentation of labor usually requires less total oxytocin than induction of labor because the uterus is more sensitive to the drug when labor has already begun.
Continuous electronic monitoring is the usual method to assess and record fetal and maternal responses to oxytocin. Many health care providers prefer internal methods of monitoring when oxytocin is used because these techniques are more accurate, especially for contraction intensity.
Nonpharmacological Methods to Stimulate Contractions
Walking.
Many women benefit from a change in activity if their labor slows. Walking stimulates contractions, eases the pressure of the fetus on the mother’s back, and adds gravity to the downward force of contractions. If she does not feel like walking, other upright positions often improve the effectiveness of each contraction. She can sit (in a chair, on the side of the bed, or in the bed), squat, kneel while facing the raised head of the bed for support, or maintain other upright positions.
Nipple Stimulation of Labor.
Stimulating the nipples causes the woman’s posterior pituitary gland to naturally secrete oxytocin. This improves the quality of contractions that have slowed or weakened, just as IV administration of synthetic oxytocin does. The woman can stimulate her nipples by doing the following:
• Pulling or rolling them, one at a time
• Gently brushing them with a dry washcloth
• Using water in a whirlpool tub or a shower
If contractions become too strong with these techniques, the woman simply stops stimulation.
Complications of Augmentation of Labor
The most common complications related to overstimulation of contractions are fetal compromise and uterine rupture (see pp. 195–196). Fetal compromise can occur because blood flow to the placenta is reduced if contractions are excessive. Most placental exchange of oxygen, nutrients, and waste products occurs between contractions. This exchange is likely to be impaired if the contractions are too long, too frequent, or too intense.
Water intoxication sometimes occurs because oxytocin inhibits the excretion of urine and promotes fluid retention. Water intoxication is not likely with the small amounts of oxytocin and fluids given intravenously during labor, but it is more likely to occur if large doses of oxytocin and fluids are given intravenously after birth.
Oxytocin is discontinued, or its rate reduced, if signs of fetal compromise or excessive uterine contractions occur. Fetal heart rates outside the normal range of 110 to 160 beats/min, late decelerations, and loss of variability (see Chapter 6) are the most common signs of fetal compromise. Excessive uterine contractions are most often evidenced by contraction frequency greater than every 2 minutes, durations longer than 90 seconds, or resting intervals shorter than 60 seconds. The resting tone of the uterus (muscle tension when it is not contracting) is often higher than normal. Internal uterine activity monitoring allows determination of peak uterine pressures and uterine resting tone.
In addition to stopping the oxytocin infusion, the registered nurse chooses one or more of the following measures to correct adverse maternal or fetal reactions:
• Increasing the nonmedicated intravenous solution
• Changing the woman’s position, avoiding the supine position
The health care provider is notified after corrective measures are taken. A tocolytic (drug that reduces uterine contractions) may be ordered if contractions do not quickly decrease after oxytocin is stopped.
Nursing Care
In 2007, the American Academy of Pediatrics (AAP) and the College of Obstetricians and Gynecologists (ACOG) recommended all patients undergoing oxytocin-induced labor be cared for by an RN with 1 : 1 or 1 : 2 ratio. Fetal heart rate must be assessed and recorded every 15 minutes during active labor and every 5 minutes during transition. Baseline maternal vital signs are assessed, and a fetal monitor tracing is performed to identify contraindications to induction or augmentation before the procedure begins.
If abnormalities are noted in either, the nurse stops the oxytocin and begins measures to reduce contractions and increase placental blood flow. The woman’s blood pressure, pulse rate, and respirations are measured every 30 to 60 minutes. Her temperature is taken every 2 to 4 hours. Recording her intake and output helps identify potential water intoxication.
Version
Version is a method of changing the fetal presentation, usually from breech to cephalic. There are two methods: external and internal. External version is the more common one. A successful version reduces the likelihood that the woman will need cesarean delivery.
Risks and Contraindications
Few maternal and fetal risks are associated with version, especially external version. Version is not indicated if there is any maternal or fetal reason why vaginal birth should not occur, because that is its goal. The following are examples of maternal or fetal conditions that are contraindications for version:
• Disproportion between the mother’s pelvis and fetal size
• Abnormal uterine or pelvic size or shape
• Abnormal placental placement
• Previous cesarean birth with a vertical uterine incision
• Active herpes virus infection
Version may not be attempted in a woman who has a higher risk for uterine rupture, such as several prior cesarean births or high parity. It is not usually attempted if the fetal presenting part is engaged in the pelvis. The main risk to the fetus is that it will become entangled in the umbilical cord, thus compressing the cord. This is more likely to happen if there is not adequate room to turn the fetus, such as in multifetal gestation (e.g., twins) or when the amount of amniotic fluid is minimal.
Technique
External version is done after 37 weeks of gestation but before the onset of labor. The procedure begins with a non–stress test (NST) or biophysical profile (BPP, see Table 5-1) to determine if the fetus is in good condition and if there is adequate amniotic fluid to perform the version. The woman receives a tocolytic drug to relax her uterus during the version.
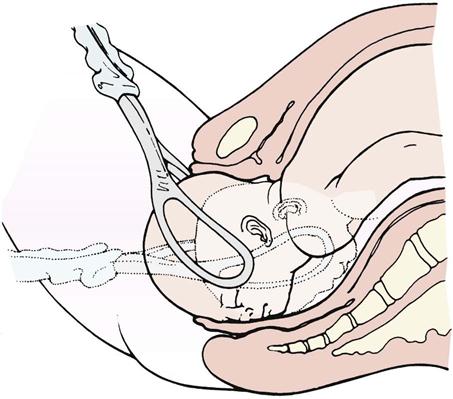
Using ultrasound to guide the procedure, the physician pushes the fetal buttocks upward out of the pelvis while pushing the fetal head downward toward the pelvis in either a clockwise or a counterclockwise turn. The fetus is monitored frequently during the procedure. The tocolytic drug is discontinued after the external version is completed (or the effort abandoned). Rh-negative women receive a dose of Rh0(D) immune globulin (RhoGAM).
Internal version is an emergency procedure. The physician usually performs internal version during a vaginal birth of twins to change the fetal presentation of the second twin.
Nursing Care
Nursing care of the woman having external version includes assisting with the procedure and observing the mother and fetus afterward for 1 to 2 hours. Baseline maternal vital signs and a fetal monitor strip (part of the NST or BPP) are taken before the version. The mother’s vital signs and the fetal heart rate are observed to ensure return to normal levels after the version is complete.
Vaginal leaking of amniotic fluid suggests that manipulating the fetus caused a tear in the membranes, and this is reported. Uterine contractions usually decrease or stop shortly after the version. The physician is notified if they do not. The nurse reviews signs of labor with the woman because version is performed near term, when spontaneous labor is expected.
Episiotomy and Lacerations
Episiotomy is the surgical enlargement of the vagina during birth. Either the physician or a nurse-midwife performs and repairs an episiotomy. A laceration is an uncontrolled tear of the tissues that results in a jagged wound. Lacerations of the perineum and episiotomy incisions are treated similarly.
Perineal lacerations and often episiotomies are described by the amount of tissue involved:
• First degree: Involves the superficial vaginal mucosa or perineal skin
• Second degree: Involves the vaginal mucosa, perineal skin, and deeper tissues of the perineum
• Third degree: Same as second degree, plus involves the anal sphincter
• Fourth degree: Extends through the anal sphincter into the rectal mucosa
Women with third- and fourth-degree lacerations may have more discomfort postpartum if they are constipated after birth.
Indications
Fetal indications for an episiotomy are similar to those for forceps or vacuum extraction (see p. 180). Additional maternal indications include the following:
• Better control over where and how much the vaginal opening is enlarged
• An opening with a clean edge rather than the ragged opening of a tear
Routine episiotomy has been challenged by several recent studies that do not support many of its supposed benefits. Nevertheless, it is so common that the nurse can expect to give postpartum care to many women with episiotomies. Perineal massage and stretching exercises before labor are becoming popular techniques to decrease the need for episiotomy during birth.
Risks
As in other incisions, infection is the primary risk in an episiotomy or laceration. An additional risk is extension of the episiotomy with a laceration into or through the rectal sphincter (third or fourth degree), which can cause prolonged perineal discomfort and stress incontinence.
Technique
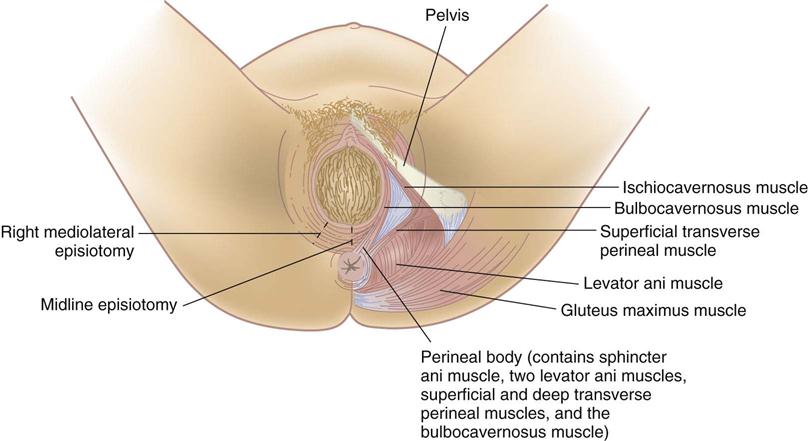
The episiotomy is performed with blunt-tipped scissors just before birth. One of the following two directions is chosen (Figure 8-1):
• Midline (median), extending directly from the lower vaginal border toward the anus
• Mediolateral, extending from the lower vaginal border toward the mother’s right or left
A median episiotomy is easier to repair and heals neatly. The mediolateral incision provides more room, but greater scarring during healing may cause painful sexual intercourse. A laceration that extends a median episiotomy is more likely to involve the rectal sphincter than one that extends the mediolateral episiotomy.
Nursing Care
Nursing care for an episiotomy or laceration begins during the fourth stage of labor. Cold packs should be applied to the perineum for at least the first 12 hours to reduce pain, bruising, and edema. After 12 to 24 hours of cold applications, warmth in the form of heat packs or sitz baths increases blood circulation, enhancing comfort and healing. Mild oral analgesics are usually sufficient for pain management. See Chapter 9 for postpartum nursing care of the woman with an episiotomy or laceration.
Forceps and Vacuum Extraction Births
Obstetric forceps and vacuum extractors are used by an obstetrician to provide traction and rotation to the fetal head when the mother’s pushing efforts are insufficient to accomplish a safe delivery. Forceps are instruments with curved blades that fit around the fetal head without unduly compressing it (Figure 8-2). Several different styles are available to assist the birth of the fetal head in a cephalic presentation or the after-coming head in a breech delivery. Forceps may also help the physician extract the fetal head through the incision during cesarean birth.
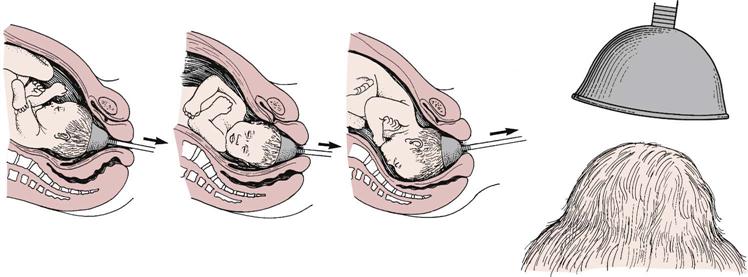
A vacuum extractor uses suction applied to the fetal head so the physician can assist the mother’s expulsive efforts (Figure 8-3). The vacuum extractor is used only with an occiput presentation. One advantage of the vacuum extractor is that it does not take up room in the mother’s pelvis, as forceps do.
Indications
Forceps or vacuum extraction may be used to end the second stage of labor if it is in the best interest of the mother or fetus. The mother may be exhausted, or she may be unable to push effectively. Women with cardiac or pulmonary disorders often have forceps or vacuum extraction births because prolonged pushing can worsen these conditions. Fetal indications include conditions in which there is evidence of an increased risk to the fetus near the end of labor. The cervix must be fully dilated, the membranes ruptured, the bladder empty, and the fetal head engaged and at +2 station for optimal outcome.
Contraindications
Forceps or vacuum extraction cannot substitute for cesarean birth if the maternal or fetal condition requires a quicker delivery. Delivery by these techniques is not done if they would be more traumatic than cesarean birth, such as when the fetus is high in the pelvis or too large for a vaginal delivery.
Risks
Trauma to maternal or fetal tissues is the main risk when forceps or vacuum extraction is used. The mother may have a laceration or hematoma (collection of blood in the tissues) in her vagina. The infant may have bruising, facial or scalp lacerations or abrasions, cephalhematoma (see Chapter 12), or intracranial hemorrhage. The vacuum extractor causes a harmless area of circular edema on the infant’s scalp (chignon) where it was applied.
Technique
The health care provider catheterizes the woman to prevent trauma to her bladder and to make more room in her pelvis. After the forceps are applied, the physician pulls in line with the pelvic curve. An episiotomy is usually done. After the fetal head is brought under the mother’s symphysis, the rest of the birth occurs in the usual way.
Birth assisted with the vacuum extractor follows a similar sequence. The health care provider applies the cup over the posterior fontanelle of the fetal occiput, and suction is created with a machine to hold it there. Traction is applied by pulling on the handle of the extractor cup.
Nursing Care
If the use of forceps or vacuum extraction is anticipated, the nurse places the sterile equipment on the delivery instrument table. After birth, care is similar to that for episiotomy and perineal lacerations. Ice is applied to the perineum to reduce bruising and edema. The physician is notified if the woman has signs of vaginal hematoma, which include severe and poorly relieved pelvic or rectal pain.
The infant’s head is examined for lacerations, abrasions, or bruising. Mild facial reddening and molding (alteration in shape) of the head are common and do not necessitate treatment. Cold treatments are not used on neonates because they would cause hypothermia.
Pressure from forceps may injure the infant’s facial nerve. This is evidenced by facial asymmetry (different appearance of right and left sides), which is most obvious when the infant cries. Facial nerve injury usually resolves without treatment. The scalp chignon from the vacuum extractor does not necessitate intervention and resolves quickly.
Cesarean Birth
Cesarean birth is the surgical delivery of the fetus through incisions in the mother’s abdomen and uterus. Cesarean birth rates in the United States are 27.6% (National Center for Health Statistics [NCHS], 2008), and the goal of Healthy People 2020 (U.S. Department of Health and Human Services, 2010) is to reduce cesarean sections to 15%. This is the basis for some of the changes in the management of the second stage of labor, such as the following:
• Position variation (upright or horizontal)
• Oxytocin (Pitocin) augmentation of labor
• Spontaneous open glottis pushing when fetus is at +1 station
• Use of vacuum-assisted delivery rapidly replacing forceps delivery
• Trial of labor before repeat cesarean (vaginal birth after cesarean [VBAC])
In 1997 the World Health Organization (WHO) recommended minimal intervention with maximum patience, support, and tender loving care (TLC). Although the total percentage of cesarean births has increased from 2002, the rate of VBAC has decreased in the United States (NCHS, 2008).
Indications
Several conditions may necessitate cesarean delivery:
• Inability of the fetus to pass through the mother’s pelvis (cephalopelvic disproportion)
• Maternal conditions such as gestational hypertension or diabetes mellitus
• Active maternal herpes virus, which may cause serious or fatal infant infection
• Previous surgery on the uterus, including the classic type of cesarean incision
• Fetal compromise, including prolapsed umbilical cord and abnormal presentations
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree