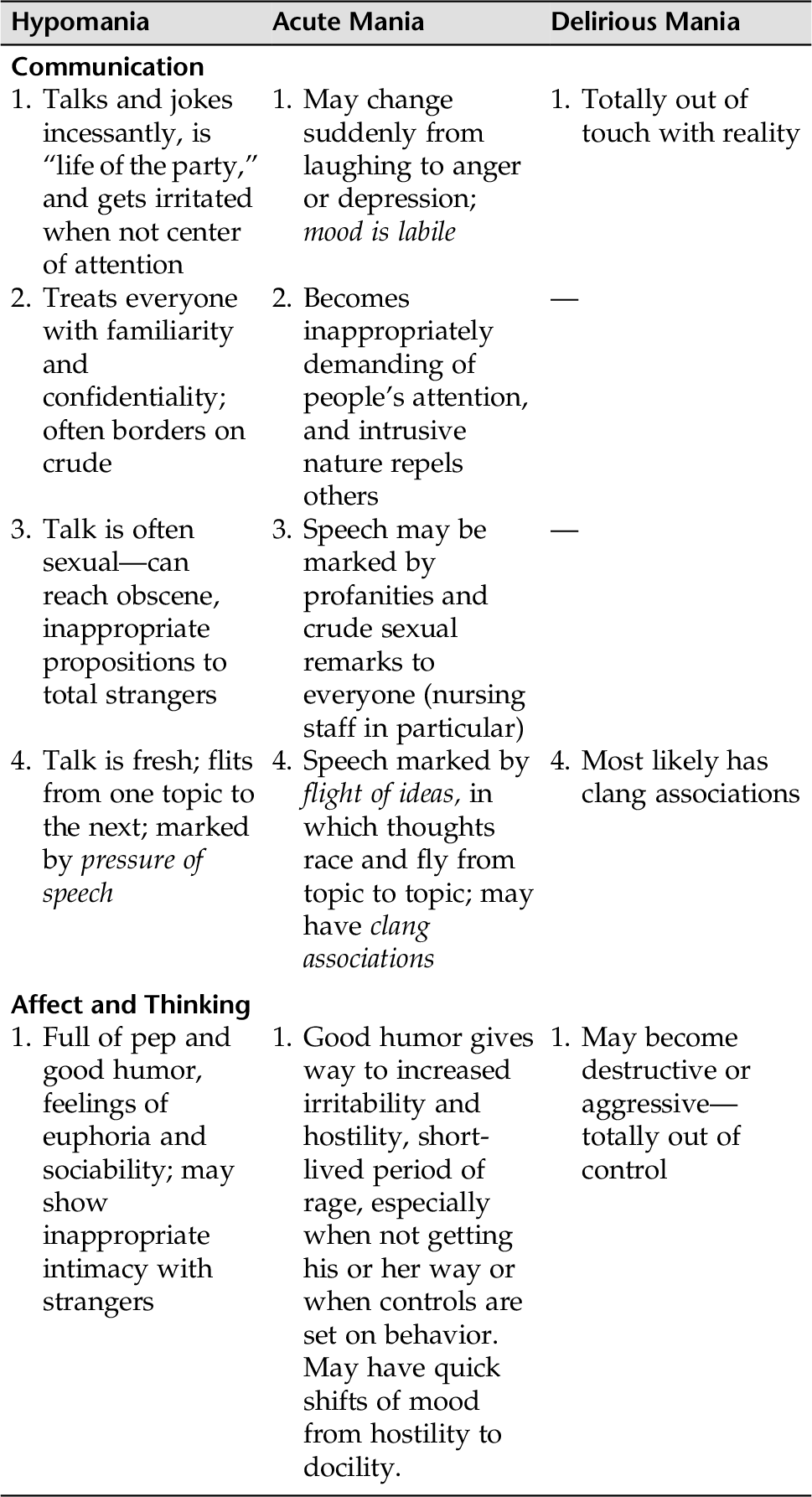
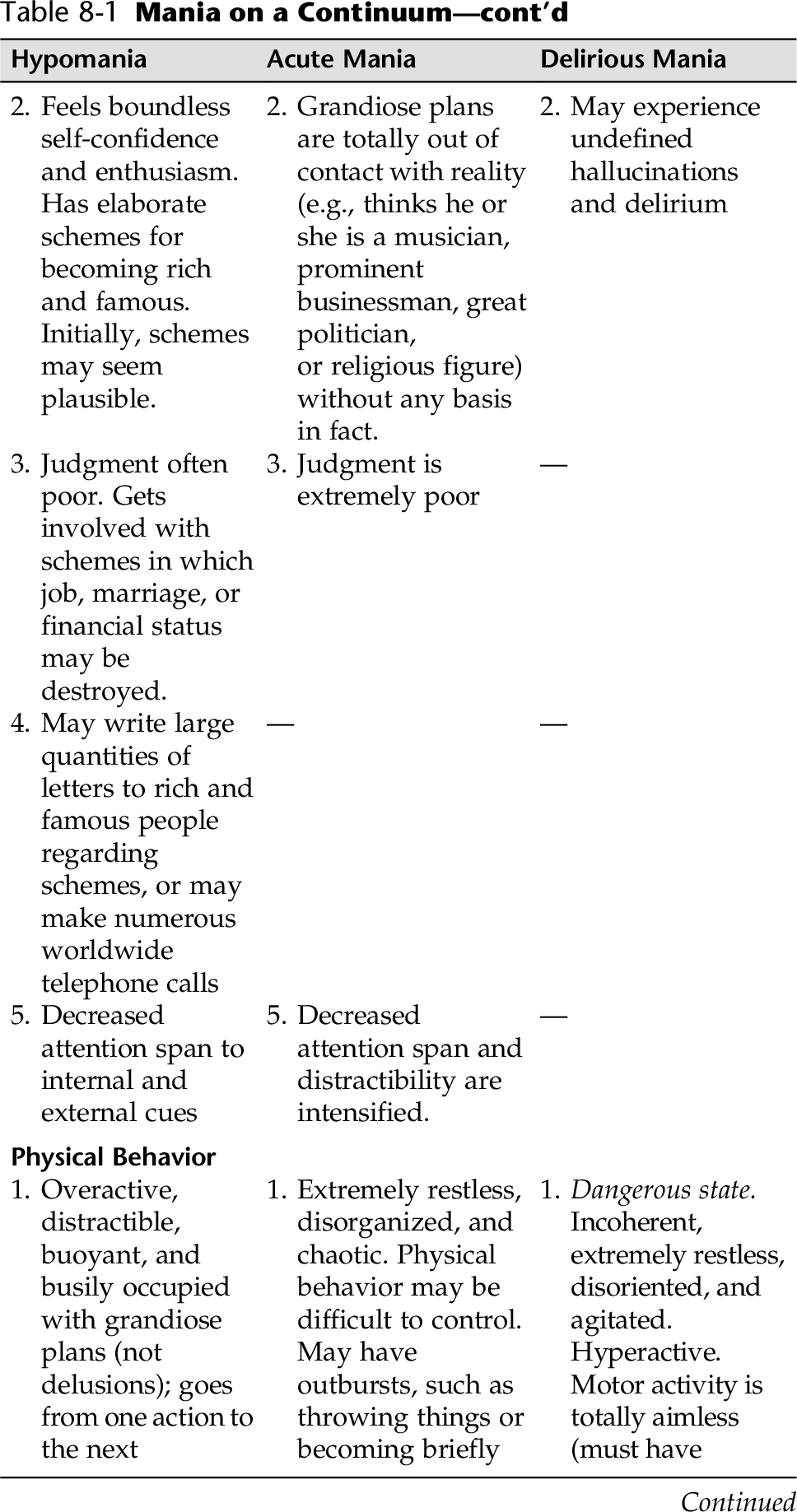
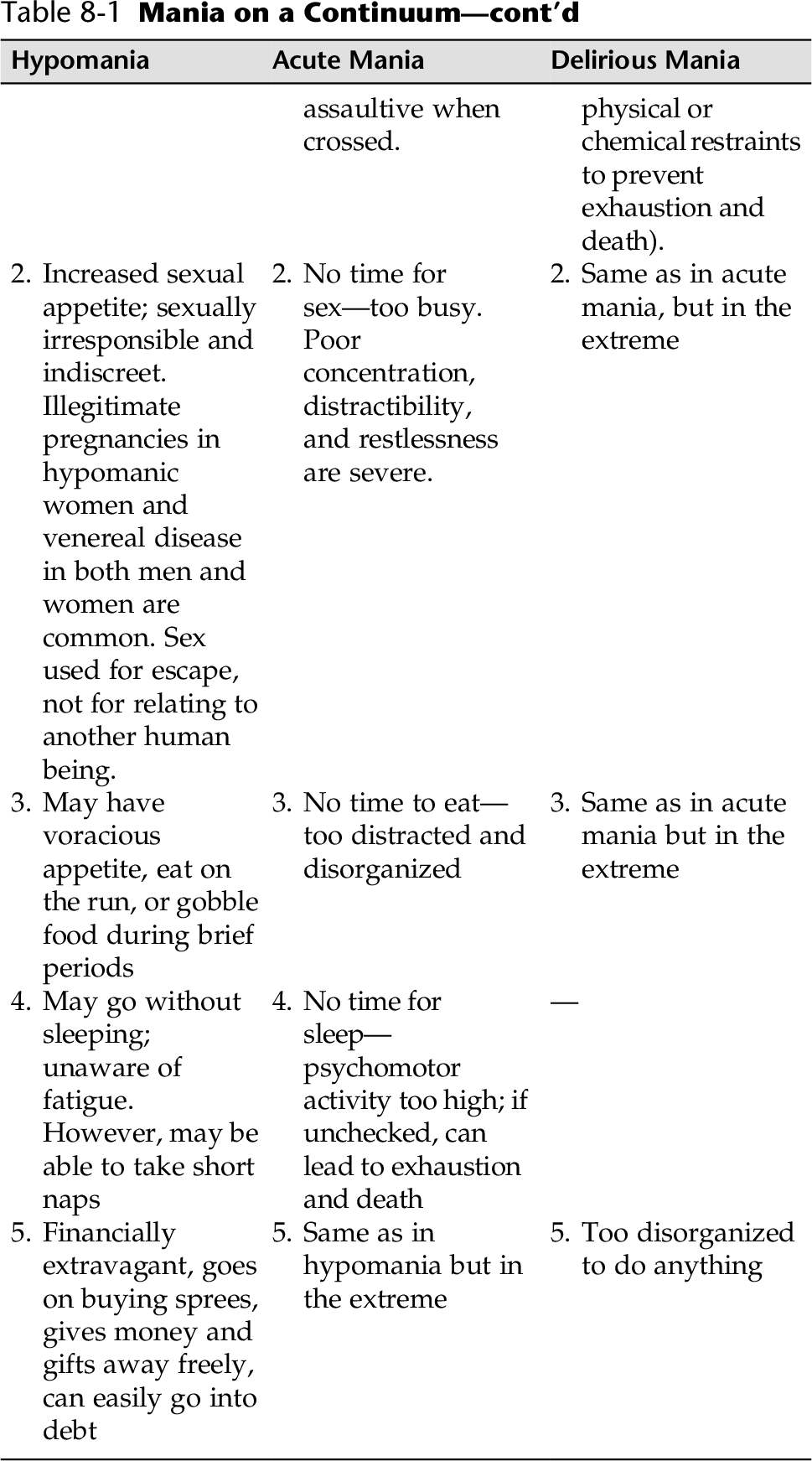
CHAPTER 8 Bipolar spectrum disorders are among the most serious of the neurobiological mental disorders that often leave people destitute; with shattered friendships, families, and partner relationships; and result in jobs lost. Bipolar spectrum disorders are a group of disorders with different courses and treatments. Simplistically stated, bipolar disorders are mood disorders that include one or more episodes of mania or hypomania (elevated, expansive, or irritable mood; increased activity and energy) and usually one or more depressive episodes. These disorders are essentially related to biochemical imbalances in the brain, and the disease is thought to be genetically transferred. Medication adherence is key if nursing and counseling interventions are to be effective. An acute or severe manic phase usually warrants hospitalization. A person experiencing hypomania, however, rarely needs hospitalization unless there is a danger to self or others. Bipolar disorders consist of three different categories of disorders: (1) cyclothymia, (2) bipolar disorder (bipolar I and bipolar II), and (3) bipolar disorder not otherwise specified. The symptoms seen in bipolar disorder I and II are more serious than those seen in cyclothymia. Cyclothymia is a chronic mood disturbance lasting two years or more with the recurrent experience of some of the symptoms of hypomania alternating with a persistent (dysthymic) depression. People with cyclothymia do not have severe impairment in their social or occupational functioning, nor do they experience psychotic symptoms such as delusions. The manic episode in bipolar I might begin suddenly and last a few days to months. There can be impairments in reality testing; when severe, these impairments can take the form of grandiose or persecutory delusions. Considerable impairment in social, occupational, and interpersonal functioning exists. Hospitalization is often required to protect the person from the consequences of poor judgment and hyperactivity. Bipolar disorder is classified as a severe, biologically based mental illness by medical science and diagnostic criteria according to the DSM-5. Bipolar I consists of one or more episodes of major depression plus one or more periods of clear-cut mania. The individual may also experience mixed episodes as well (simultaneous symptoms of mania and depression). Bipolar II consists of one or more periods of major depression plus at least one hypomanic episode. The distinction between hypomania and mania is made clear In Table 8-1. Bipolar disorder can be grouped into three phases: 2. Continuation Phase (continuation of treatment)—Usually lasts for 4 to 9 months, and the goal during this phase is to prevent relapse. 3. Maintenance Treatment Phase—Aimed at preventing the recurrence of an episode of bipolar illness. Many of the interventions in this chapter address the patient in the acute phase, because this phase often requires hospitalization and immediate and complex nursing care. A thorough physical workup will most likely identify medical conditions associated with mania and/or drugs (prescription, over-the-counter, recreational) that can induce mania. • Periods of hyperactivity (pacing, restlessness, accelerated actions) • Overconfident, exaggerated view of own abilities • Decreased need for sleep, no acknowledgment of fatigue • Increased energy • Poor social judgment, engaging in reckless and self-destructive activities (foolish business ventures, sexual indiscretions, buying sprees) • Rapid-fire speech; pressured speech; loud, garrulous, rhyming or punning • Brief attention span, easily distractible, flights of ideas, loosened associations, delusions • Expansive, irritable, or paranoid behaviors • Impatient, uncooperative, abusive, obscene, manipulative See Appendix D-4 for a questionnaire for mania. Patients might want to take this test frequently to monitor symptoms. Assessment will, of course, include identification of manic symptoms (Appendix D-4) and depressive symptoms (Appendix D-3). However, there are very important areas that need to be identified to secure safety, not just for the patient, but perhaps others as well. Important overall assessment guidelines follow. 1. Assess if patient is a danger to self or others: • Manic patients can exhaust themselves to the point of death. • Patient might not eat or sleep for days at a time. • Poor impulse control might result in harm to others or self. • Uncontrolled spending can leave individuals and their families destitute. 2. Patients might give away all of their money or possessions, so might need controls to protect them from bankruptcy. 3. Assess for need for hospitalization to safeguard and stabilize patient. 4. Assess medical status. A thorough medical examination helps determine if mania is primary (a mood disorder—bipolar/cyclothymia) or secondary to another condition. Mania can be: • Secondary to a general medical condition • Substance induced (use or abuse of drug, medication, or toxin exposure) 5. Assess the patient’s and family’s understanding of bipolar disorder, knowledge of medications, support groups, and organizations that provide information on bipolar disorder. During an acutely or extremely manic episode, hospitalization is recommended to prevent physical exhaustion and to initiate and stabilize medication. The primary consideration is the prevention of exhaustion and death from cardiac collapse. Because of the patient’s poor judgment, excessive and constant motor activity, probable dehydration, and difficulty evaluating reality, the patient is at risk for injury (Risk for Injury). Aggression is a common feature in mania. At times, intrusive and taunting behaviors can induce others to strike out against these patients. Conversely, when in a manic state, a patient might evidence inability to control behavior, and destructive, hostile, and aggressive behaviors (range reaction) might occur and pose danger to the well-being of others and/or property (Risk for Violence: Self-Directed or Other-Directed). Grandiosity and poor judgment can result in the patient giving away money and possessions indiscriminately, bankruptcy, and neglect of family. Patients might get involved in making foolish business deals or make impulsive major life changes (e.g., divorce, marriage, or career changes). Getting involved in impossible schemes, shady legal deals, and questionable business ventures can also be part of the picture. Because of the patient’s grandiose thinking and extremely poor judgment, and hyperactivity, Ineffective Impulse Control is usually part of the picture. The behaviors that stem from the patient’s faulty thinking and impulsivity usually result in Ineffective Impulse Control. Patients in the manic phase can be extremely manipulative, fault finding, and adept at exploiting other’s vulnerabilities. They constantly push limits. Often the motivation for this manipulation is an attempt to gain a sense of control, when in fact the person is totally unable to control any aspect of his or her life—thoughts, feelings, and particularly behaviors. Therefore, Defensive Coping might be evidenced by the patient’s manipulative, angry, and hostile verbal behaviors. The families of individuals with bipolar disorder often experience extreme disruptions in their lives and might be in crises when their family member is in acute and severe mania. Infidelity and divorce is common; family savings might be wiped out and debt accumulated; relationships within the family unit might be strained beyond endurance; and friendships can be ruined. Interrupted Family Processes must always be assessed and information and referrals for support provided. The patient in the acute or extreme manic state might have numerous unmet physical needs. The manic patient is too agitated and hyperactive to eat, sleep, or be appropriately groomed or dressed and may be constipated. Therefore, Deficient Fluid Volume, Imbalanced Nutrition, Disturbed Sleep Pattern, Constipation, Dressing/Grooming Self-Care Deficit, and Bathing/Hygiene Self-Care Deficit are all areas that need to be carefully assessed. When the patient is severely manic, the nurse could target interventions for all of the above using Total Self-Care Deficit (eating, sleeping, dressing/grooming, bathing/hygiene, bowel functioning). Table 8-1 provides a list of potential nursing diagnoses. Specific behaviors demonstrated by the manic patient should be addressed separately, as follows in this chapter. Overall guidelines that are effective with bipolar patients during periods of mania include: 1. Use a firm and calm approach. 2. Use short, concise explanations or statements. 3. Remain neutral; avoid power struggles. 4. Provide a consistent and structured environment. 5. Firmly redirect energy into appropriate and constructive channels. 6. Decrease environmental stimuli whenever possible. 7. Provide structured solitary activities; tasks that take minimal concentration are best. Avoid groups and stimulating activities until the patient can tolerate that level of activity. 8. Spend one-on-one time with the patient if he or she is psychotic or anxious. 9. Provide frequent rest periods. 10. Provide high-calorie fluids and finger foods frequently throughout the day. 11. On a daily basis, monitor the patient’s: • Food intake • Elimination (constipation often a problem) 12. Teach patient and family about illness, and be sure patient has written information regarding his or her medications. 13. Ascertain that patient and family have information on supportive services in their community for further information and support. The following sections identify primary nursing diagnoses for use with a manic patient, particularly in the acute and severely manic phases of the illness. Included are specific nursing interventions that are appropriate for meeting outcome criteria for each diagnosis. Cognitive, affective, and psychomotor factors: • Response to medication will have expected therapeutic effects • Maintenance of therapeutic blood levels (0.4 to 1.0 mEq/L, although 0.6- 0.8 mEq are effective for most patients [Lehne, 2013])* • Sustain optimum physical health through medication management and therapeutic regimen Patient will: • Be free from injury within 2 to 3 weeks • Cardiac status stable • Well hydrated • Skin free of abrasions and scrapes • Be free from excessive physical agitation and purposeless motor activity within 2 weeks • Take short voluntary rest periods during the day by (date) • Patient’s cardiac status will remain stable while in the hospital. • While acutely manic, patient will drink 8 ounces of fluid every hour throughout the day. • Patient will spend time with the nurse in a quiet environment three to four times a day between 7 AM and 11 PM with the aid of nursing guidance. • Patient will remain free from falls and abrasions every day while in the hospital. • Patient will be free from dangerous levels of hyperactive motor behavior with the aid of medications and nursing interventions within 24 hours. • Displays nonviolent behaviors toward self and others • Verbalizes control of feelings • Interacts with others appropriately Patient will: • Refrain from verbal threats and loud, profane language toward others by (date) • Seek help when experiencing aggressive impulses by (date) • Demonstrate healthier ways to deal with stress (e.g., walking, sports) Patient will: • Refrain from provoking others to physical harm, with the aid of seclusion or nursing interventions by (date) • Respond to external controls (medications, seclusion, nursing interventions) when potential or actual loss of control occurs by (date)
Bipolar Spectrum Disorders
OVERVIEW
Cyclothymia
Bipolar Disorder (Bipolar I and Bipolar II)
ASSESSMENT
Presenting Signs and Symptoms
Assessment Tools
Assessment Guidelines
Elated-Phase Bipolar
NURSING DIAGNOSES WITH INTERVENTIONS
Discussion of Potential Nursing Diagnoses
Overall Guidelines for Nursing Interventions
Elated-Phase Bipolar
Selected Nursing Diagnoses Nursing Care Plans
Risk Factors (Risk-Related Behaviors)
 Biochemical/neurological dysfunction
Biochemical/neurological dysfunction
 Physical (e.g., broken skin, altered mobility)
Physical (e.g., broken skin, altered mobility)
 Impaired judgment (reality testing, risky behavior)
Impaired judgment (reality testing, risky behavior)
 Excessive and constant motor activity—unable to rest for even short periods
Excessive and constant motor activity—unable to rest for even short periods
 Lack of fluid ingestion/dehydration
Lack of fluid ingestion/dehydration
 Abrasions, bruises, cuts from running/falling into objects
Abrasions, bruises, cuts from running/falling into objects
Outcome Criteria
Long-Term Goals
Short-Term Goals
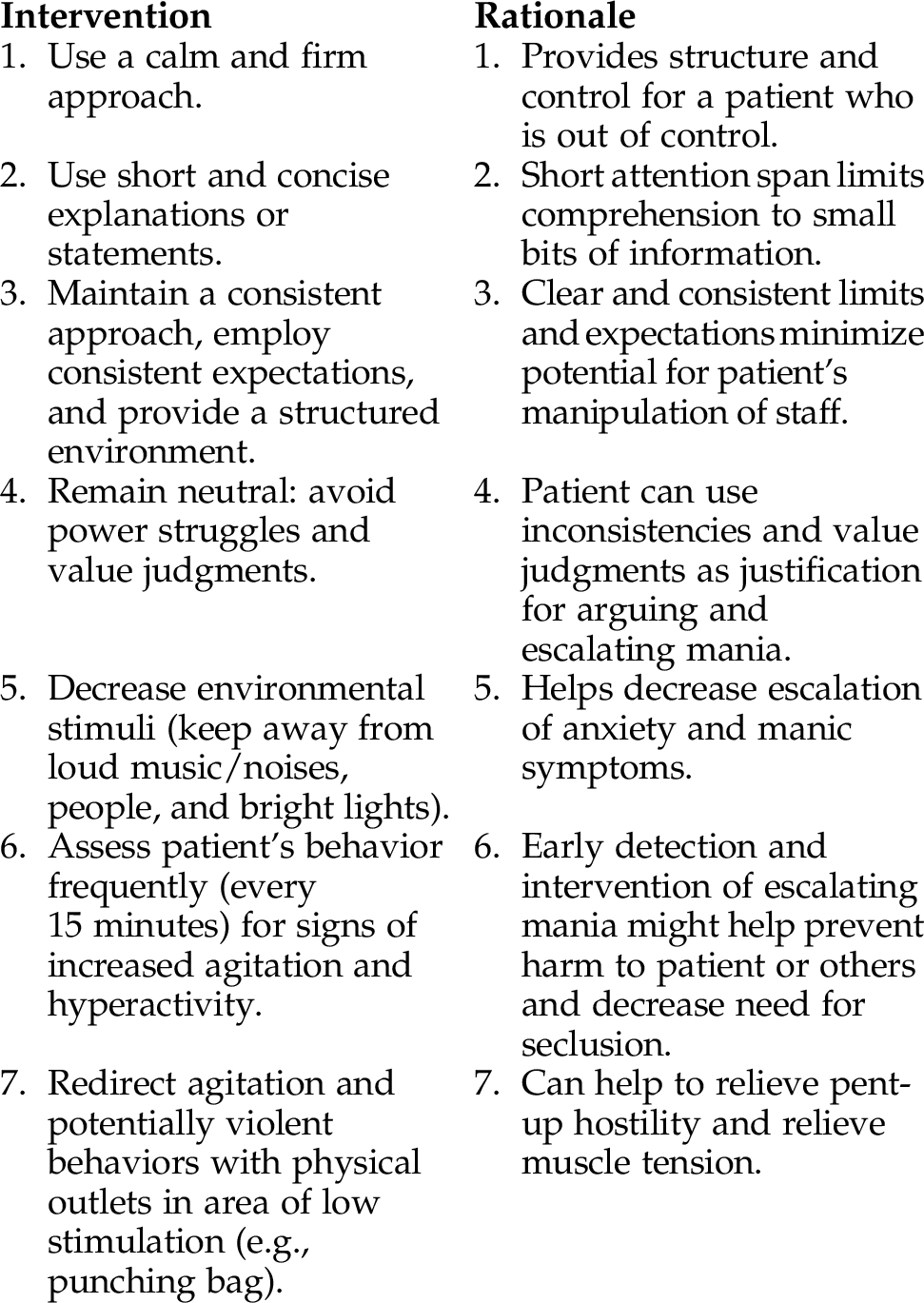
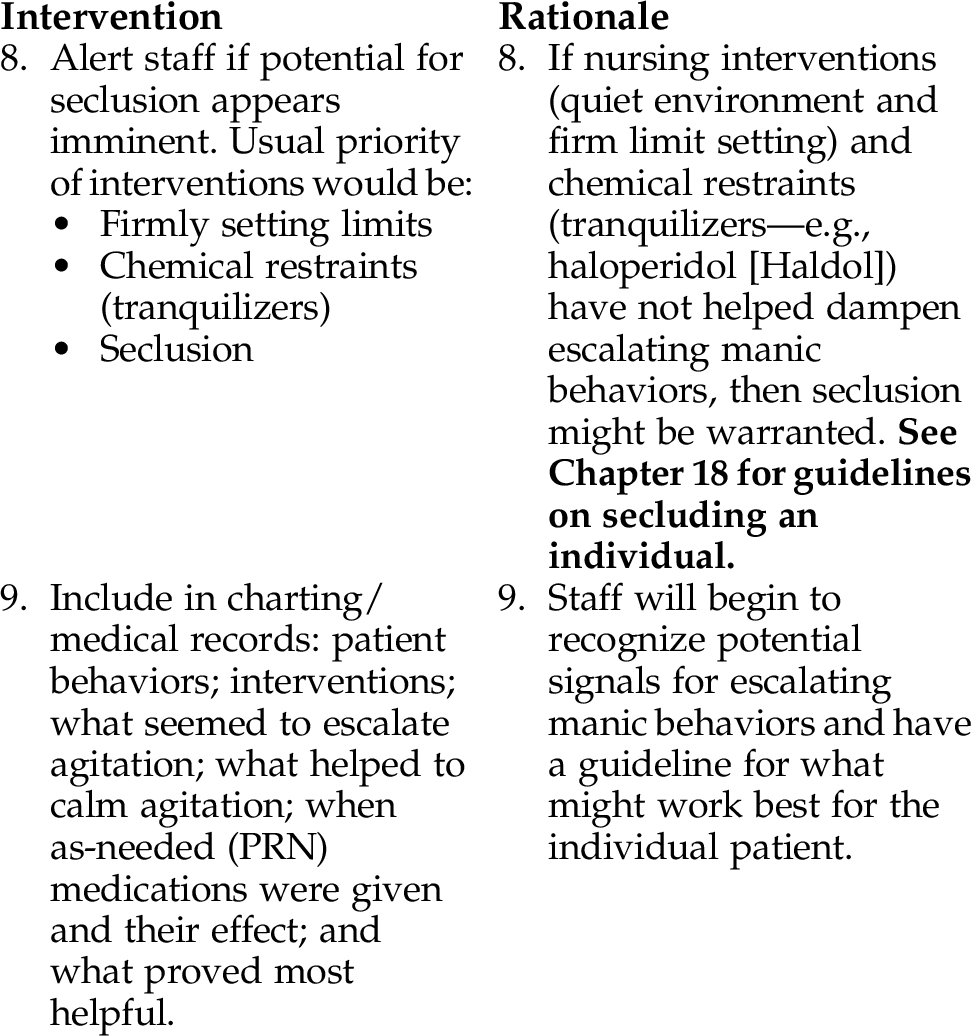
INTERVENTIONS AND RATIONALES
Risk Factors (Related To)
 History of violence toward others
History of violence toward others
 Mental health problems (e.g., bipolar spectrum disorder)
Mental health problems (e.g., bipolar spectrum disorder)
 Biochemical/neurological imbalances
Biochemical/neurological imbalances
Defining Characteristics (As Evidenced By)
 Verbal threats against self (suicidal threats/attempts, hitting or injuring self, banging head against wall)
Verbal threats against self (suicidal threats/attempts, hitting or injuring self, banging head against wall)
 Provocative behaviors (e.g., argumentative)
Provocative behaviors (e.g., argumentative)
 Loud, threatening, profane speech
Loud, threatening, profane speech
 Agitated behaviors (e.g., slamming doors, prowling hallways, increased muscle tension, knocking things over
Agitated behaviors (e.g., slamming doors, prowling hallways, increased muscle tension, knocking things over
Outcome Criteria
Long-Term Goals
Short-Term Goals
INTERVENTIONS AND RATIONALES
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree