CHAPTER 7 Happiness and unhappiness are appropriate responses to life events. When sadness, grief, or elation is extremely intense and the mood unduly prolonged, a mood disorder may be the cause. It’s important to understand that individuals who are going through depression are often in substantial pain, experiencing severe suffering, and have intolerable sadness. Depressive symptoms often coexist in people with alcohol or substance use problems. Depressive symptoms are common in people who have other psychiatric disorders (e.g., anxiety disorders, eating disorders, borderline personality disorders, schizophrenia). Depression is highly comorbid in individuals who have been physically or mentally abused (posttrauma behaviors). Depression might also be a critical symptom of another medical disorder or condition such as hepatitis, mononucleosis, multiple sclerosis, dementia, cancer, diabetes, and chronic pain. Depression is often directly related to the intake of many commonly prescribed medications such as antihypertensive medications, steroids, hormones, digitalis, and stimulants. Therefore, mood disorders are common and can be caused by a medical condition, psychoactive drugs, medications, and a host of psychiatric conditions. However, interventions for depression can be helpful, regardless of the etiology. Risk for Suicide is an essential component of a thorough assessment, regardless of the cause of depression. Refer to Chapter 17 for more on the diagnoses and interventions specific for suicide. The two DSM-5 depressive disorders discussed here are Major Depressive Disorder (MDD) and Persistent Depressive Disorder (dysthymia). In MDD, a severely depressed mood, usually recurrent, causes clinically significant distress or impairment in social, occupational, or other important areas of the person’s life. The depressed mood can be distinguished from the person’s usual functioning and might occur suddenly or gradually. Major depression is basically a depression that is thought to involve changes in receptor neurotransmitter relationships in the limbic system, prefrontal cortex, hippocampus, and amygdala. The primary neurotransmitters involved with depression are serotonin and norepinephrine, although dopamine is also related to depression. Genetic factors and biochemical and brain scans also reveal anomalies in some individuals suffering from depression. People with major depression may have other problems, such as: • Psychotic features—delusions or hallucinations • Seasonal affective disorder (SAD)—most prominent during certain seasons (e.g., winter or summer); SAD is more prevalent in climates with longer periods of darkness in a 24-hour cycle • Catatonic features—for example, peculiarities of voluntary movement, motor immobility, purposeless motor activity, echolalia, or echopraxia • Melancholic features—severe symptoms, loss of feelings of pleasure, worse in morning, early morning awakening, significant weight loss, excessive feelings of guilt • Postpartum onset—within 4 weeks of delivery Persistent depressive disorder (dysthymia) is characterized by less severe, usually chronic depressive symptoms that have been present for a longer period of time (e.g., 2 years or longer). The symptoms of persistent depressive disorder are very similar to those of major depression, which makes an accurate diagnosis difficult. Although the symptoms and functional impairment are not as severe with persistent depressive disorder (dysthymia) as they are in MDD, symptoms can cause significant distress or impairment in major areas of the person’s life. Individuals with dysthymia are usually able to function at work and in social situations, but not often at optimal levels. There are no psychotic symptoms in people with a persistent depressive disorder. • Mood of sadness, despair, emptiness • Diminished interest in or pleasure in almost all activities (anhedonia) • Vegetative Signs: Alterations in eating, sleeping, activity level (fatigue), and libido • Feelings of worthlessness or guilt • Difficulty with concentration, memory, and making decisions • Recurrent thoughts of death and/or self-harm • Apathy, low motivation, and social withdrawal • Irritability • Excessive emotional sensitivity • May complain of pain, such as backache or headache, that does not seem to have a physical cause Many useful assessment tools are available to evaluate for depression. Appendix D-3, Hamilton Rating Scale for Depression (HRSD), is a good example. • The patient has taken drugs or alcohol • Medical conditions are present 2. Always evaluate the patient’s risk for harm to self or others. Overt hostility is highly correlated with suicide. Depression can drastically affect many areas of a person’s life. Risk for Self-Directed Violence is the first priority for assessment and intervention. Risk for Suicide is a concern for patients who have a variety of psychiatric disorders (schizophrenia, bipolar disorder, substance abuse, borderline personality disorder), as well as medical disorders and syndromes. Refer to Chapter 17 for information on suicide. Depression often affects the person’s cognitive ability. Poor concentration, lack of judgment, and difficulties with memory can all affect a person’s ability to cope with his or her confused thoughts and profound feelings of despair. Therefore Ineffective Coping is almost always in evidence. Feelings of self-worth plummet (Chronic Low Self-Esteem), and ability to gain strength from usual religious activities dwindles (Spiritual Distress). Feelings of hopelessness are common. Most noticeably, the ability to interact and gain solace from others is markedly reduced (Impaired Social Interaction). The vegetative signs of depression can lead to physical complications such as lack of sleep (Disturbed Sleep Pattern), change in eating patterns (Imbalanced Nutrition), and change in elimination (most often Constipation, although diarrhea can also occur in agitated individuals). Therefore, Self-Care Deficit is often an obvious occurrence. Table 7-1 identifies some potential nursing diagnoses for depressive disorders. Table 7-1 Potential Nursing Diagnoses for Depressive Disorders The section that identifies specific nursing diagnoses, goals, and interventions is useful when working with depressed patients and targeting discrete problems. However, the following overall guidelines are important throughout the nurse’s work with depressed patients. 2. Note that the instillation of hope is a key tool for recovery. 3. Enhance the patient’s sense of self by highlighting past accomplishments and strengths. 4. Whether in the hospital or in the community: • Assess patient’s needs for self-care, and offer support when appropriate. • Monitor and intervene to help patient maintain adequate nutrition, hydration, and elimination. • Monitor and intervene to help provide adequate balance of rest, sleep, and activity. • Monitor and record increases/decreases in symptoms and which nursing interventions are effective. • Involve the patient’s support system, and find supports for patient and family members in the community that are appropriate to their needs. 5. The dysfunctional attitude or learned helplessness and hopelessness seen with depressed individuals can be alleviated through cognitive therapy or other psychotherapeutic interventions. 6. Continuously assess for the possibility of suicidal thoughts and ideation throughout the patient’s course of recovery. (Refer to Chapter 17 for information on suicide.) 7. Primary depression is a medical disease. People respond well to psychopharmacology and electroconvulsive therapy (ECT). Be sure patients and those closely involved with them understand the nature of the disease and have written information about the specific medications the patient is taking. Psychoeducation and a support system are essential. 8. Assess the family’s and significant other’s needs for teaching, counseling, self-help groups, and knowledge of community resources. The following section offers key nursing diagnoses, goals, and nursing interventions that can help nurses and other clinicians when planning care for a depressed individual/patient. • Behavioral manifestations of depression are absent • Satisfaction with social circumstances and achievement of life goals • Seeks help when experiencing self-destructive/other-destructive impulses • Positive changes in quality of life (e.g., ability to work, intimate relationships, social relationships, and enjoyment of life have improved significantly). Patient will: • Demonstrate alternative ways of dealing with negative feelings and emotional stress by (date) • Identify supports and support groups with whom he or she is in contact within 1 month • State that he or she wants to live • Start working on constructive plans for the future • Demonstrate adherence with any medication or treatment plan within 2 weeks Patients will: • Identify at least two people he or she can call for support and emotional guidance when he or she is feeling self-destructive before discharge • Show willingness to work on a medical/treatment plan that is congruent with their cultural values and future goals. Assessment findings/diagnostic cues: • Increased ability to concentrate • Processes information, and makes appropriate decisions • Increased ability to problem solve • Increased ability to meet role expectations Patient will: • Demonstrate an increased ability to make appropriate decisions when planning with nurse or clinician by (date) • Identify negative thoughts and rationally counter them and/or reframe them in a positive manner within 2 weeks • Show improved mood as demonstrated by a standard depression rating scale (e.g., Hamilton Rating Scale for Depression in Appendix D-3). Patient will: • Identify two goals he or she wants to achieve from treatment, with aid of nursing intervention, within 1 to 2 days • Discuss with nurse two irrational thoughts about self and others by the end of the first day • Reframe three irrational thoughts with nurse/practitioner by (date)
Depressive Disorders
OVERVIEW
Major Depressive Disorder
Persistent Depressive Disorder (Dysthymia)
ASSESSMENT
Presenting Signs and Symptoms
Assessment Tools
Assessment Guidelines
Depression
NURSING DIAGNOSES WITH INTERVENTIONS
Discussion of Potential Nursing Diagnoses
Signs and Symptoms
Potential Nursing Diagnoses
Previous suicide attempts, putting affairs in order, giving away prized possessions, suicidal ideation (has a plan and the ability to carry it out), makes overt or covert statements regarding killing self, feelings of worthlessness, hopelessness, helplessness
Risk for Self-Directed Violence
Risk for Self-Mutilation
Risk for Suicide
Difficulty with simple tasks, inability to function at previous level, poor problem solving, poor cognitive functioning, verbalizations of inability to cope
Ineffective Coping
Interrupted Family Processes
Risk for Impaired Parenting
Ineffective Role Performance
Difficulty making decisions, poor concentration, inability to take action
Decisional Conflict
Feelings of helplessness, hopelessness, powerlessness
Hopelessness
Powerlessness
Questions meaning of life, own existence; unable to participate in usual religious practices, conflict over spiritual beliefs, anger toward spiritual deity or religious representatives
Spiritual Distress
Impaired Religiosity
Feelings of worthlessness, poor self-image, negative sense of self, self-negating verbalizations, feels like a failure, expressions of shame or guilt, hypersensitive to slights or criticism
Chronic Low Self-Esteem
Situational Low Self-Esteem
Withdrawn, uncommunicative, speaks only in monosyllables, shies away from contact with others
Impaired Social Interaction
Social Isolation
Risk for Loneliness
Vegetative signs of depression: changes in sleep, eating, grooming and hygiene, elimination, and sexual patterns
Self-Care Deficit (bathing/hygiene, dressing/grooming, feeding, toileting)
Imbalanced Nutrition
Disturbed Sleep Pattern
Constipation
Sexual Dysfunction
Overall Guidelines for Nursing Interventions
Depression
Selected Nursing Diagnoses and Nursing Care Plans
Risk Factors (Related To)
 Emotional problems (hopelessness, despair, increased anxiety, panic, anger, hostility)
Emotional problems (hopelessness, despair, increased anxiety, panic, anger, hostility)
 Physical health problems (e.g., somatic symptom disorder, chronic or terminal illness)
Physical health problems (e.g., somatic symptom disorder, chronic or terminal illness)
 Behavioral cues (e.g., giving away personal items, making a will, taking out a large life insurance policy, writing forlorn love notes)
Behavioral cues (e.g., giving away personal items, making a will, taking out a large life insurance policy, writing forlorn love notes)
 History of multiple suicide attempts
History of multiple suicide attempts
 Verbal clues (e.g., talking about death, saying “People would be better off without me”)
Verbal clues (e.g., talking about death, saying “People would be better off without me”)
 Mental health problems (severe depression, psychosis, severe personality disorder, eating disorder, addictions)
Mental health problems (severe depression, psychosis, severe personality disorder, eating disorder, addictions)
 Lack of social resources (e.g., poor rapport, socially isolated, unresponsive family)
Lack of social resources (e.g., poor rapport, socially isolated, unresponsive family)
 Suicide plan, suicidal ideation
Suicide plan, suicidal ideation
 Lack of personal resources (e.g., for achievement, poor insight, affect unavailable and poorly controlled)
Lack of personal resources (e.g., for achievement, poor insight, affect unavailable and poorly controlled)
 History of multiple suicide attempts
History of multiple suicide attempts
 Conflictual interpersonal relationships
Conflictual interpersonal relationships
Outcome Criteria
Long-Term Goals
Short-Term Goals
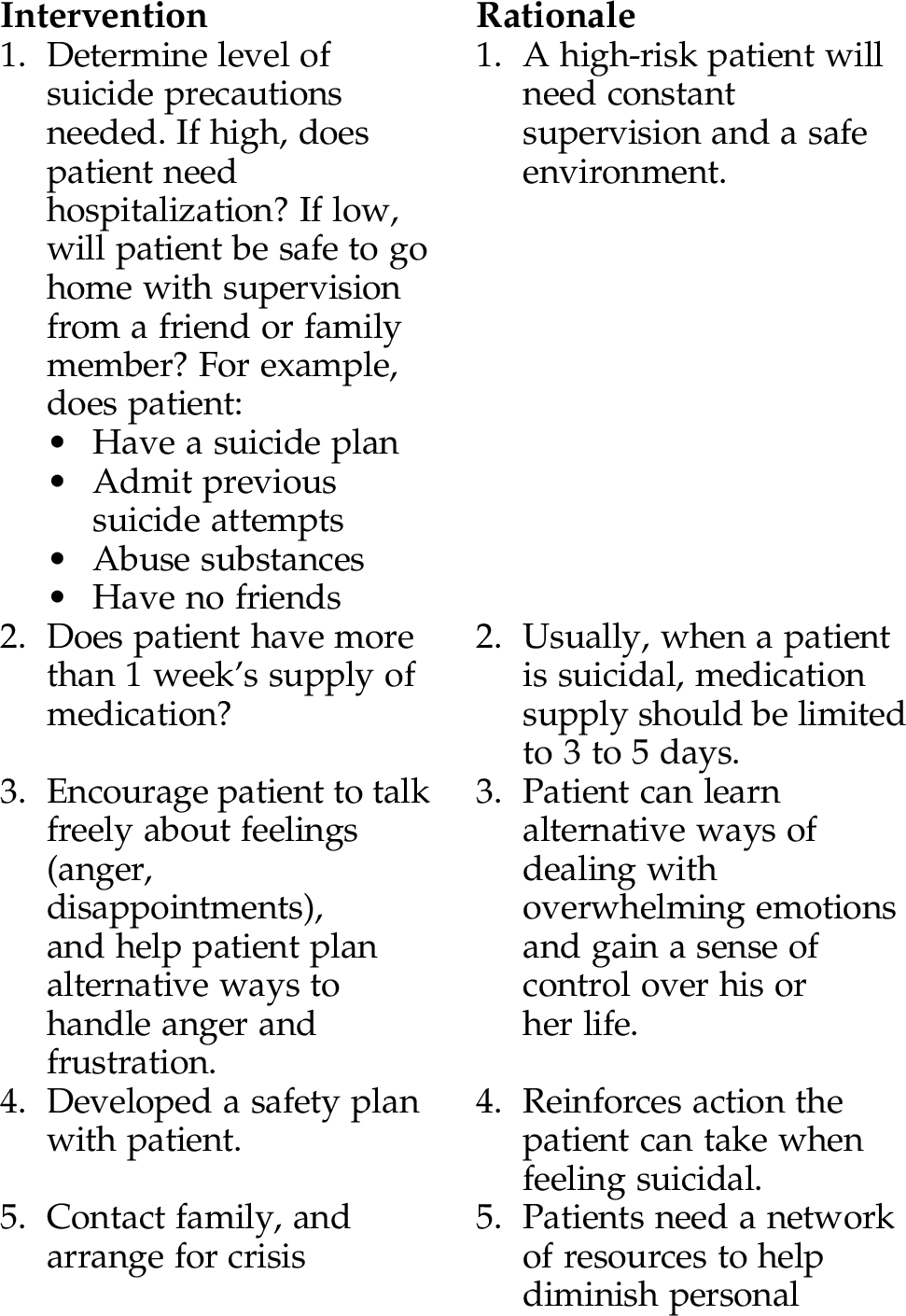
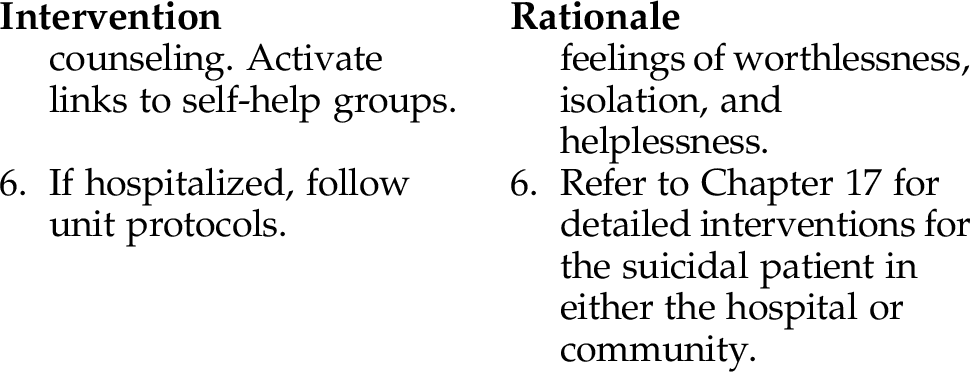
INTERVENTIONS AND RATIONALES
Some Related Factors (Related To)
 Disturbance in pattern of tension release
Disturbance in pattern of tension release
 Inadequate opportunity to prepare for stressor
Inadequate opportunity to prepare for stressor
 Inadequate resources available
Inadequate resources available
 Inadequate social support created by characteristics of the relationship
Inadequate social support created by characteristics of the relationship
 Inability to conserve adaptive energies
Inability to conserve adaptive energies
 Biochemical/neurophysical imbalances
Biochemical/neurophysical imbalances
 Overwhelming life circumstances
Overwhelming life circumstances
 Pathological fatigue, lack of motivation
Pathological fatigue, lack of motivation
Some Defining Characteristics (As Evidenced By)
 decreased use of social supports
decreased use of social supports
 Difficulty organizing information
Difficulty organizing information
 Inability to meet role expectations
Inability to meet role expectations
 Lack of goal-directed behavior
Lack of goal-directed behavior
 Severe anxiety or depressed mood
Severe anxiety or depressed mood
 Persistent feelings of extreme anxiety, guilt, or fear
Persistent feelings of extreme anxiety, guilt, or fear
Outcome Criteria
Long-Term Goals
Short-Term Goals
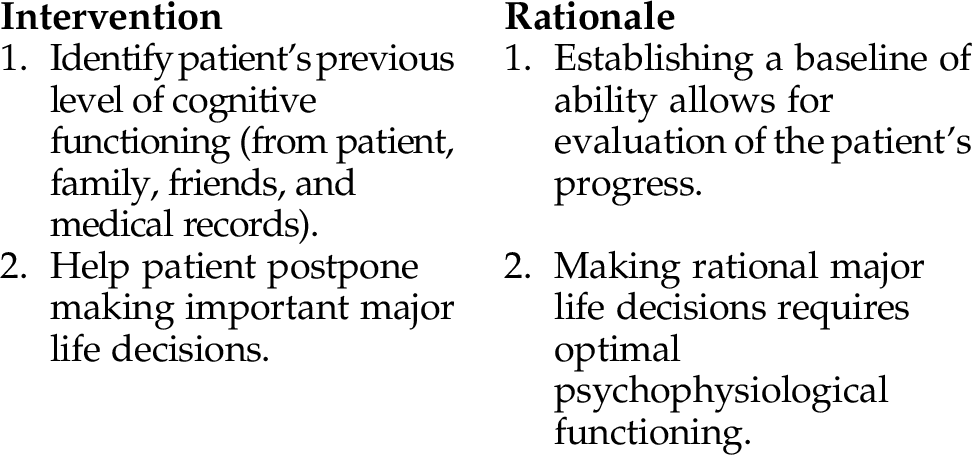
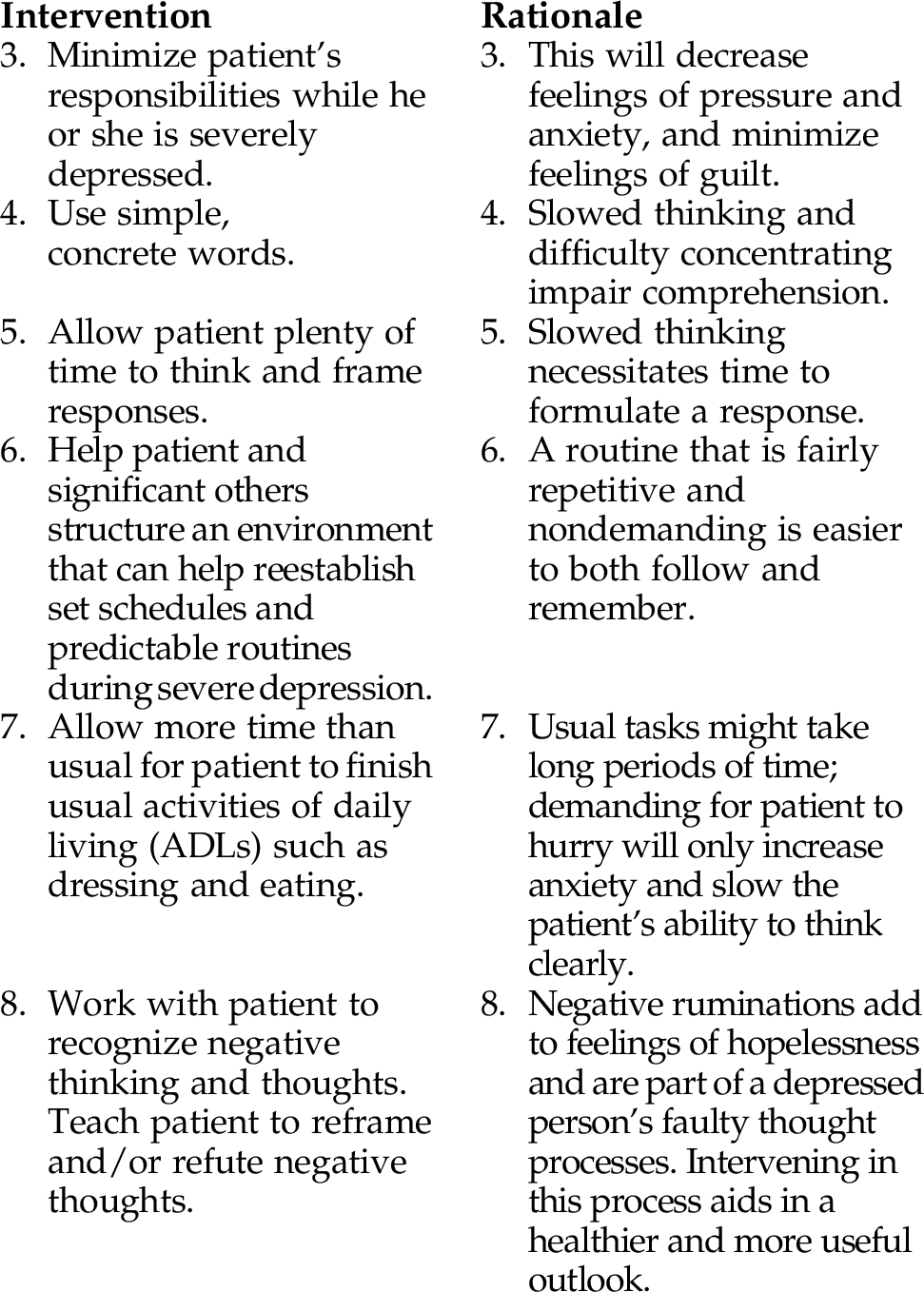
INTERVENTIONS AND RATIONALES
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree